Strategies to Overcome Bypass Mechanisms Mediating Clinical
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nimotuzumab, an Antitumor Antibody That Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding While Permitting the Active Receptor Conformation
Published OnlineFirst July 7, 2009; DOI: 10.1158/0008-5472.CAN-08-4518 Experimental Therapeutics, Molecular Targets, and Chemical Biology Nimotuzumab, an Antitumor Antibody that Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding while Permitting the Active Receptor Conformation Ariel Talavera,1,2 Rosmarie Friemann,2,3 Silvia Go´mez-Puerta,1 Carlos Martinez-Fleites,4 Greta Garrido,1 Ailem Rabasa,1 Alejandro Lo´pez-Requena,1 Amaury Pupo,1 Rune F. Johansen,3 Oliberto Sa´nchez,5 Ute Krengel,2 and Ernesto Moreno1 1Center of Molecular Immunology, Havana, Cuba; 2Department of Chemistry, University of Oslo, Oslo, Norway; and 3Center for Molecular and Behavioral Neuroscience, Institute of Medical Microbiology, University of Oslo, Rikshospitalet HF, Oslo, Norway; 4Department of Chemistry, University of York, Heslington, York, United Kingdom; and 5Center for Genetic Engineering and Biotechnology, Havana, Cuba Abstract region of the EGFR (eEGFR), leaving the dimerization ‘‘arm’’ in Overexpression of the epidermal growth factor (EGF) receptor domain II ready for binding a second monomer (4, 5). It has been (EGFR) in cancer cells correlates with tumor malignancy and shown that the eEGFR adopts a ‘‘tethered’’ or inactive conformation poor prognosis for cancer patients. For this reason, the EGFR in the absence of EGF (6). In this characteristic conformation, has become one of the main targets of anticancer therapies. the dimerization arm is hidden by interactions with domain IV, Structural data obtained in the last few years have revealed whereas domains I and III remain separated. Thus, to adopt the the molecular mechanism for ligand-induced EGFR dimeriza- ‘‘extended’’ or active conformation observed in the crystal structure tion and subsequent signal transduction, and also how this of the complex with EGF (4), the receptor must undergo a major signal is blocked by either monoclonal antibodies or small conformational change that brings together domains I and III (6). -

Targeted and Novel Therapy in Advanced Gastric Cancer Julie H
Selim et al. Exp Hematol Oncol (2019) 8:25 https://doi.org/10.1186/s40164-019-0149-6 Experimental Hematology & Oncology REVIEW Open Access Targeted and novel therapy in advanced gastric cancer Julie H. Selim1 , Shagufta Shaheen2 , Wei‑Chun Sheu3 and Chung‑Tsen Hsueh4* Abstract The systemic treatment options for advanced gastric cancer (GC) have evolved rapidly in recent years. We have reviewed the recent data of clinical trial incorporating targeted agents, including inhibitors of angiogenesis, human epidermal growth factor receptor 2 (HER2), mesenchymal–epithelial transition, epidermal growth factor receptor, mammalian target of rapamycin, claudin‑18.2, programmed death‑1 and DNA. Addition of trastuzumab to platinum‑ based chemotherapy has become standard of care as front‑line therapy in advanced GC overexpressing HER2. In the second‑line setting, ramucirumab with paclitaxel signifcantly improves overall survival compared to paclitaxel alone. For patients with refractory disease, apatinib, nivolumab, ramucirumab and TAS‑102 have demonstrated single‑agent activity with improved overall survival compared to placebo alone. Pembrolizumab has demonstrated more than 50% response rate in microsatellite instability‑high tumors, 15% response rate in tumors expressing programmed death ligand 1, and non‑inferior outcome in frst‑line treatment compared to chemotherapy. This review summarizes the current state and progress of research on targeted therapy for advanced GC. Keywords: Gastric cancer, Targeted therapy, Human epidermal growth factor receptor 2, Programmed death‑1, Vascular endothelial growth factor receptor 2 Background GC mortality which is consistent with overall decrease in Gastric cancer (GC), including adenocarcinoma of the GC-related deaths [4]. gastroesophageal junction (GEJ) and stomach, is the ffth Tere have been several eforts to perform large-scale most common cancer and the third leading cause of can- molecular profling and classifcation of GC. -
Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -
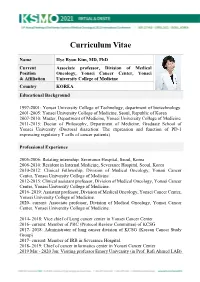
KSMO 2021 CV SS Hye
Curriculum Vitae Name Hye Ryun Kim, MD, PhD Current Associate professor, Division of Medical Position Oncology, Yonsei Cancer Center, Yonsei & Affiliation University College of Medicine Country KOREA Educational Background 1997-2001: Yonsei University College of Technology, department of biotechnology. 2001-2005: Yonsei University College of Medicine, Seoul, Republic of Korea 2007-2010: Master, Department of Medicine, Yonsei University College of Medicine 2011-2015: Doctor of Philosophy, Department of Medicine, Graduate School of Yonsei University (Doctoral dissertion: The expression and function of PD-1 expressing regulatory T cells of cancer patients) Professional Experience 2005-2006: Rotating internship, Severance Hospital, Seoul, Korea 2006-2010: Resident in Internal Medicine, Severance Hospital, Seoul, Korea 2010-2012: Clinical Fellowship, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2012-2015: Clinical assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2016- 2019: Assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2020- current: Associate professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2014- 2018: Vice chief of Lung cancer center in Yonsei Cancer Center 2016- current: Member of PRC (Protocol Review Committee) of KCSG 2017- 2018: Administrator of lung cancer division of KCSG (Korean Cancer Study Group) 2017- current: -

Advances in Epidermal Growth Factor Receptor Specific Immunotherapy: Lessons to Be Learned from Armed Antibodies
www.oncotarget.com Oncotarget, 2020, Vol. 11, (No. 38), pp: 3531-3557 Review Advances in epidermal growth factor receptor specific immunotherapy: lessons to be learned from armed antibodies Fleury Augustin Nsole Biteghe1,*, Neelakshi Mungra2,*, Nyangone Ekome Toung Chalomie4, Jean De La Croix Ndong5, Jean Engohang-Ndong6, Guillaume Vignaux7, Eden Padayachee8, Krupa Naran2,* and Stefan Barth2,3,* 1Department of Radiation Oncology and Biomedical Sciences, Cedars-Sinai Medical, Los Angeles, CA, USA 2Medical Biotechnology & Immunotherapy Research Unit, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 3South African Research Chair in Cancer Biotechnology, Department of Integrative Biomedical Sciences, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 4Sun Yat-Sen University, Zhongshan Medical School, Guangzhou, China 5Department of Orthopedic Surgery, New York University School of Medicine, New York, NY, USA 6Department of Biological Sciences, Kent State University at Tuscarawas, New Philadelphia, OH, USA 7Arctic Slope Regional Corporation Federal, Beltsville, MD, USA 8Department of Physiology, University of Kentucky, Lexington, KY, USA *These authors contributed equally to this work Correspondence to: Stefan Barth, email: [email protected] Keywords: epidermal growth factor receptor (EGFR); recombinant immunotoxins (ITs); targeted human cytolytic fusion proteins (hCFPs); recombinant antibody-drug conjugates (rADCs); recombinant antibody photoimmunoconjugates (rAPCs) Received: May 30, 2020 Accepted: August 11, 2020 Published: September 22, 2020 Copyright: © 2020 Biteghe et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy
