Dual Targeting of the Epidermal Growth Factor Receptor Using
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanism of Resistance to Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors and a Potential Treatment Strategy
cells Review Mechanism of Resistance to Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitors and a Potential Treatment Strategy Tatsuya Nagano * , Motoko Tachihara and Yoshihiro Nishimura Division of Respiratory Medicine, Department of Internal Medicine, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan; [email protected] (M.T.); [email protected] (Y.N.) * Correspondence: [email protected]; Tel.: +81-78-382-5660 Received: 25 October 2018; Accepted: 15 November 2018; Published: 15 November 2018 Abstract: Treatment with epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs) improves the overall survival of patients with EGFR-mutated non-small-cell lung cancer (NSCLC). First-generation EGFR-TKIs (e.g., gefitinib and erlotinib) or second-generation EGFR-TKIs (e.g., afatinib and dacomitinib) are effective for the treatment of EGFR-mutated NSCLC, especially in patients with EGFR exon 19 deletions or an exon 21 L858R mutation. However, almost all cases experience disease recurrence after 1 to 2 years due to acquired resistance. The EGFR T790M mutation in exon 20 is the most frequent alteration associated with the development of acquired resistance. Osimertinib—a third-generation EGFR-TKI—targets the T790M mutation and has demonstrated high efficacy against EGFR-mutated lung cancer. However, the development of acquired resistance to third-generation EGFR-TKI, involving the cysteine residue at codon 797 mutation, has been observed. Other mechanisms of acquired resistance include the activation of alternative pathways or downstream targets and histological transformation (i.e., epithelial–mesenchymal transition or conversion to small-cell lung cancer). -

Nimotuzumab, an Antitumor Antibody That Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding While Permitting the Active Receptor Conformation
Published OnlineFirst July 7, 2009; DOI: 10.1158/0008-5472.CAN-08-4518 Experimental Therapeutics, Molecular Targets, and Chemical Biology Nimotuzumab, an Antitumor Antibody that Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding while Permitting the Active Receptor Conformation Ariel Talavera,1,2 Rosmarie Friemann,2,3 Silvia Go´mez-Puerta,1 Carlos Martinez-Fleites,4 Greta Garrido,1 Ailem Rabasa,1 Alejandro Lo´pez-Requena,1 Amaury Pupo,1 Rune F. Johansen,3 Oliberto Sa´nchez,5 Ute Krengel,2 and Ernesto Moreno1 1Center of Molecular Immunology, Havana, Cuba; 2Department of Chemistry, University of Oslo, Oslo, Norway; and 3Center for Molecular and Behavioral Neuroscience, Institute of Medical Microbiology, University of Oslo, Rikshospitalet HF, Oslo, Norway; 4Department of Chemistry, University of York, Heslington, York, United Kingdom; and 5Center for Genetic Engineering and Biotechnology, Havana, Cuba Abstract region of the EGFR (eEGFR), leaving the dimerization ‘‘arm’’ in Overexpression of the epidermal growth factor (EGF) receptor domain II ready for binding a second monomer (4, 5). It has been (EGFR) in cancer cells correlates with tumor malignancy and shown that the eEGFR adopts a ‘‘tethered’’ or inactive conformation poor prognosis for cancer patients. For this reason, the EGFR in the absence of EGF (6). In this characteristic conformation, has become one of the main targets of anticancer therapies. the dimerization arm is hidden by interactions with domain IV, Structural data obtained in the last few years have revealed whereas domains I and III remain separated. Thus, to adopt the the molecular mechanism for ligand-induced EGFR dimeriza- ‘‘extended’’ or active conformation observed in the crystal structure tion and subsequent signal transduction, and also how this of the complex with EGF (4), the receptor must undergo a major signal is blocked by either monoclonal antibodies or small conformational change that brings together domains I and III (6). -

