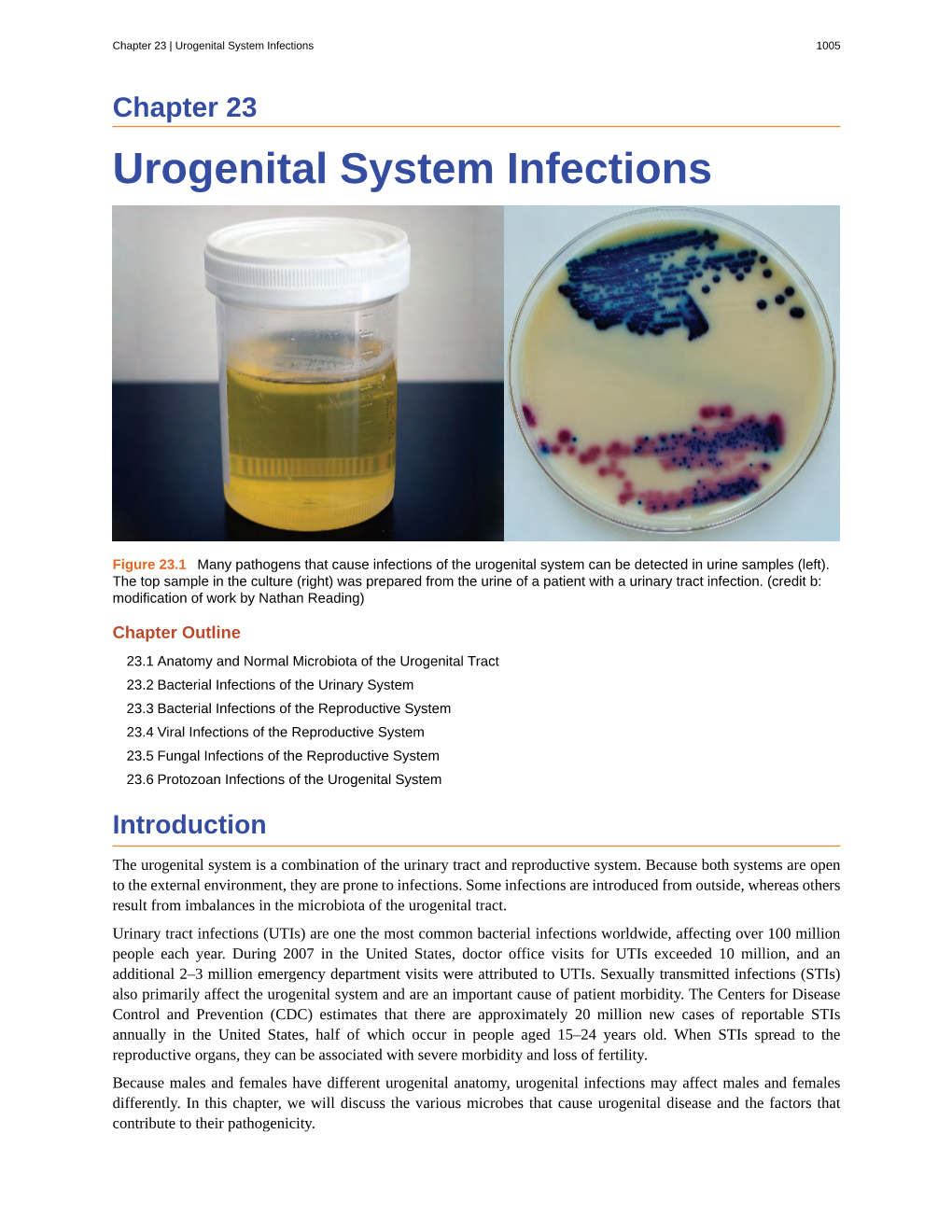
Urogenital System Infections 1005
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

CSI Study Guide-Female and Male Exams
Guide for Skill Station Female & Male Exams 2019 1. Overview Students will have the opportunity to perform female and male GU exams using both mannequins and standardized patients. The female standardized patient GU exam will include the external genitalia and pelvic exam, including use of a speculum; Male GU exam will include hernia and external genitalia/testicular examination. Practice session using mannequin will include evaluation of the prostate. Also refer to the Female and Male Exam – Factsheet 2019 for additional simulation lab session instructions 2. Goal of the Procedure Accurately perform female and male GU exams using proper techniques and logical sequence, while providing for patient comfort and modesty. 3. Reference(s) Jarvis, C. (2016). Physical Examination and Health Assessment. (7th ed.). Philadelphia: Elsevier. 4. Required Reading / Review Begin by reviewing the materials from 609a Health Assessment: a. Panoptos: Week 11 Male Genitourinary System: Anus, Rectum, Prostate: Male Genital Exam Week 12 Female Genital exam b. Jarvis, C. (2016). Physical Examination and Health Assessment. Pocket Guide (7th ed.). Philadelphia: Elsevier. Use above link, then use your UA Net ID Credentials to sign into the library, then click view full text, navigate to below chapters • Chapter 17 Male Genitourinary System pp 225-236; 12 pages • Chapter 18 Female Genitourinary System pp 237-252; 16 pages • Chapter 19 Anus, Rectum, and Prostate pp 253-260; 8 pages 5. Required Procedure Competencies Professionalism 1. Present/on time 2. Prepared (readings, etc.) 3. Engaged and participated 4. Respectful of others Communication skills 1. Obtain name and age of the patient and relationship of others if present 2. -

The Cyclist's Vulva
The Cyclist’s Vulva Dr. Chimsom T. Oleka, MD FACOG Board Certified OBGYN Fellowship Trained Pediatric and Adolescent Gynecologist National Medical Network –USOPC Houston, TX DEPARTMENT NAME DISCLOSURES None [email protected] DEPARTMENT NAME PRONOUNS The use of “female” and “woman” in this talk, as well as in the highlighted studies refer to cis gender females with vulvas DEPARTMENT NAME GOALS To highlight an issue To discuss why this issue matters To inspire future research and exploration To normalize the conversation DEPARTMENT NAME The consensus is that when you first start cycling on your good‐as‐new, unbruised foof, it is going to hurt. After a “breaking‐in” period, the pain‐to‐numbness ratio becomes favourable. As long as you protect against infection, wear padded shorts with a generous layer of chamois cream, no underwear and make regular offerings to the ingrown hair goddess, things are manageable. This is wrong. Hannah Dines British T2 trike rider who competed at the 2016 Summer Paralympics DEPARTMENT NAME MY INTRODUCTION TO CYCLING Childhood Adolescence Adult Life DEPARTMENT NAME THE CYCLIST’S VULVA The Issue Vulva Anatomy Vulva Trauma Prevention DEPARTMENT NAME CYCLING