Whole Body Low Dose Computed Tomography (WBLDCT) Can Be Comparable to Whole-Body Magnetic Resonance Imaging (WBMRI) in the Assessment of Multiple Myeloma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SPR 2013 Postgraduate Course May 14-15, 2013 SAM Questionnaire Tuesday, May 14, 2013 CHEST Digital Radiography Robert Macdougal
SPR 2013 Postgraduate Course May 14-15, 2013 SAM Questionnaire Tuesday, May 14, 2013 CHEST Digital Radiography Robert MacDougall, MSc 1. Which of the following is unaffected by the selection of Value of Interest Look Up Table (VOI-LUT): A. Diagnostic information in the processed image B. Target Exposure (ET) C. Exposure Index (EI) D. Deviation Index (DI) E. Brightness and contrast of the displayed image Correct Answer: B 2. Exposure Index (EI) represents: A. The exposure at the entrance to the patient B. The exposure at the detector plane measured with an ion chamber C. The brightness of the displayed image D. The exposure at the detector calculated from the mean signal response of the detector within the Values of Interest E. The deviation from a target exposure Correct Answer: D References 1. An Exposure Indicator for Digital Radiography: Report of AAPM Task Group 116. American Association of Physicists in Medicine. Accessed April 10, 2013. https://www.aapm.org/pubs/reports/RPT_116.pdf 2. Internation Electrotechnical Commission. Medical Electrical Equipment. Exposure Index of Digital X-ray Imaging Systems - Part 1: Definitions and Requirements for General Radiography. IEC Publication No. 62494-1. Geneva, Switzerland: International Electrotechnical Commission, 2002. Functional Chest MR Imaging Hyun Woo Goo, MD, PhD 3. Which one of the followings is the LEAST likely limitation of thoracic MR imaging? A. Low signal-to-noise ratio due to the low proton density of the lung B. Potential hazards from ionizing radiation C. Motion artifacts from respiratory motion and cardiac pulsation D. Relatively long examination time E. Susceptibility artifacts from multiple air-tissue interfaces Correct Answer: B References 1. -
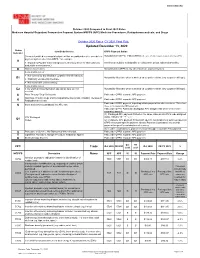
Updated December 13, 2020
WWW.SNMMI.ORG October 2020 Compared to Final 2021 Rates Medicare Hospital Outpatient Prospective Payment System HOPPS (APC) Medicine Procedures, Radiopharmaceuticals, and Drugs October 2020 Rates CY 2021 Final Rule Updated December 13, 2020 Status Item/Code/Service OPPS Payment Status Indicator Services furnished to a hospital outpatient that are paid under a fee schedule or Not paid under OPPS. Paid by MACs under a fee schedule or payment system other than OPPS. payment system other than OPPS,* for example: A ● Separately Payable Clinical Diagnostic Laboratory Services (Not subject to Services are subject to deductible or coinsurance unless indicated otherwise. deductible or coinsurance.) D Discontinued Codes Not paid under OPPS or any other Medicare payment system. Items and Services: ● Not covered by any Medicare outpatient benefit category Not paid by Medicare when submitted on outpatient claims (any outpatient bill type). E1 ● Statutorily excluded by Medicare ● Not reasonable and necessary Items and Services: E2 ● for which pricing information and claims data are not Not paid by Medicare when submitted on outpatient claims (any outpatient bill type). available G Pass-Through Drug/ Biologicals Paid under OPPS; separate APC payment NonPass-Through Drugs and nonimplantable Biologicals, including Therapeutic Paid under OPPS; separate APC payment K Radiopharmaceuticals Paid under OPPS; payment is packaged into payment for other services. Therefore, Items and Services packaged into APC rate N there is no separate APC payment. Paid under OPPS; Addendum B displays APC assignments when services are separately payable. (1) Packaged APC payment if billed on the same claim as a HCPCS code assigned STV-Packaged status indicator “S,” “T,” or “V.” Q1 Codes (2) Composite APC payment if billed with specific combinations of services based on OPPS composite-specific payment criteria. -

Criteria for Acceptability of Medical Radiological Equipment Used in Diagnostic Radiology, Nuclear Medicine and Radiotherapy