Deciphering Molecular Mechanisms and Prioritizing Therapeutic Targets in Cardio-Oncology
Figure 1. This is a pilot view to explore the potential of EpiGraphDB to inform us about proteins that are linked to the pathophysiology of cancer and cardiovascular disease (CVD). For each cancer type (pink diamonds), we searched for cancer related proteins (light blue circles) that interact with other proteins identified as protein quantitative trait loci (pQTLs) for CVD (red diamonds for pathologies, orange triangles for risk factors). These pQTLs can be acting in cis (solid lines) or trans-acting (dotted lines). Proteins can interact either directly, a protein-protein interaction (dotted blue edges), or through the participation in the same pathway (red parallel lines). Shared pathways are represented with blue hexagons. We also queried which of these proteins are targeted by existing drugs. We found that the cancer drug cetuximab (yellow circle) inhibits EGFR. Other potential drugs are depicted in light brown hexagonal meta-nodes that are detailed below. Deciphering molecular mechanisms and prioritizing therapeutic targets in cardio-oncology Pau Erola1,2, Benjamin Elsworth1,2, Yi Liu2, Valeriia Haberland2 and Tom R Gaunt1,2,3 1 CRUK Integrative Cancer Epidemiology Programme; 2 MRC Integrative Epidemiology Unit, University of Bristol; 3 The Alan Turing Institute Cancer and cardiovascular disease (CVD) make by far the immense What is EpiGraphDB? contribution to the totality of human disease burden, and although mortality EpiGraphDB is an analytical platform and graph database that aims to is declining the number of those living with the disease shows little address the necessity of innovative and scalable approaches to harness evidence of change (Bhatnagar et al., Heart, 2016). -

Targeted and Novel Therapy in Advanced Gastric Cancer Julie H
Selim et al. Exp Hematol Oncol (2019) 8:25 https://doi.org/10.1186/s40164-019-0149-6 Experimental Hematology & Oncology REVIEW Open Access Targeted and novel therapy in advanced gastric cancer Julie H. Selim1 , Shagufta Shaheen2 , Wei‑Chun Sheu3 and Chung‑Tsen Hsueh4* Abstract The systemic treatment options for advanced gastric cancer (GC) have evolved rapidly in recent years. We have reviewed the recent data of clinical trial incorporating targeted agents, including inhibitors of angiogenesis, human epidermal growth factor receptor 2 (HER2), mesenchymal–epithelial transition, epidermal growth factor receptor, mammalian target of rapamycin, claudin‑18.2, programmed death‑1 and DNA. Addition of trastuzumab to platinum‑ based chemotherapy has become standard of care as front‑line therapy in advanced GC overexpressing HER2. In the second‑line setting, ramucirumab with paclitaxel signifcantly improves overall survival compared to paclitaxel alone. For patients with refractory disease, apatinib, nivolumab, ramucirumab and TAS‑102 have demonstrated single‑agent activity with improved overall survival compared to placebo alone. Pembrolizumab has demonstrated more than 50% response rate in microsatellite instability‑high tumors, 15% response rate in tumors expressing programmed death ligand 1, and non‑inferior outcome in frst‑line treatment compared to chemotherapy. This review summarizes the current state and progress of research on targeted therapy for advanced GC. Keywords: Gastric cancer, Targeted therapy, Human epidermal growth factor receptor 2, Programmed death‑1, Vascular endothelial growth factor receptor 2 Background GC mortality which is consistent with overall decrease in Gastric cancer (GC), including adenocarcinoma of the GC-related deaths [4]. gastroesophageal junction (GEJ) and stomach, is the ffth Tere have been several eforts to perform large-scale most common cancer and the third leading cause of can- molecular profling and classifcation of GC. -

The Impact of EGFR T790M Mutations and BIM Mrna Expression On