HAS POSITIVE BENEFITS Popular Means of Exercise Has gained popularity among Ideal nonimpact women in the past aerobic exercise decade Increases Lowers all cause cardiorespiratory mortality risks fitness DEPARTMENT NAME Hermans TJN, Wijn RPWF, Winkens B, et al. Urogenital and Sexual complaints in female club cyclists‐a cross‐sectional study. J Sex Med 2016 CYCLING ALSO PREDISPOSES TO VULVAR TRAUMA • Significant decreases in pudendal nerve sensory function in women cyclists • Similar to men, women cyclists suffer from compression injuries that compromise normal function of the main neurovascular bundle of the vulva • Buller et al. -

Pregnancy and Cesarean Delivery After Multimodal Therapy for Vulvar Carcinoma: a Case Report
MOLECULAR AND CLINICAL ONCOLOGY 5: 583-586, 2016 Pregnancy and cesarean delivery after multimodal therapy for vulvar carcinoma: A case report KUNIAKI TORIYABE1,2, HARUKI TANIGUCHI2, TOKIHIRO SENDA2,3, MASAKO NAKANO2, YOSHINARI KOBAYASHI2, MIHO IZAWA2, HIROHIKO TANAKA2, TETSUO ASAKURA2, TSUTOMU TABATA1 and TOMOAKI IKEDA1 1Department of Obstetrics and Gynecology, Mie University Graduate School of Medicine, Tsu, Mie 514-8507; 2Department of Obstetrics and Gynecology, Mie Prefectural General Medical Center, Yokkaichi, Mie 510-8561; 3Department of Obstetrics and Gynecology, Kinan Hospital, Mihama, Mie 519-5293, Japan Received November 4, 2015; Accepted September 12, 2016 DOI: 10.3892/mco.2016.1021 Abstract. Reports of pregnancy following treatment for vulvectomy, may have an increased incidence of caesarean vulvar carcinoma are extremely uncommon, as the main delivery (2). In the literature, vulvar scarring following radical problem of subsequent pregnancy is vulvar scarring following vulvectomy was the major reason for pregnant women under- radical surgery. We herein report the case of a patient who was going caesarean section (2-7). To date, no cases of pregnancy diagnosed with stage I squamous cell carcinoma of the vulva following vulvar carcinoma have been reported in patients at the age of 17 years and was treated with multimodal therapy, who had undergone surgery and radiotherapy. including neoadjuvant chemotherapy, wide local excision with We herein describe a case in which caesarean section was bilateral inguinal lymph node dissection and adjuvant radio- performed due to the presence of extensive vulvar scarring therapy. The patient became pregnant spontaneously 9 years following multimodal therapy for vulvar carcinoma, including after her initial diagnosis and the antenatal course was good, chemotherapy, surgery and radiotherapy. -

Table of Contents
viii Contents Chapter 1. Taking the Certification Examination . 1 General Suggestions for Preparing for the Exam About the Certification Exams Chapter 2. Developmental and Behavioral Sciences . 11 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Paula Chiplis, PhD, RN, CPNP Psychosocial, Cognitive, and Ethical-Moral Development Behavior Modification Physical Development: Normal Growth Expectations and Developmental Milestones Family Concepts and Issues Family-Centered Care Cultural and Spiritual Diversity Chapter 3. Communication . 