Development and Preclinical Evaluation of Cixutumumab Drug
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HER2 Inhibition in Gastro-Oesophageal Cancer: a Review Drawing on Lessons Learned from Breast Cancer
Submit a Manuscript: http://www.f6publishing.com World J Gastrointest Oncol 2018 July 15; 10(7): 159-171 DOI: 10.4251/wjgo.v10.i7.159 ISSN 1948-5204 (online) REVIEW HER2 inhibition in gastro-oesophageal cancer: A review drawing on lessons learned from breast cancer Hazel Lote, Nicola Valeri, Ian Chau Hazel Lote, Nicola Valeri, Centre for Molecular Pathology, Accepted: May 30, 2018 Institute of Cancer Research, Sutton SM2 5NG, United Kingdom Article in press: May 30, 2018 Published online: July 15, 2018 Hazel Lote, Nicola Valeri, Ian Chau, Department of Medicine, Royal Marsden Hospital, Sutton SM2 5PT, United Kingdom ORCID number: Hazel Lote (0000-0003-1172-0372); Nicola Valeri (0000-0002-5426-5683); Ian Chau (0000-0003-0286-8703). Abstract Human epidermal growth factor receptor 2 (HER2)- Author contributions: Lote H wrote the original manuscript and revised it following peer review comments; Valeri N reviewed inhibition is an important therapeutic strategy in HER2- the manuscript; Chau I reviewed and contributed to the content of amplified gastro-oesophageal cancer (GOC). A significant the manuscript. proportion of GOC patients display HER2 amplification, yet HER2 inhibition in these patients has not displayed Supported by National Health Service funding to the National the success seen in HER2 amplified breast cancer. Mu- Institute for Health Research Biomedical Research Centre at ch of the current evidence surrounding HER2 has been the Royal Marsden NHS Foundation Trust and The Institute of obtained from studies in breast cancer, and we are only re- Cancer Research, No. A62, No. A100, No. A101 and No. A159; Cancer Research UK funding, No. -

Nimotuzumab, an Antitumor Antibody That Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding While Permitting the Active Receptor Conformation
Published OnlineFirst July 7, 2009; DOI: 10.1158/0008-5472.CAN-08-4518 Experimental Therapeutics, Molecular Targets, and Chemical Biology Nimotuzumab, an Antitumor Antibody that Targets the Epidermal Growth Factor Receptor, Blocks Ligand Binding while Permitting the Active Receptor Conformation Ariel Talavera,1,2 Rosmarie Friemann,2,3 Silvia Go´mez-Puerta,1 Carlos Martinez-Fleites,4 Greta Garrido,1 Ailem Rabasa,1 Alejandro Lo´pez-Requena,1 Amaury Pupo,1 Rune F. Johansen,3 Oliberto Sa´nchez,5 Ute Krengel,2 and Ernesto Moreno1 1Center of Molecular Immunology, Havana, Cuba; 2Department of Chemistry, University of Oslo, Oslo, Norway; and 3Center for Molecular and Behavioral Neuroscience, Institute of Medical Microbiology, University of Oslo, Rikshospitalet HF, Oslo, Norway; 4Department of Chemistry, University of York, Heslington, York, United Kingdom; and 5Center for Genetic Engineering and Biotechnology, Havana, Cuba Abstract region of the EGFR (eEGFR), leaving the dimerization ‘‘arm’’ in Overexpression of the epidermal growth factor (EGF) receptor domain II ready for binding a second monomer (4, 5). It has been (EGFR) in cancer cells correlates with tumor malignancy and shown that the eEGFR adopts a ‘‘tethered’’ or inactive conformation poor prognosis for cancer patients. For this reason, the EGFR in the absence of EGF (6). In this characteristic conformation, has become one of the main targets of anticancer therapies. the dimerization arm is hidden by interactions with domain IV, Structural data obtained in the last few years have revealed whereas domains I and III remain separated. Thus, to adopt the the molecular mechanism for ligand-induced EGFR dimeriza- ‘‘extended’’ or active conformation observed in the crystal structure tion and subsequent signal transduction, and also how this of the complex with EGF (4), the receptor must undergo a major signal is blocked by either monoclonal antibodies or small conformational change that brings together domains I and III (6). -

Or Ramucirumab (IMC-1121B) Plus Mitoxantrone and Prednisone in Men with Metastatic Docetaxel-Pretreated Castration-Resistant Prostate Cancer
European Journal of Cancer (2015) 51, 1714– 1724 Available at www.sciencedirect.com ScienceDirect journal homepage: www.ejcancer.com A randomised non-comparative phase II trial of cixutumumab (IMC-A12) or ramucirumab (IMC-1121B) plus mitoxantrone and prednisone in men with metastatic docetaxel-pretreated castration-resistant prostate cancer Maha Hussain a,1,⇑, Dana Rathkopf b,1, Glenn Liu c,1, Andrew Armstrong d,1, Wm. Kevin Kelly e, Anna Ferrari f, John Hainsworth g, Adarsh Joshi h, Rebecca R. Hozak i, Ling Yang h, Jonathan D. Schwartz h,2, Celestia S. Higano j,1 a University of Michigan Comprehensive Cancer Center, Ann Arbor, MI, United States b Memorial Sloan-Kettering, New York, NY, United States c University of Wisconsin, Carbone Cancer Center, Madison, WI, United States d Duke Cancer Institute and Duke Prostate Center, Duke University, Durham, NC, United States e Thomas Jefferson University, Philadelphia, PA, United States f New York University Clinical Cancer Center, New York, NY, United States g Sarah Cannon Research Institute, Nashville, TN, United States h Eli Lilly and Company, Bridgewater, NJ, United States i Eli Lilly and Company, Indianapolis, IN, United States j University of Washington, Fred Hutchinson Cancer Research Center, Seattle, WA, United States Received 11 February 2015; received in revised form 27 April 2015; accepted 10 May 2015 Available online 13 June 2015 KEYWORDS Abstract Background: Cixutumumab, a human monoclonal antibody (HuMAb), targets the Ramucirumab insulin-like growth factor receptor. Ramucirumab is a recombinant HuMAb that binds to vas- Cixutumumab cular endothelial growth factor receptor-2. A non-comparative randomised phase II study Mitoxantrone evaluated cixutumumab or ramucirumab plus mitoxantrone and prednisone (MP) in Prednisone metastatic castration-resistant prostate cancer (mCRPC). -

Targeted and Novel Therapy in Advanced Gastric Cancer Julie H
Selim et al. Exp Hematol Oncol (2019) 8:25 https://doi.org/10.1186/s40164-019-0149-6 Experimental Hematology & Oncology REVIEW Open Access Targeted and novel therapy in advanced gastric cancer Julie H. Selim1 , Shagufta Shaheen2 , Wei‑Chun Sheu3 and Chung‑Tsen Hsueh4* Abstract The systemic treatment options for advanced gastric cancer (GC) have evolved rapidly in recent years. We have reviewed the recent data of clinical trial incorporating targeted agents, including inhibitors of angiogenesis, human epidermal growth factor receptor 2 (HER2), mesenchymal–epithelial transition, epidermal growth factor receptor, mammalian target of rapamycin, claudin‑18.2, programmed death‑1 and DNA. Addition of trastuzumab to platinum‑ based chemotherapy has become standard of care as front‑line therapy in advanced GC overexpressing HER2. In the second‑line setting, ramucirumab with paclitaxel signifcantly improves overall survival compared to paclitaxel alone. For patients with refractory disease, apatinib, nivolumab, ramucirumab and TAS‑102 have demonstrated single‑agent activity with improved overall survival compared to placebo alone. Pembrolizumab has demonstrated more than 50% response rate in microsatellite instability‑high tumors, 15% response rate in tumors expressing programmed death ligand 1, and non‑inferior outcome in frst‑line treatment compared to chemotherapy. This review summarizes the current state and progress of research on targeted therapy for advanced GC. Keywords: Gastric cancer, Targeted therapy, Human epidermal growth factor receptor 2, Programmed death‑1, Vascular endothelial growth factor receptor 2 Background GC mortality which is consistent with overall decrease in Gastric cancer (GC), including adenocarcinoma of the GC-related deaths [4]. gastroesophageal junction (GEJ) and stomach, is the ffth Tere have been several eforts to perform large-scale most common cancer and the third leading cause of can- molecular profling and classifcation of GC. -

Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -

IGF System in Sarcomas: a Crucial Pathway with Many Unknowns to Exploit for Therapy
61 1 Journal of Molecular C Mancarella and Targeting IGF system in sarcoma 61:1 T45–T60 Endocrinology K Scotlandi THEMATIC REVIEW 40 YEARS OF IGF1 IGF system in sarcomas: a crucial pathway with many unknowns to exploit for therapy Caterina Mancarella and Katia Scotlandi Experimental Oncology Lab, CRS Development of Biomolecular Therapies, Orthopaedic Rizzoli Institute, Bologna, Italy Correspondence should be addressed to K Scotlandi: [email protected] This paper forms part of a special section on 40 Years of IGF1. The guest editors for this section were Derek LeRoith and Emily Gallagher. Abstract The insulin-like growth factor (IGF) system has gained substantial interest due to its Key Words involvement in regulating cell proliferation, differentiation and survival during anoikis f sarcomas and after conventional and targeted therapies. However, results from clinical trials have f IGF system been largely disappointing, with only a few but notable exceptions, such as trials targeting f targeted therapy sarcomas, especially Ewing sarcoma. This review highlights key studies focusing on IGF f clinical trials signaling in sarcomas, specifically studies underscoring the properties that make this system an attractive therapeutic target and identifies new relationships that may be exploited. This review discusses the potential roles of IGF2 mRNA-binding proteins (IGF2BPs), discoidin domain receptors (DDRs) and metalloproteinase pregnancy-associated plasma protein-A (PAPP-A) in regulating the IGF system. Deeper investigation of these novel regulators of the IGF system may help us to further elucidate the spatial and temporal control of the IGF Journal of Molecular axis, as understanding the control of this axis is essential for future clinical studies. -
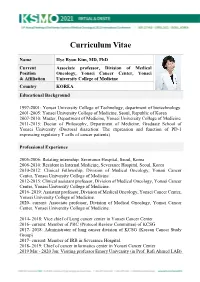
KSMO 2021 CV SS Hye
Curriculum Vitae Name Hye Ryun Kim, MD, PhD Current Associate professor, Division of Medical Position Oncology, Yonsei Cancer Center, Yonsei & Affiliation University College of Medicine Country KOREA Educational Background 1997-2001: Yonsei University College of Technology, department of biotechnology. 2001-2005: Yonsei University College of Medicine, Seoul, Republic of Korea 2007-2010: Master, Department of Medicine, Yonsei University College of Medicine 2011-2015: Doctor of Philosophy, Department of Medicine, Graduate School of Yonsei University (Doctoral dissertion: The expression and function of PD-1 expressing regulatory T cells of cancer patients) Professional Experience 2005-2006: Rotating internship, Severance Hospital, Seoul, Korea 2006-2010: Resident in Internal Medicine, Severance Hospital, Seoul, Korea 2010-2012: Clinical Fellowship, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2012-2015: Clinical assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2016- 2019: Assistant professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2020- current: Associate professor, Division of Medical Oncology, Yonsei Cancer Center, Yonsei University College of Medicine. 2014- 2018: Vice chief of Lung cancer center in Yonsei Cancer Center 2016- current: Member of PRC (Protocol Review Committee) of KCSG 2017- 2018: Administrator of lung cancer division of KCSG (Korean Cancer Study Group) 2017- current: -