Author Manuscript Published OnlineFirst on February 3, 2014; DOI: 10.1158/1078-0432.CCR-13-2233 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. The impact of EGFR T790M mutations and BIM mRNA expression on outcome in patients with EGFR-mutant NSCLC treated with erlotinib or chemotherapy in the randomized phase III EURTAC trial Carlota Costa1, Miguel Angel Molina1, Ana Drozdowskyj2, Ana Giménez-Capitán1, Jordi Bertran-Alamillo1, Niki Karachaliou1, Radj Gervais3, Bartomeu Massuti4, Jia Wei1,5, Teresa Moran6, Margarita Majem7, Enriqueta Felip8, Enric Carcereny6, Rosario Garcia-Campelo9, Santiago Viteri1, Miquel Taron1,6, Mayumi Ono10, Petros Giannikopoulos11, Trever Bivona11,12, Rafael Rosell6,11,13 1Pangaea Biotech, Barcelona, Spain; 2Pivotal, Madrid, Spain; 3Centre François Baclesse, Caen, France; 4Hospital General de Alicante, Alicante, Spain; 5Drum Tower Hospital, Nanjing, China; 6Catalan Institute of Oncology, Badalona, Spain; 7Hospital Sant Pau, Barcelona, Spain; 8Hospital Vall d’Hebron, Barcelona, Spain; 9Complejo Hospitalario Universitario, La Coruña, Spain; 10Kyushu University, Fukuoka, Japan; 11Cancer Therapeutics Innovation Group, New York, NY, USA; 12Helen Diller Comprehensive Cancer Center, University of California, San Francisco, CA, USA; 13Molecular Oncology Research (MORe) Foundation, Barcelona, Spain Running title: BIM mRNA expression and survival in NSCLC Keywords: BIM mRNA expression, EGFR mutations, T790M, chemotherapy, erlotinib Financial support: Work in Dr Rafael Rosell’s laboratory is partially supported by a grant from La Caixa Foundation and by a grant from Red Tematica de Investigacion Cooperativa en Cancer (RTICC; grant RD12/0036/0072). Neither of these funding agencies was involved in the study design or conduct, data management or analysis, manuscript preparation or review, or the decision to submit for publication. -
Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -

Therapeutic Inhibition of VEGF Signaling and Associated Nephrotoxicities
REVIEW www.jasn.org Therapeutic Inhibition of VEGF Signaling and Associated Nephrotoxicities Chelsea C. Estrada,1 Alejandro Maldonado,1 and Sandeep K. Mallipattu1,2 1Division of Nephrology, Department of Medicine, Stony Brook University, Stony Brook, New York; and 2Renal Section, Northport Veterans Affairs Medical Center, Northport, New York ABSTRACT Inhibition of vascular endothelial growth factor A (VEGFA)/vascular endothelial with hypertension and proteinuria. Re- growth factor receptor 2 (VEGFR2) signaling is a common therapeutic strategy in ports describe histologic changes in the oncology, with new drugs continuously in development. In this review, we consider kidney primarily as glomerular endothe- the experimental and clinical evidence behind the diverse nephrotoxicities associ- lial injury with thrombotic microangiop- ated with the inhibition of this pathway. We also review the renal effects of VEGF athy (TMA).8 Nephrotic syndrome has inhibition’s mediation of key downstream signaling pathways, specifically MAPK/ also been observed,9 with the clinical ERK1/2, endothelial nitric oxide synthase, and mammalian target of rapamycin manifestations varying according to (mTOR). Direct VEGFA inhibition via antibody binding or VEGF trap (a soluble decoy mechanism and direct target of VEGF receptor) is associated with renal-specific thrombotic microangiopathy (TMA). Re- inhibition. ports also indicate that tyrosine kinase inhibition of the VEGF receptors is prefer- Current VEGF inhibitors can be clas- entially associated with glomerulopathies such as minimal change disease and FSGS. sifiedbytheirtargetofactioninthe Inhibition of the downstream pathway RAF/MAPK/ERK has largely been associated VEGFA-VEGFR2 pathway: drugs that with tubulointerstitial injury. Inhibition of mTOR is most commonly associated with bind to VEGFA, sequester VEGFA, in- albuminuria and podocyte injury, but has also been linked to renal-specificTMA.In hibit receptor tyrosine kinases (RTKs), all, we review the experimentally validated mechanisms by which VEGFA-VEGFR2 or inhibit downstream pathways. -
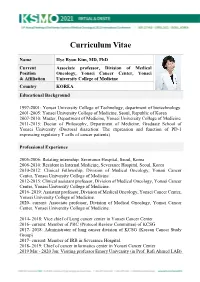
KSMO 2021 CV SS Hye