cancers Review Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy Laura Boyero 1 , Amparo Sánchez-Gastaldo 2, Miriam Alonso 2, 1 1,2,3, , 1,2, , José Francisco Noguera-Uclés , Sonia Molina-Pinelo * y and Reyes Bernabé-Caro * y 1 Institute of Biomedicine of Seville (IBiS) (HUVR, CSIC, Universidad de Sevilla), 41013 Seville, Spain; [email protected] (L.B.); [email protected] (J.F.N.-U.) 2 Medical Oncology Department, Hospital Universitario Virgen del Rocio, 41013 Seville, Spain; [email protected] (A.S.-G.); [email protected] (M.A.) 3 Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), 28029 Madrid, Spain * Correspondence: [email protected] (S.M.-P.); [email protected] (R.B.-C.) These authors contributed equally to this work. y Received: 16 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Simple Summary: Immuno-oncology has redefined the treatment of lung cancer, with the ultimate goal being the reactivation of the anti-tumor immune response. This has led to the development of several therapeutic strategies focused in this direction. However, a high percentage of lung cancer patients do not respond to these therapies or their responses are transient. Here, we summarized the impact of immunotherapy on lung cancer patients in the latest clinical trials conducted on this disease. As well as the mechanisms of primary and acquired resistance to immunotherapy in this disease. Abstract: After several decades without maintained responses or long-term survival of patients with lung cancer, novel therapies have emerged as a hopeful milestone in this research field. -

Nimotuzumab Inhibits Cholangiocarcinoma Cell
ANTICANCER RESEARCH 37 : 3591-3597 (2017) doi:10.21873/anticanres.11729 Nimotuzumab Inhibits Cholangiocarcinoma Cell Metastasis via Suppression of the Epithelial–Mesenchymal Transition Process SUREERAT PADTHAISONG 1,2 , MALINEE THANEE 1,2,3 , ANCHALEE TECHASEN 2,3,4 , NISANA NAMWAT 1,2,3 , PUANGRAT YONGVANIT 2,3 , AEKKAPHOD LIWATTHAKUN 5, KHITTISAK HANKLA 5, SAKKARN SANGKHAMANON 4,6 and WATCHARIN LOILOME 1,2,3 Departments of 1Biochemistry, 5Surgery, and 6Pathology, Khon Kaen University, Khon Kaen, Thailand; 2Cholangiocarcinoma Research Institute, Faculty of Medicine, 3Cholangiocarcinoma Screening and Care Program (CASCAP) and 4Faculty of Associated Medical Sciences, Khon Kaen University, Khon Kaen, Thailand Abstract. Background/Aim: Changes in epidermal growth liver fluke Opisthorchis viverrini is a major risk factor for factor receptor (EGFR) are commonly found in cancer the development of CCA in this area. CCA is difficult to progression, signaling a poor outcome in patients. In the diagnose at an early stage. Most patients receive treatment present study, we aimed to investigate whether nimotuzumab when the disease becomes advanced, leading to a poor could be of benefit for cholangiocarcinoma (CCA) treatment. prognosis as surgical resection, which is potentially curative Materials and Methods: The expression of EGFR was for early-stage disease, is usually ineffective for advanced or explored using immunohistochemical staining in cases late stages (2, 3). Therefore, new approaches involving divided into groups with low and high expression. The effect targeted therapy are needed. of nimotuzumab on CCA cell growth, metastasis and the We previously reported that the expression of kinase A molecular mechanisms by which nimotuzumab inhibits CCA regulatory subunit I α ( PRKAR1A ) is involved in cell metastasis were evaluated. -

One Target, Different Effects: a Comparison of Distinct Therapeutic Antibodies Against the Same Targets
