Biology of Aging: Cardiovascular, Respiratory and Urinary Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1535190852 9 Medical Terminology Urinary.Pdf
Syrian Private University Medical Faculty Medical Terminology M.A.Kubtan , MD – FRCS Lecture 9 M.A.Kubtan Objectives After studying this chapter, you will be able to: •Name the parts of the urinary system and discuss the function of each part •Define combining forms used in building words that relate to the urinary system •Identify the meaning of related abbreviations •Name the common diagnoses, clinical procedures, and laboratory tests used in treating disorders of the urinary system M.A.Kubtan 2 Objectives Part 2 •List and define the major pathological conditions of the urinary system •Explain the meaning of surgical terms related to the urinary system •Recognize common pharmacological agents used in treating the urinary system M.A.Kubtan 3 Structure and Function The Urinary System Bladder Kidneys •Also called the excretory system •Maintains water Urinary System balance •Removes waste products from the Urethra Ureters blood by excreting them in the urine Meatus M.A.Kubtan 4 Kidneys Kidneys The kidneys are bean-shaped organs located in the retroperitoneal portion of the abdominal cavity on either side of the vertebral column. Two Primary Functions •To form urine for excretion •To retain essential substances the body needs in the process called reabsorption M.A.Kubtan 5 Parts of the Kidney Kidneys filter about 1700 kidney liters of blood daily in the average adult. medulla Parts of the kidneys •Cortex hilum -outer protective portion •Medulla -inner soft portion •Hilum -a depression located in the middle of the concave side of the kidney where blood vessels, nerves, and the ureters enter and cortex exit the kidneys M.A.Kubtan 6 Urine Production Urine is produced by filtration of: •water •sugar •creatine •salts •urea •uric acid Each kidney contains more than 1 million nephrons which are the functional units of the kidneys. -

Anatomy and Physiology Male Reproductive System References
DEWI PUSPITA ANATOMY AND PHYSIOLOGY MALE REPRODUCTIVE SYSTEM REFERENCES . Tortora and Derrickson, 2006, Principles of Anatomy and Physiology, 11th edition, John Wiley and Sons Inc. Medical Embryology Langeman, pdf. Moore and Persaud, The Developing Human (clinically oriented Embryologi), 8th edition, Saunders, Elsevier, . Van de Graff, Human anatomy, 6th ed, Mcgraw Hill, 2001,pdf . Van de Graff& Rhees,Shaum_s outline of human anatomy and physiology, Mcgraw Hill, 2001, pdf. WHAT IS REPRODUCTION SYSTEM? . Unlike other body systems, the reproductive system is not essential for the survival of the individual; it is, however, required for the survival of the species. The RS does not become functional until it is “turned on” at puberty by the actions of sex hormones sets the reproductive system apart. The male and female reproductive systems complement each other in their common purpose of producing offspring. THE TOPIC : . 1. Gamet Formation . 2. Primary and Secondary sex organ . 3. Male Reproductive system . 4. Female Reproductive system . 5. Female Hormonal Cycle GAMET FORMATION . Gamet or sex cells are the functional reproductive cells . Contain of haploid (23 chromosomes-single) . Fertilizationdiploid (23 paired chromosomes) . One out of the 23 pairs chromosomes is the determine sex sex chromosome X or Y . XXfemale, XYmale Gametogenesis Oocytes Gameto Spermatozoa genesis XY XX XX/XY MALE OR FEMALE....? Male Reproductive system . Introduction to the Male Reproductive System . Scrotum . Testes . Spermatic Ducts, Accessory Reproductive Glands,and the Urethra . Penis . Mechanisms of Erection, Emission, and Ejaculation The urogenital system . Functionally the urogenital system can be divided into two entirely different components: the urinary system and the genital system. -

Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
![The Genitourinary System (And] Instructor's Guide: the Genitourinary System](https://docslib.b-cdn.net/cover/6525/the-genitourinary-system-and-instructors-guide-the-genitourinary-system-1156525.webp)
The Genitourinary System (And] Instructor's Guide: the Genitourinary System
DOCUMENT RESUME ED 213 968 CE 031 777 TITLE The Genitourinary System (and] Instructor's Guide: The Genitourinary System. Health Occupations Education Module: Instructional Materials in Anatomy and Physiology for Pennsylvania Health Occupations Programs. INSTITUTION National Evaluation Systems, Inc., Amherst, Mass. SPONS AGENCY Pennsylvania State Dept. of Education, Harrisburg. Bureau of Vocational and Technical Education. PUB DATE atm 80 NOTE 33p.; For related documents see listing in note of CE 031 758. EDRS PRICE MF01/PCO2 Plus Postage. DESCRIPTORS ' *Allied Health Occupations Education; *Anatomy; Behaviorpl Objectives; *Individualized Instruction; *Learning Activities; Learning Modules; *Males; Medical Vocabulary; *Physiology; Postsecondary Education; Pretests Posttests; Programed Instructional Materials; Secondary Education; Self Evaluation (Individuals); Teaching Methods IDENTIFIERS *Genitourinary System; Pennsylvania ABSTRACT This module on the genitourinary system is one of 17 modules designed for individualized instruction in health occupations education programs at both the secondary and postsecondary levels. It is part of an eight-unit miniseries on anatomy, and physiology within the series of 17 modules. Following a preface which explains to the student how to use the module, the unit consists of a pretest with answers, three sections (information sheets) with their objectives (e.g., identify and describe the location and anatomical structure of the kidneys), optional activities (e.g., research the process of _____dialysi-sby an artificial kidney machine), and posttests, and a glossary of terms. Topics covered in the unit are introduction to the genitourinary system, the urinary system, and the male reproductive system. An accompanying instructor's guide Contains suggestions for using the module and answers to the posttest. (KC) *********************************************************************** * Reproductions supplied by EDRS are the best that can be made * * from the original document. -

The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -

Laboratory 8 - Urinary and Reproductive Systems
Laboratory 8 - Urinary and Reproductive Systems Urinary System Please read before starting: It is easy to damage the structures of the reproductive system as you expose structures associated with excretion, so exercise caution as you do this. Please also note that we will have drawings available as well to help you find and identify the structures described below. The major blood vessels serving the kidneys are the Renal renal artery and the renal pyramid vein., which are located deep in the parietal peritoneum. The renal artery is a branch of the dorsal aorta that comes off Renal further caudal than the cranial pelvis mesenteric artery. Dissect the left kidney in situ, dividing it into dorsal and ventral portions by making a frontal section along the outer periphery. Observe the renal cortex renal medulla (next layer in) renal pyramids renal pelvis ureter (see above diagram) The kidneys include a variety of structures including an arterial supply, a venous return, extensive capillary networks around each nephron and then, of course, the filtration and reabsorption apparatus. These structures are primarily composed of nephrons (the basic functional unit of the kidney) and the ducts which carry urine away from the nephron (the collecting ducts and larger ducts eventually draining these into the ureters from each kidney. The renal pyramids contain the extensions of the nephrons into the renal medulla (the Loops of Henle) and the collecting ducts. Urine is eventually emptied into the renal pelvis before leaving the kidneys in the ureters. The ureters leaves the kidneys medially at approximately the midpoint of the organs and then run caudal to the urinary bladder. -