Curriculum Vitae Name Hye Ryun Kim, MD, PhD Current Associate professor, Division of Medical Position Oncology, Yonsei Cancer Center, Yonsei & Affiliation University College of Medicine Country KOREA Educational Background 1997-2001: Yonsei University College of Technology, department of biotechnology. 2001-2005: Yonsei University College of Medicine, Seoul, Republic of Korea 2007-2010: Master, Department of Medicine, Yonsei University College of Medicine 2011-2015: Doctor of Philosophy, Department of Medicine, Graduate School of Yonsei University (Doctoral dissertion: The expression and function of PD-1 expressing regulatory T cells of cancer patients) Professional Experience 2005-2006: Rotating internship, Severance Hospital, Seoul, Korea 2006-2010: Resident in Internal Medicine, Severance Hospital, Seoul, Korea 2010-2012: Clinical Fellowship, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2012-2015: Clinical assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2016- 2019: Assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2020- current: Associate professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2014- 2018: Vice chief of Lung cancer center in Yonsei Cancer Center 2016- current: Member of PRC (Protocol Review Committee) of KCSG 2017- 2018: Administrator of lung cancer division of KCSG (Korean Cancer Study Group) 2017- current: -

Advances in Epidermal Growth Factor Receptor Specific Immunotherapy: Lessons to Be Learned from Armed Antibodies
www.oncotarget.com Oncotarget, 2020, Vol. 11, (No. 38), pp: 3531-3557 Review Advances in epidermal growth factor receptor specific immunotherapy: lessons to be learned from armed antibodies Fleury Augustin Nsole Biteghe1,*, Neelakshi Mungra2,*, Nyangone Ekome Toung Chalomie4, Jean De La Croix Ndong5, Jean Engohang-Ndong6, Guillaume Vignaux7, Eden Padayachee8, Krupa Naran2,* and Stefan Barth2,3,* 1Department of Radiation Oncology and Biomedical Sciences, Cedars-Sinai Medical, Los Angeles, CA, USA 2Medical Biotechnology & Immunotherapy Research Unit, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 3South African Research Chair in Cancer Biotechnology, Department of Integrative Biomedical Sciences, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 4Sun Yat-Sen University, Zhongshan Medical School, Guangzhou, China 5Department of Orthopedic Surgery, New York University School of Medicine, New York, NY, USA 6Department of Biological Sciences, Kent State University at Tuscarawas, New Philadelphia, OH, USA 7Arctic Slope Regional Corporation Federal, Beltsville, MD, USA 8Department of Physiology, University of Kentucky, Lexington, KY, USA *These authors contributed equally to this work Correspondence to: Stefan Barth, email: [email protected] Keywords: epidermal growth factor receptor (EGFR); recombinant immunotoxins (ITs); targeted human cytolytic fusion proteins (hCFPs); recombinant antibody-drug conjugates (rADCs); recombinant antibody photoimmunoconjugates (rAPCs) Received: May 30, 2020 Accepted: August 11, 2020 Published: September 22, 2020 Copyright: © 2020 Biteghe et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy
cancers Review Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy Laura Boyero 1 , Amparo Sánchez-Gastaldo 2, Miriam Alonso 2, 1 1,2,3, , 1,2, , José Francisco Noguera-Uclés , Sonia Molina-Pinelo * y and Reyes Bernabé-Caro * y 1 Institute of Biomedicine of Seville (IBiS) (HUVR, CSIC, Universidad de Sevilla), 41013 Seville, Spain; [email protected] (L.B.); [email protected] (J.F.N.-U.) 2 Medical Oncology Department, Hospital Universitario Virgen del Rocio, 41013 Seville, Spain; [email protected] (A.S.-G.); [email protected] (M.A.) 3 Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), 28029 Madrid, Spain * Correspondence: [email protected] (S.M.-P.); [email protected] (R.B.-C.) These authors contributed equally to this work. y Received: 16 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Simple Summary: Immuno-oncology has redefined the treatment of lung cancer, with the ultimate goal being the reactivation of the anti-tumor immune response. This has led to the development of several therapeutic strategies focused in this direction. However, a high percentage of lung cancer patients do not respond to these therapies or their responses are transient. Here, we summarized the impact of immunotherapy on lung cancer patients in the latest clinical trials conducted on this disease. As well as the mechanisms of primary and acquired resistance to immunotherapy in this disease. Abstract: After several decades without maintained responses or long-term survival of patients with lung cancer, novel therapies have emerged as a hopeful milestone in this research field. -