Advances in Epidermal Growth Factor Receptor Specific Immunotherapy: Lessons to Be Learned from Armed Antibodies
www.oncotarget.com Oncotarget, 2020, Vol. 11, (No. 38), pp: 3531-3557 Review Advances in epidermal growth factor receptor specific immunotherapy: lessons to be learned from armed antibodies Fleury Augustin Nsole Biteghe1,*, Neelakshi Mungra2,*, Nyangone Ekome Toung Chalomie4, Jean De La Croix Ndong5, Jean Engohang-Ndong6, Guillaume Vignaux7, Eden Padayachee8, Krupa Naran2,* and Stefan Barth2,3,* 1Department of Radiation Oncology and Biomedical Sciences, Cedars-Sinai Medical, Los Angeles, CA, USA 2Medical Biotechnology & Immunotherapy Research Unit, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 3South African Research Chair in Cancer Biotechnology, Department of Integrative Biomedical Sciences, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa 4Sun Yat-Sen University, Zhongshan Medical School, Guangzhou, China 5Department of Orthopedic Surgery, New York University School of Medicine, New York, NY, USA 6Department of Biological Sciences, Kent State University at Tuscarawas, New Philadelphia, OH, USA 7Arctic Slope Regional Corporation Federal, Beltsville, MD, USA 8Department of Physiology, University of Kentucky, Lexington, KY, USA *These authors contributed equally to this work Correspondence to: Stefan Barth, email: [email protected] Keywords: epidermal growth factor receptor (EGFR); recombinant immunotoxins (ITs); targeted human cytolytic fusion proteins (hCFPs); recombinant antibody-drug conjugates (rADCs); recombinant antibody photoimmunoconjugates (rAPCs) Received: May 30, 2020 Accepted: August 11, 2020 Published: September 22, 2020 Copyright: © 2020 Biteghe et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. -

Therapeutic Targeting of the IGF Axis
cells Review Therapeutic Targeting of the IGF Axis Eliot Osher and Valentine M. Macaulay * Department of Oncology, University of Oxford, Oxford, OX3 7DQ, UK * Correspondence: [email protected]; Tel.: +44-1865617337 Received: 8 July 2019; Accepted: 9 August 2019; Published: 14 August 2019 Abstract: The insulin like growth factor (IGF) axis plays a fundamental role in normal growth and development, and when deregulated makes an important contribution to disease. Here, we review the functions mediated by ligand-induced IGF axis activation, and discuss the evidence for the involvement of IGF signaling in the pathogenesis of cancer, endocrine disorders including acromegaly, diabetes and thyroid eye disease, skin diseases such as acne and psoriasis, and the frailty that accompanies aging. We discuss the use of IGF axis inhibitors, focusing on the different approaches that have been taken to develop effective and tolerable ways to block this important signaling pathway. We outline the advantages and disadvantages of each approach, and discuss progress in evaluating these agents, including factors that contributed to the failure of many of these novel therapeutics in early phase cancer trials. Finally, we summarize grounds for cautious optimism for ongoing and future studies of IGF blockade in cancer and non-malignant disorders including thyroid eye disease and aging. Keywords: IGF; type 1 IGF receptor; IGF-1R; cancer; acromegaly; ophthalmopathy; IGF inhibitor 1. Introduction Insulin like growth factors (IGFs) are small (~7.5 kDa) ligands that play a critical role in many biological processes including proliferation and protection from apoptosis and normal somatic growth and development [1]. IGFs are members of a ligand family that includes insulin, a dipeptide comprised of A and B chains linked via two disulfide bonds, with a third disulfide linkage within the A chain. -

Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy
cancers Review Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy Laura Boyero 1 , Amparo Sánchez-Gastaldo 2, Miriam Alonso 2, 1 1,2,3, , 1,2, , José Francisco Noguera-Uclés , Sonia Molina-Pinelo * y and Reyes Bernabé-Caro * y 1 Institute of Biomedicine of Seville (IBiS) (HUVR, CSIC, Universidad de Sevilla), 41013 Seville, Spain; [email protected] (L.B.); [email protected] (J.F.N.-U.) 2 Medical Oncology Department, Hospital Universitario Virgen del Rocio, 41013 Seville, Spain; [email protected] (A.S.-G.); [email protected] (M.A.) 3 Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), 28029 Madrid, Spain * Correspondence: [email protected] (S.M.-P.); [email protected] (R.B.-C.) These authors contributed equally to this work. y Received: 16 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Simple Summary: Immuno-oncology has redefined the treatment of lung cancer, with the ultimate goal being the reactivation of the anti-tumor immune response. This has led to the development of several therapeutic strategies focused in this direction. However, a high percentage of lung cancer patients do not respond to these therapies or their responses are transient. Here, we summarized the impact of immunotherapy on lung cancer patients in the latest clinical trials conducted on this disease. As well as the mechanisms of primary and acquired resistance to immunotherapy in this disease. Abstract: After several decades without maintained responses or long-term survival of patients with lung cancer, novel therapies have emerged as a hopeful milestone in this research field. -