Urinary System
Urinary system Sándor Katz M.D.,Ph.D. Urinary system - constituents • kidneys • ureters • urinary bladder • urethra Kidney Weight: 130-140g Kidneys - location 1. On the posterior body wall 2. Posterior to parietal peritoneum – retroperitoneal organ 3. At the level of T12-L2 (left kidney) and L1-L3 (right kidney) Kidneys - location Kidneys – covering structures 1. Renal (Gerota’s) fascia 2. Adipose capsule 3. Fibrous capsule Kidneys - neighbouring organs and structures Kidney – gross anatomy External structures: Hilum of kidney: 1. Renal vein 2. Renal artery 3. Ureter Internal structures: 1. Cortex 2. Medulla 3. Minor calyces 4. Major calyces 5. Renal pelvis Renal cortex Renal columns (Bertini’s columns) Renal medulla – renal pyramids A p p r o x i m a t e l y 3 0 pyramids are in each kidney and many of them are fused together. renal papilla Minor calyces 8-9 in each kidney Major calyces Approx. 3 in each kidney Renal pelvis Renal hilum - L1/L2 level renal sinus From anterior to posterior direction: 1. renal vein 2. renal artery 3. ureter From superior to inferior direction: 1. renal artery 2. renal vein 3. ureter Renal arteries - L1 level Renal artery • segmental arteries • interlobar arteries • arcuate arteries • interlobular arteries • afferent arterioles Renal veins left renal vein is longer than the right one and crosses over the aorta Renal veins right renal vein left renal vein is longer than the right one and crosses over the aorta left renal vein Tributaries of the renal veins • (stellate veins – only under the fibrous capsule) • interlobular veins • arcuate veins • interlobar veins • segmental veins Renal veins left suprarenal vein (empties into the left renal vein) left gonadal (testicular or ovarian) vein (empties into the left renal vein) The right suprarenal and gonadal veins empty into the IVC. -

Structures of Urinary System
Bio217 F2014 Unit 8 Bio217: Pathophysiology Class Notes Kidneys (2) Professor Linda Falkow ◦ Retroperitoneal ◦ Renal capsule Unit VIII: Urinary (Renal) System Disorders ◦ Adipose capsule and ◦ Renal fascia Reproductive System Disorders ◦ Hilum Ureters (2) Urinary Bladder (1) Chapter 28: Structure & Function of Renal & Urologic Systems Urethra (1) Chapter 29: Alterations of Renal & Urinary Tract Function Chapter 31: Structure and Function of Reproductive Systems Chapter 32: Alterations of the Reproductive Systems Structures of Urinary System • 1.2 million nephrons per kidney • Functional unit of the kidney • Cortex – Cortical nephrons • Medulla – Juxtamedullary nephrons • Pyramids • Parts of nephron • Calyces – Renal corpuscle (=_______________________________) – Minor and major – Renal tubules • Proximal tubule (pct) • Renal pelvis • Loop of Henle Structures of the Kidney • Distal tubule (dct)Nephron • Glomerular filtration membrane –Blood passes through the three layers and forms the filtrate Nephron Nephron 1 Bio217 F2014 Unit 8 • Juxtaglomerular apparatus – Juxtaglomerular cells ( renin) – Macula densa (sense changes in Na+) – Renin-angiotensin pathway: ___________ • Decr. blood vol. or decr. Na+ incr. renin Angiotensin I Angiotensin II aldosterone (incr. reabsorption of Na+ and H2O) Nephron Juxtaglomerular Apparatus • Urinary Bladder – Detrusor muscle – Trigone – Micturition reflex • Urethra – Internal and external sphincters – 3 to 4 cm in females – 18 to 20 cm in males Structures of Urinary System Urinary Bladder and Urethra -