Resistance Mechanisms to Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer
www.nature.com/bjc REVIEW ARTICLE Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer Alessandro Leonetti1,2, Sugandhi Sharma2, Roberta Minari1, Paola Perego3, Elisa Giovannetti2,4 and Marcello Tiseo 1,5 Osimertinib is an irreversible, third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor that is highly selective for EGFR-activating mutations as well as the EGFR T790M mutation in patients with advanced non-small cell lung cancer (NSCLC) with EGFR oncogene addiction. Despite the documented efficacy of osimertinib in first- and second-line settings, patients inevitably develop resistance, with no further clear-cut therapeutic options to date other than chemotherapy and locally ablative therapy for selected individuals. On account of the high degree of tumour heterogeneity and adaptive cellular signalling pathways in NSCLC, the acquired osimertinib resistance is highly heterogeneous, encompassing EGFR-dependent as well as EGFR- independent mechanisms. Furthermore, data from repeat plasma genotyping analyses have highlighted differences in the frequency and preponderance of resistance mechanisms when osimertinib is administered in a front-line versus second-line setting, underlying the discrepancies in selection pressure and clonal evolution. This review summarises the molecular mechanisms of resistance to osimertinib in patients with advanced EGFR-mutated NSCLC, including MET/HER2 amplification, activation of the RAS–mitogen-activated protein kinase (MAPK) or RAS–phosphatidylinositol -

Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches
cancers Review Leptomeningeal Metastases from Solid Tumors: Recent Advances in Diagnosis and Molecular Approaches Alessia Pellerino 1,* , Priscilla K. Brastianos 2, Roberta Rudà 1,3 and Riccardo Soffietti 1 1 Department of Neuro-Oncology, University and City of Health and Science Hospital, 10126 Turin, Italy; [email protected] (R.R.); riccardo.soffi[email protected] (R.S.) 2 Massachusetts General Hospital Cancer Center, Harvard Medical School, Boston, MA 02115, USA; [email protected] 3 Department of Neurology, Castelfranco Veneto and Brain Tumor Board Treviso Hospital, 31100 Treviso, Italy * Correspondence: [email protected]; Tel.: +39-011-633-4904 Simple Summary: Leptomeningeal metastases are a devastating complication of solid tumors with poor survival, regardless of the type of treatments. The limited efficacy of targeted agents is due to the molecular divergence between leptomeningeal recurrences and primary site, as well as the presence of a heterogeneous blood-brain barrier and blood-tumor barrier that interfere with the penetration of drugs into the brain. The diagnosis of leptomeningeal metastases is achieved by neurological examination, and/or brain and spinal magnetic resonance, and/or a positive cerebrospinal fluid cytology. The presence of neoplastic cells in the cerebrospinal fluid examination is the gold-standard for the diagnosis of leptomeningeal metastases; however, novel techniques known as “liquid biopsy” aim to improve the sensitivity and specificity in detecting circulating neoplastic cells or DNA in the cerebrospinal fluid. Targeted therapies and immunotherapies have changed the natural history Citation: Pellerino, A.; Brastianos, of metastatic solid tumors, including lung, breast cancer, and melanoma. Targeting actionable P.K.; Rudà, R.; Soffietti, R.