2017 Immuno-Oncology Medicines in Development
2017 Immuno-Oncology Medicines in Development Adoptive Cell Therapies Drug Name Organization Indication Development Phase ACTR087 + rituximab Unum Therapeutics B-cell lymphoma Phase I (antibody-coupled T-cell receptor Cambridge, MA www.unumrx.com immunotherapy + rituximab) AFP TCR Adaptimmune liver Phase I (T-cell receptor cell therapy) Philadelphia, PA www.adaptimmune.com anti-BCMA CAR-T cell therapy Juno Therapeutics multiple myeloma Phase I Seattle, WA www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 "armored" CAR-T Juno Therapeutics recurrent/relapsed chronic Phase I cell therapy Seattle, WA lymphocytic leukemia (CLL) www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 CAR-T cell therapy Intrexon B-cell malignancies Phase I Germantown, MD www.dna.com ZIOPHARM Oncology www.ziopharm.com Boston, MA anti-CD19 CAR-T cell therapy Kite Pharma hematological malignancies Phase I (second generation) Santa Monica, CA www.kitepharma.com National Cancer Institute Bethesda, MD Medicines in Development: Immuno-Oncology 1 Adoptive Cell Therapies Drug Name Organization Indication Development Phase anti-CEA CAR-T therapy Sorrento Therapeutics liver metastases Phase I San Diego, CA www.sorrentotherapeutics.com TNK Therapeutics San Diego, CA anti-PSMA CAR-T cell therapy TNK Therapeutics cancer Phase I San Diego, CA www.sorrentotherapeutics.com Sorrento Therapeutics San Diego, CA ATA520 Atara Biotherapeutics multiple myeloma, Phase I (WT1-specific T lymphocyte South San Francisco, CA plasma cell leukemia www.atarabio.com -

Co-Targeting HER2/Erbb2 and Insulin-Like Growth Factor-1
Signature: Med Sci Monit, 2002; 8(12): BR521-526 WWW.MEDSCIMONIT.COM PMID: 12503030 Basic Research Received: 2002.11.08 Accepted: 2002.11.20 Co-targeting HER2/ErbB2 and insulin-like growth BR Published: 2002.12.27 factor-1 receptors causes synergistic inhibition of growth in HER2-overexpressing breast cancer cells Authors’ Contribution: A Study Design abcdef b AG B Data Collection Anne Camirand , Yuhong Lu , Michael Pollak C Statistical Analysis D Data Interpretation Department of Oncology, McGill University, Montréal, QC, Canada E Manuscript Preparation F Literature Search Source of support: Streams of Excellence program of the Canadian Breast Cancer Research Institute. G Funds Collection Summary Background: The humanized anti-HER2 monoclonal antibody trastuzumab (Herceptin®) is useful in the treatment of ErbB2-overexpressing breast cancers, but its efficiency is limited because devel- opment of resistance is common. In order to study the possibility of improving the efficacy of therapies directed against HER2/erbB2, we investigated the effects of co-targeting this recep- tor and the insulin-like growth factor 1 receptor (IGF-1R), a widely-expressed protein tyro- sine kinase with important roles in suppression of apoptosis and stimulation of proliferation. Material/Methods: The experimental strategy involved combining trastuzumab treatment and reduction of IGF- 1R signaling through incremental heat-induced expression of the dominant-negative IGF-1 receptor 486/STOP under the control of the heat-sensitive Drosophila HSP70 promoter, in HER2/erbB2-overexpressing MCF7her18 breast cancer cells. Results: Isobologram analysis of combinatorial treatment data revealed a strong synergistic interaction between trastuzumab treatment and the induction of the dominant-negative IGF-1R expres- sion, resulting in potentiation of growth inhibition in transfected cancer cells.