23 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Culturally Sensitive Communication Components of Therapeutic Communication Communication Barriers Modes of Communication Patient Confidentiality Written Communication in Nursing Practice Professional Communication Advocacy Chapter 4. The Nursing Process . 33 Clara J. Richardson, MSN, RN–BC Nursing Assessment Nursing Diagnosis and Treatment Chapter 5. Basic and Applied Sciences . 49 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Paula Chiplis, PhD, RN, CPNP Trauma and Diseases Processes Common Genetic Disorders Common Childhood Diseases Traction Pharmacology Nutrition Chemistry Clinical Signs Associated With Isotonic Dehydration in Infants ix Chapter 6. Educational Principles and Strategies . 69 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Patient Education Chapter 7. Life Situations and Adaptive and Maladaptive Responses . 75 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Palliative Care End-of-Life Care Response to Crisis Chapter 8. Sensory Disorders . 87 Clara J. Richardson, MSN, RN–BC Developmental Characteristics of the Pediatric Sensory System Hearing Disorders Vision Disorders Conjunctivitis Otitis Media and Otitis Externa Retinoblastoma Trauma to the Eye Chapter 9. -

GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M Anual
13 Male Reproductive System Disorders Vaunette Fay, PhD, RN, FNP-BC, GNP-BC GERIATRIC APPRoACH Normal Changes of Aging Male Reproductive System • Decreased testosterone level leads to increased estrogen-to-androgen ratio • Testicular atrophy • Decreased sperm motility; fertility reduced but extant • Increased incidence of gynecomastia Sexual function • Slowed arousal—increased time to achieve erection • Erection less firm, shorter lasting • Delayed ejaculation and decreased forcefulness at ejaculation • Longer interval to achieving subsequent erection Prostate • By fourth decade of life, stromal fibrous elements and glandular tissue hypertrophy, stimulated by dihydrotestosterone (DHT, the active androgen within the prostate); hyperplastic nodules enlarge in size, ultimately leading to urethral obstruction 398 GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M anual Clinical Implications History • Many men are overly sensitive about complaints of the male genitourinary system; men are often not inclined to initiate discussion, seek help; important to take active role in screening with an approach that is open, trustworthy, and nonjudgmental • Sexual function remains important to many men, even at ages over 80 • Lack of an available partner, poor health, erectile dysfunction, medication adverse effects, and lack of desire are the main reasons men do not continue to have sex • Acute and chronic alcohol use can lead to impotence in men • Nocturia is reported in 66% of patients over 65 – Due to impaired ability to concentrate urine, reduced -
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Urologic Disorders