EUROPEAN COMMISSION RADIATION PROTECTION N° 162 Criteria for Acceptability of Medical Radiological Equipment used in Diagnostic Radiology, Nuclear Medicine and Radiotherapy Directorate-General for Energy Directorate D — Nuclear Safety & Fuel Cycle Unit D4 — Radiation Protection 2012 This report was prepared by Quality Assurance Reference Centre for the European Commission under contract N°. ENER/10/NUCL/SI2.581655 and represents those organisations’ views on the subject matter. The views and opinions expressed herein do not necessarily state or reflect those of the European Commission and should not be relied upon as a statement of the Commission’s views. The European Commission does not guarantee the accuracy of the data included in this report, nor does it accept responsibility for any use made thereof. Europe Direct is a service to help you find answers to your questions about the European Union Freephone number (*): 00 800 6 7 8 9 10 11 (*) Certain mobile telephone operators do not allow access to 00 800 numbers or these calls may be billed. More information on the European Union is available on the Internet (http://europa.eu). Luxembourg: Publications Office of the European Union, 2012 ISBN 978-92-79-27747-4 doi: 10.2768/22561 © European Union, 2012 Reproduction is authorised provided the source is acknowledged. Printed in Luxembourg 2 FOREWORD Luxembourg, October 2012 The work of the European Commission in the field of radiation protection is governed by the Euratom Treaty and the secondary legislation adopted under it. Council Directive 97/43/Euratom (the Medical Exposure Directive, MED) is the legal act defining the Euratom requirements on radiation protection of patients and of other individuals submitted to medical exposure. -

Diagnostic Radiology Physics Diagnostic This Publication Provides a Comprehensive Review of Topics Relevant to Diagnostic Radiology Physics
A Handbook for Teachers and Students A Handbook for Teachers Diagnostic Diagnostic This publication provides a comprehensive review of topics relevant to diagnostic radiology physics. It is intended to provide the basis for the education of medical physicists in the field of diagnostic radiology. Bringing together the work of 41 authors and reviewers from 12 countries, the handbook covers a broad range of topics including radiation physics, dosimetry and Radiology instrumentation, image quality and image perception, imaging modality specific topics, recent advances in digital techniques, and radiation biology and protection. It is not designed to replace the large number of textbooks available on many aspects of diagnostic radiology physics, but is expected Radiology Physics Physics to fill a gap in the teaching material for medical radiation physics in imaging, providing in a single manageable volume the broadest coverage of topics currently available. The handbook has been endorsed by several international professional bodies and will be of value to those preparing for their certification A Handbook for as medical physicists, radiologists and diagnostic radiographers. Teachers and Students D.R. Dance S. Christofides A.D.A. Maidment I.D. McLean K.H. Ng Technical Editors International Atomic Energy Agency Vienna ISBN 978–92–0–131010–1 1 @ DIAGNOSTIC RADIOLOGY PHYSICS: A HANDBOOK FOR TEACHERS AND STUDENTS The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GHANA OMAN ALBANIA GREECE PAKISTAN ALGERIA GUATEMALA -

Diffraction-Enhanced X-Ray Imaging of in Vitro Breast Tumours
UNIVERSITY OF HELSINKI REPORT SERIES IN PHYSICS HU-P-D113 DIFFRACTION-ENHANCED X-RAY IMAGING OF IN VITRO BREAST TUMOURS Jani Keyriläinen Division of X-ray Physics Department of Physical Sciences Faculty of Science University of Helsinki Helsinki, Finland Department of Oncology Helsinki University Central Hospital Helsinki, Finland ACADEMIC DISSERTATION To be presented, with the permission of the Faculty of Science of the University of Helsinki, for public criticism in Auditorium D101 of the Department of Physical Sciences (Physicum), Gustaf Hällströmin katu 2, on October 29th, 2004, at 12 o’clock noon. Helsinki 2004 ISSN 0356-0961 ISBN 952-10-1655-8 ISBN 952-10-1656-6 (pdf-version) http://ethesis.helsinki.fi/ Helsinki 2004 Yliopistopaino PREFACE This thesis is based on research done at the Division of X-ray Physics, Department of Physical Sciences, University of Helsinki (HU, Finland), at the Medical Beamline ID17, European Synchrotron Radiation Facility (ESRF, Grenoble, France), and at the departments of Oncology, Pathology and Radiology, Helsinki University Central Hospital (HUCH, Finland), all of which are acknowledged. I wish to express my gratitude to Professor Juhani Keinonen, Ph.D., Head of the Department of Physical Sciences, and to Professor Seppo Manninen, Ph.D., former Head of the Division of X-ray Physics, for the opportunity to work at the Department. I also wish to thank Professor Heikki Joensuu, M.D., Ph.D., Head of the Department of Oncology, and William Thomlinson, Ph.D., former Beamline Responsible, ID17, for allowing me to use the outstanding working facilities of their institutions. I am most grateful to my supervisors, Professor Pekka Suortti, Ph.D., Department of Physical Sciences, and Docent Mikko Tenhunen, Ph.D., Chief Physicist of the Department of Oncology, for proposing to me the topic of this study and guiding me throughout this research work. -

Whole Body MR
Whole Body MR: Techniques and Staging in Oncology ‐ How To • Extent of disease and staging • Response to treatment – Early assessment of response to treatment may allow more individualized therapy • Surveillance • Complications – Osteonecrosis – Infection • Cancer predisposition syndromes screening Condition Associated neoplasms Surveillance NF type I Optic nerve glioma, neurofibromas, leukemia (especially juvenile Annual physical examination; annual ophthalmologic examination in early childhood (to age 5 y); regular myelomonocytic leukemia developmental assessment and blood pressure monitoring; appropriate monitoring by a specialist and myelodysplastic syndromes, MPNST (lifetime risk of 8%–13%), GIST according to CNS, skeletal, or cardiovascular abnormalities (lifetime risk of 6%), pheochromocytoma (1%), rhabdomyosarcoma, neuroblastoma Beckwith- Wilms tu (40%–43%), hepatoblastoma (12-20%), adrenocortical ca, Abdominal US every 3 mo to age 7 y; measurement of serum AFP level every 3 mo to age 4 y; daily Wiedemann neuroblastoma, rhabdomyosarcoma abdominal examination by the caretaker at the discretion of the caretaker or parent; abdominal syndrome examination by a physician every 6 mo MEN 1 Parathyroid gland adenomas (65%–90%), pancreatic neuroendocrine tumors Screening starting at age 5–10 y, including measurement of fasting glucose, calcium, PTH, insulin, (50%–70%), and anterior pituitary gland adenomas (25%–65%) prolactin, and IGF1 levels; annual pancreatic US; pancreatic and pituitary MR imaging every 3–5 y; yearly abdominal CT or MR -
Paleoradiology Imaging Mummies and Fossils
R. K. Chhem · D. R. Brothwell Paleoradiology R. K. Chhem · D. R. Brothwell Paleoradiology Imaging Mummies and Fossils With 390 Figures and 58 Tables 123 Don R. Brothwell, PhD Department of Archaeology The University of York The King’s Manor York Y01 7EP UK Rethy K. Chhem, MD, PhD, FRCPC Department of Diagnostic Radiology and Nuclear Medicine Schulich School of Medicine and Dentistry University of Western Ontario London Health Sciences Centre 339 Windermere Road London, Ontario N6A 5A5 Canada Library of Congress Control Number: 2007936308 ISBN 978-3-540-48832-3 Springer Berlin Heidelberg New York This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilm or in any other way, and storage in data banks. Duplication of this publication or parts thereof is permitted only under the provisions of the German Copyright Law of September 9, 1965, in its current version, and permission for use must always be obtained from Springer-Verlag. Violations are liable for prosecution under the German Copyright Law. Springer is a part of Springer Science+Business Media springer.com © Springer-Verlag Berlin Heidelberg 2008 The use of general descriptive names, registered names, trademarks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. Product liability: The publishers cannot guarantee the accuracy of any information about dosage and application contained in this book. -