Excretory System
Excretory System Excretory System • Functions • Removes wastes from blood • Removes harmful substances from blood • Regulates body fluids • Maintains homeostasis • Main Parts • Kidneys • Urinary bladder • Large intestine • Lungs • Skin Urinary System: • Not all the waste products that leave the body are solid. • Most liquid wastes formed by the body are excreted by the urinary system. Bladder • Muscular sac in the pelvis • Urine is made in the kidneys and travels down two tubes called ureters to the bladder • Urine exits the bladder into the urethra, which carries out of the body Large Intestine: • The undigested material not absorbed by the large intestine forms a semi- solid waste product known as feces. These solid wastes are removed by the body through the rectum. Kidneys: • The main organs of the urinary system • Bean-shaped organs in your abdomen that filter blood and remove waste. • The wastewater, or urine, that has been filtered out of the blood moves into the ureters, tubes that connect the kidneys to the bladder. • The bladder is a muscular sac that holds urine until it exits the body through the urethra. The Lungs: • The lungs are another part of the excretory system. • Lungs are part of the respiratory system, also. • Wastes removed by the lungs include carbon dioxide and water vapor produced by cellular respiration. The Skin • The skin also functions in excretion. • Sweat glands in the skin produce perspiration. • When a person perspires, the skin excretes water and salts. Working Together Works with the circulatory system in transporting blood through kidneys. Urea, uric acid, and water are removed from the blood and most of the water is put back in the system. -
Day 6 Urogenital System
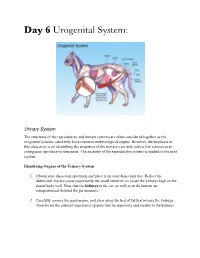
Day 6 Urogenital System: Urinary System The structures of the reproductive and urinary systems are often considered together as the urogenital systems, since they have common embryological origins. However, the emphasis in this dissection is on identifying the structures of the urinary tract with only a few references to contiguous reproductive structures. The anatomy of the reproductive system is studied in the next section. Identifying Organs of the Urinary System 1. Obtain your dissection specimen and place it on your dissection tray. Reflect the abdominal viscera (most importantly the small intestine) to locate the kidneys high on the dorsal body wall. Note that the kidneys in the cat, as well as in the human are retroperitoneal (behind the peritoneum). 2. Carefully remove the peritoneum, and clear away the bed of fat that invests the kidneys. Then locate the adrenal (suprarenal) glands that lie superiorly and medial to the kidneys. 3. Identify the renal artery (red latex injected), the renal vein (blue latex injected), and the ureter at the hilus region of the kidney. (You may find two renal veins leaving one kidney in the cat but not in humans). 4. Trace the ureters to the urinary bladder, a smooth muscular sac located superiorly to the small intestine. If your cat is a female, be careful not to confuse the ureters with the urine tubes, which lie superior to the bladder in the same general region. See Figure D8.1. Observe the sites where the ureters enter the bladder. How would you describe the entrance point anatomically? 5. Cut through the bladder wall, and examine the region of the uretheral exit to see if you can discern any evidence of the internal sphincter. -

Medical Terminology
MEDICAL TERMINOLOGY THE URINARY SYSTEM MATCHING EXERCISES KEY ANATOMICAL TERMS 1. urethral meatus f. opening in urethra to outside of body 2. creatinine d. waste product of muscle metabolism excreted in urine 3. ureter e. tube carrying urine from kidney to bladder 4. urethra i. canal carrying urine to outside of body 5. nephron c. microscopic functional unit capable of forming urine 6. hilum j. indented opening in kidney for incoming and exiting vessels 7. renal cortex a. outer part of kidney 8. urea h. waste product from liver excreted in urine 9. renal medulla b. inner part of kidney 10. calyces g. system of ducts carrying urine from nephrons to renal pelvis 1. principal organs of urinary system g. kidneys 2. microscopic ball of capillaries at top of j. glomerulus nephron 3. basin-like portion of ureter within kidney h renal pelvis 4. outer part of kidney i. renal cortex 5. pale yellow liquid waste (95% water) a. urine 6. strong fibrous tissue holding kidneys in place b. renal fascia 7. inner part of kidney d. renal medulla 8. vessel carrying blood to c. afferent arteriole glomerulus 9. stem portion of nephron e. renal tubule 10. vessel carrying blood from glomerulus f. efferent arteriole SYMPTOMATIC AND DIAGNOSTIC TERMS 1. hematuria e. blood in urine 2. pyelonephrosis d. abnormal condition of renal pelvis 3. ureterolithiasis c. development of a calculus in urinary kidney to bladder tube 4. urethrodynia f. pain in canal carrying urine to outside of body 5. polydipsia b. excessive thirst 6. glycosuria a. sugar in urine 1.