Urologic Disorders Abdulaziz Althunayan Consultant Urologist Assistant professor of Surgery Urologic Disorders Urinary tract infections Urolithiasis Benign Prostatic Hyperplasia and voiding dysfunction Urinary tract infections Urethritis Acute Pyelonephritis Epididymitis/orchitis Chronic Pyelonephritis Prostatitis Renal Abscess cystitis URETHRITIS S&S – urethral discharge – burning on urination – Asymptomatic Gonococcal vs. Nongonococcal DX: – incubation period(3-10 days vs. 1-5 wks) – Urethral swab – Serum: Chlamydia-specific ribosomal RNA URETHRITIS Epididymitis Acute : pain, swelling, of the epididymis <6wk chronic :long-standing pain in the epididymis and testicle, usu. no swelling. DX – Epididymitis vs. Torsion – U/S – Testicular scan – Younger : N. gonorrhoeae or C. trachomatis – Older : E. coli Epididymitis Prostatitis Syndrome that presents with inflammation± infection of the prostate gland including: – Dysuria, frequency – dysfunctional voiding – Perineal pain – Painful ejaculation Prostatitis Prostatitis Acute Bacterial Prostatitis : – Rare – Acute pain – Storage and voiding urinary symptoms – Fever, chills, malaise, N/V – Perineal and suprapubic pain – Tender swollen hot prostate. – Rx : Abx and urinary drainage cystitis S&S: – dysuria, frequency, urgency, voiding of small urine volumes, – Suprapubic /lower abdominal pain – ± Hematuria – DX: dip-stick urinalysis Urine culture Pyelonephritis Inflammation of the kidney and renal pelvis S&S : – Chills – Fever – Costovertebral angle tenderness (flank Pain) – GI:abdo pain, N/V, and -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Non-Certified Epididymitis DST.Pdf
Clinical Prevention Services Provincial STI Services 655 West 12th Avenue Vancouver, BC V5Z 4R4 Tel : 604.707.5600 Fax: 604.707.5604 www.bccdc.ca BCCDC Non-certified Practice Decision Support Tool Epididymitis EPIDIDYMITIS Testicular torsion is a surgical emergency and requires immediate consultation. It can mimic epididymitis and must be considered in all people presenting with sudden onset, severe testicular pain. Males less than 20 years are more likely to be diagnosed with testicular torsion, but it can occur at any age. Viability of the testis can be compromised as soon as 6-12 hours after the onset of sudden and severe testicular pain. SCOPE RNs must consult with or refer all suspect cases of epididymitis to a physician (MD) or nurse practitioner (NP) for clinical evaluation and a client-specific order for empiric treatment. ETIOLOGY Epididymitis is inflammation of the epididymis, with bacterial and non-bacterial causes: Bacterial: Chlamydia trachomatis (CT) Neisseria gonorrhoeae (GC) coliforms (e.g., E.coli) Non-bacterial: urologic conditions trauma (e.g., surgery) autoimmune conditions, mumps and cancer (not as common) EPIDEMIOLOGY Risk Factors STI-related: condomless insertive anal sex recent CT/GC infection or UTI BCCDC Clinical Prevention Services Reproductive Health Decision Support Tool – Non-certified Practice 1 Epididymitis 2020 BCCDC Non-certified Practice Decision Support Tool Epididymitis Other considerations: recent urinary tract instrumentation or surgery obstructive anatomic abnormalities (e.g., benign prostatic