Whole-Body Imaging of the Musculoskeletal System: the Value of MR Imaging
CORE Metadata, citation and similar papers at core.ac.uk Provided by PubMed Central Skeletal Radiol (2007) 36:1109–1119 DOI 10.1007/s00256-007-0323-5 REVIEW ARTICLE Whole-body imaging of the musculoskeletal system: the value of MR imaging Gerwin P. Schmidt & Maximilian F. Reiser & Andrea Baur-Melnyk Received: 17 December 2006 /Revised: 25 March 2007 /Accepted: 9 April 2007 / Published online: 7 June 2007 # ISS 2007 Abstract In clinical practice various modalities are used Keywords Whole-body . Imaging . Musculoskeletal . for whole-body imaging of the musculoskeletal system, Magnetic resonance imaging including radiography, bone scintigraphy, computed tomog- raphy, magnetic resonance imaging (MRI), and positron emission tomography-computed tomography (PET-CT). Introduction Multislice CT is far more sensitive than radiographs in the assessment of trabecular and cortical bone destruction and The skeletal system is a frequent target of metastatic spread allows for evaluation of fracture risk. The introduction of from various primary tumors like carcinoma of the breast, combined PET-CT scanners has markedly increased diag- lung and prostate cancer. Moreover, primary malignancies nostic accuracy for the detection of skeletal metastases may also originate from the bone marrow, such as lymphoma compared with PET alone. The unique soft-tissue contrast and multiple myeloma [1]. Therefore, it is highly important of MRI enables for precise assessment of bone marrow to accurately assess manifestations of malignant diseases infiltration and adjacent soft tissue structures so that within the bone marrow in order to facilitate adequate alterations within the bone marrow may be detected before therapy and predict prognosis. osseous destruction becomes apparent in CT or metabolic Only pronounced destruction of bone with loss of bone changes occur on bone scintigraphy or PET scan. -

PET Coding Review and Resources
Volume 3, Issue 3 SUMMER 2006 pet center of excellence newsletter SNM Members Appointed to National Academy of Sciences PET Coding Review Committee to Review State of Nuclear Medicine and Resources By Denise A. Merlino, MBA, CNMT, CPC, FSNMTS Peter S. Conti, immediate past president of ET is a technology that continues to evolve, and coding, coverage, and payment both SNM and the PET Center of Excellence, Psystems have been evolving along with it. In March of 2005, PET providers and a number of other SNM members were transitioned from using complicated “G” series Healthcare Common Procedure Cod- recently named to the National Academy of ing System (HCPCS) codes to the American Medical Association (AMA) Current Sciences (NAS) ad hoc committee of experts Procedural Terminology (CPT) codes for Medicare-covered indications. Last January, to review the “state of the science” for nuclear PET radiopharmaceutical HCPCS codes were changed for FDG and rubidium. Finally, medicine. in May, the National Oncologic PET Registry (NOPR) went into operation providing “The 13-month $700,000 study will pro- Medicare coverage of FDG PET studies for all cancer indications that did not fall under vide the opportunity to validate the importance the current national coverage determination (NCD) policy. of basic nuclear medicine research,” said Every change brings with it the need to train staff, update billing software, and make Conti, a professor of radiology, pharmacy and certain that all billing procedures are in compliance with the new regulations. The list biomedical engineering at the University of below summarizes the top 10 things you need to know about coding PET today. -
Evicore Preface to the Imaging Guidelines V20.0.2018 Eff 05.17.18
CLINICAL GUIDELINES Preface to the Imaging Guidelines Version 20.0.2018 Effective May 17, 2018 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies: This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2016 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2018 eviCore healthcare. All rights reserved. Imaging Guidelines V20.0.2018 Preface to the Imaging Guidelines Preface-1: Guideline Development 3 Preface-2: Benefits, Coverage Policies, and Eligibility Issues 4 Preface-3: Clinical Information 5 Preface-4: Coding Issues 9 Preface-5: Whole Body Imaging 16 Preface-6: References 19 Preface-7: Copyright Information 20 Preface-8: Trademarks 21 ______________________________________________________________________________________________________ © 2018 eviCore healthcare. All Rights Reserved. Page 2 of 21 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Imaging Guidelines V20.0.2018 Preface-1: Guideline Development The eviCore healthcare (eviCore) evidence-based, proprietary clinical guidelines evaluate a range of advanced imaging and procedures, including CT, MRI, PET, and Radiation Oncology, Sleep Studies and Cardiac and Spine interventions. -

Radiation Doses Radiation Technology Have Represented Sig- Received by Patients and the Associated Nificant Gains in the Prognosis for Early Dis- Health Risks
Forty-Third Annual Meeting Program Advances in Radiation Protection in Medicine April 16-17, 2007 Crystal Forum Crystal City Marriott 1999 Jefferson Davis Highway Arlington, Virginia Co-sponsors American College of Radiology Reston, Virginia Xoran Technologies Ann Arbor, Michigan Introduction Advances in Radiation Protection in Medicine Forty-Third Annual Meeting of the National Council on Radiation Protection and Measurements (NCRP) During the past two decades remarkable increased the radiation exposure of both progress has been made in the development patients and medical practitioners. Special and application of new medical technologies concerns have been raised regarding use of that utilize radiation for the early detection the newer radiation modalities in pediatric and effective treatment of cancer and other radiology and in imaging and radiotherapy diseases. These advances, however, are procedures with pregnant women. accompanied by many questions about how NCRP’s 2007 Annual Meeting features to maximize medical benefits to patients, presentations by physicians, medical physi- while controlling and reducing their risks cists, and experts in radiation health effects from exposure to ionizing radiation. These who will discuss the rapid growth in use of issues are the theme of the 2007 NCRP relatively new medical radiation diagnostic Annual Meeting. and therapeutic procedures, and the current Although the many advances in medical state of understanding of radiation doses radiation technology have represented sig- received by patients and the associated nificant gains in the prognosis for early dis- health risks. Topical areas of focus at the ease detection and therapy, there are issues meeting will include diagnostic radiology, regarding the safety of these new radiation nuclear medicine, interventional radiology, modalities that are of current interest and radiation oncology, and interdisciplinary concern to the medical community. -

Novel Muscle Imaging in Inflammatory Rheumatic Diseases—A Focus on Ultrasound Shear Wave Elastography and Quantitative
Novel muscle imaging in inflammatory rheumatic diseases — a focus on ultrasound shear wave elastography and quantitative MRI Item Type Article Authors Farrow, Matthew; Biglands, J.; Alfuraih, A.M.; Wakefield, R.J.; Tan, A.L. Citation Farrow M, Biglands J, Alfuraih AM et al (2020) Novel muscle imaging in inflammatory rheumatic diseases - a focus on ultrasound shear wave elastography and quantitative MRI. Frontiers In Medicine. 7: Article 434. Rights © 2020 Farrow, Biglands, Alfuraih, Wakefield and Tan. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. Download date 28/09/2021 22:32:08 Link to Item http://hdl.handle.net/10454/18472 PERSPECTIVE published: 12 August 2020 doi: 10.3389/fmed.2020.00434 Novel Muscle Imaging in Inflammatory Rheumatic Diseases—A Focus on Ultrasound Shear Wave Elastography and Quantitative MRI Matthew Farrow 1,2,3, John Biglands 2,4, Abdulrahman M. Alfuraih 5, Richard J. Wakefield 1,2 and Ai Lyn Tan 1,2* 1 Leeds Institute of Rheumatic and Musculoskeletal Medicine, Chapel Allerton Hospital, University of Leeds, Leeds, United Kingdom, 2 NIHR Leeds Biomedical Research Centre, Leeds Teaching Hospitals NHS Trust, Leeds, United