EXPERIMENTAL and MOLECULAR MEDICINE, Vol. 43, No. 10, 539-549, October 2011 One target, different effects: a comparison of distinct therapeutic antibodies against the same targets Hyunbo Shim ple, four antibodies against TNF-α have been approved by the FDA -- infliximab, adalimumab, golimumab, and Department of Life Science certolizumab pegol -- with many more in clinical and Division of Life and Pharmaceutical Sciences preclinical development. The situation is similar for Ewha Womans University HER2, CD20, EGFR, and VEGF, each having one or Seoul 120-750, Korea more approved antibodies and many more under Correspondence: Tel, 82-2-3277-4240; development. This review discusses the different bind- Fax, 82-2-3277-3760; E-mail, [email protected] ing characteristics, mechanisms of action, and bio- http://dx.doi.org/10.3858/emm.2011.43.10.063 logical and clinical activities of multiple monoclonal antibodies against TNF-α, HER-2, CD20, and EGFR and Accepted 2 August 2011 provides insights into the development of therapeutic Available Online 3 August 2011 antibodies. Abbreviations: ADC, antibody-drug conjugate; ADCC, antibody- dependent cellular cytotoxicity; CD20, cluster of differentiation Keywords: antibodies, monoclonal; antigens, CD20; 20; CDC, complement dependent cytotoxicity; CLL, chronic pharmacology; receptor, epidermal growth factor; re- lymphocytic leukemia; ECD, extracellular domain; EGFR, epi- ceptor, erbB-2; tumor necrosis factor-α dermal growth factor receptor; EpCAM, epithelial cell adhe- sion molecule; FcγR, Fc gamma receptor; -

The Two Tontti Tudiul Lui Hi Ha Unit
THETWO TONTTI USTUDIUL 20170267753A1 LUI HI HA UNIT ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2017 /0267753 A1 Ehrenpreis (43 ) Pub . Date : Sep . 21 , 2017 ( 54 ) COMBINATION THERAPY FOR (52 ) U .S . CI. CO - ADMINISTRATION OF MONOCLONAL CPC .. .. CO7K 16 / 241 ( 2013 .01 ) ; A61K 39 / 3955 ANTIBODIES ( 2013 .01 ) ; A61K 31 /4706 ( 2013 .01 ) ; A61K 31 / 165 ( 2013 .01 ) ; CO7K 2317 /21 (2013 . 01 ) ; (71 ) Applicant: Eli D Ehrenpreis , Skokie , IL (US ) CO7K 2317/ 24 ( 2013. 01 ) ; A61K 2039/ 505 ( 2013 .01 ) (72 ) Inventor : Eli D Ehrenpreis, Skokie , IL (US ) (57 ) ABSTRACT Disclosed are methods for enhancing the efficacy of mono (21 ) Appl. No. : 15 /605 ,212 clonal antibody therapy , which entails co - administering a therapeutic monoclonal antibody , or a functional fragment (22 ) Filed : May 25 , 2017 thereof, and an effective amount of colchicine or hydroxy chloroquine , or a combination thereof, to a patient in need Related U . S . Application Data thereof . Also disclosed are methods of prolonging or increasing the time a monoclonal antibody remains in the (63 ) Continuation - in - part of application No . 14 / 947 , 193 , circulation of a patient, which entails co - administering a filed on Nov. 20 , 2015 . therapeutic monoclonal antibody , or a functional fragment ( 60 ) Provisional application No . 62/ 082, 682 , filed on Nov . of the monoclonal antibody , and an effective amount of 21 , 2014 . colchicine or hydroxychloroquine , or a combination thereof, to a patient in need thereof, wherein the time themonoclonal antibody remains in the circulation ( e . g . , blood serum ) of the Publication Classification patient is increased relative to the same regimen of admin (51 ) Int . -

Development and Preclinical Evaluation of Cixutumumab Drug
www.nature.com/scientificreports OPEN Development and preclinical evaluation of cixutumumab drug conjugates in a model of insulin growth factor receptor I (IGF‑1R) positive cancer Viswas Raja Solomon1, Elahe Alizadeh1, Wendy Bernhard2, Amal Makhlouf1,3, Siddesh V. Hartimath1, Wayne Hill2, Ayman El‑Sayed2, Kris Barreto2, Clarence Ronald Geyer 2 & Humphrey Fonge1,4* Overexpression of insulin growth factor receptor type 1 (IGF‑1R) is observed in many cancers. Antibody drug conjugates (ADCs) with PEGylated maytansine (PEG6‑DM1) show promise in vitro. We developed PEG6‑DM1 ADCs with low and high drug to antibody ratios (DAR) using an anti‑ IGF‑1R antibody cixutumumab (IMC‑A12). Conjugates with low (cixutumumab‑PEG6‑DM1‑Low) and high (cixutumumab‑PEG6‑DM1‑High) DAR as 3.4 and 7.2, respectively, were generated. QC was performed by UV spectrophotometry, HPLC, bioanalyzer, and biolayer‑interferometry. We compared the in vitro binding and internalization rates of the ADCs in IGF‑1R‑positive MCF‑7/Her18 cells. We radiolabeled the ADCs with 111In and used microSPECT/CT imaging and ex vivo biodistribution to understand their in vivo behavior in MCF‑7/Her18 xenograft mice. The therapeutic potential of the ADC was studied in vitro and in mouse xenograft. Internalization rates of all ADCs was high and increased over 48 h and EC50 was in the low nanomolar range. MicroSPECT/CT imaging and ex vivo 111 biodistribution showed signifcantly lower tumor uptake of In‑cixutumumab‑PEG6‑DM1‑High 111 111 compared to In‑cixutumumab‑PEG6‑DM1‑Low and In‑cixutumumab. Cixutumumab‑PEG6‑DM1‑ Low signifcantly prolonged the survival of mice bearing MCF‑7/Her18 xenograft compared with cixutumumab, cixutumumab‑PEG6‑DM1‑High, or the PBS control group. -

Antibodies for the Treatment of Brain Metastases, a Dream Or a Reality?
pharmaceutics Review Antibodies for the Treatment of Brain Metastases, a Dream or a Reality? Marco Cavaco, Diana Gaspar, Miguel ARB Castanho * and Vera Neves * Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Av. Prof. Egas Moniz, 1649-028 Lisboa, Portugal * Correspondence: [email protected] (M.A.R.B.C.); [email protected] (V.N.) Received: 19 November 2019; Accepted: 28 December 2019; Published: 13 January 2020 Abstract: The incidence of brain metastases (BM) in cancer patients is increasing. After diagnosis, overall survival (OS) is poor, elicited by the lack of an effective treatment. Monoclonal antibody (mAb)-based therapy has achieved remarkable success in treating both hematologic and non-central-nervous system (CNS) tumors due to their inherent targeting specificity. However, the use of mAbs in the treatment of CNS tumors is restricted by the blood–brain barrier (BBB) that hinders the delivery of either small-molecules drugs (sMDs) or therapeutic proteins (TPs). To overcome this limitation, active research is focused on the development of strategies to deliver TPs and increase their concentration in the brain. Yet, their molecular weight and hydrophilic nature turn this task into a challenge. The use of BBB peptide shuttles is an elegant strategy. They explore either receptor-mediated transcytosis (RMT) or adsorptive-mediated transcytosis (AMT) to cross the BBB. The latter is preferable since it avoids enzymatic degradation, receptor saturation, and competition with natural receptor substrates, which reduces adverse events. Therefore, the combination of mAbs properties (e.g., selectivity and long half-life) with BBB peptide shuttles (e.g., BBB translocation and delivery into the brain) turns the therapeutic conjugate in a valid approach to safely overcome the BBB and efficiently eliminate metastatic brain cells. -

(INN) for Biological and Biotechnological Substances
INN Working Document 05.179 Update 2013 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) INN Working Document 05.179 Distr.: GENERAL ENGLISH ONLY 2013 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) International Nonproprietary Names (INN) Programme Technologies Standards and Norms (TSN) Regulation of Medicines and other Health Technologies (RHT) Essential Medicines and Health Products (EMP) International Nonproprietary Names (INN) for biological and biotechnological substances (a review) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int ) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected] ). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form/en/index.html ). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned.