Global Vaccination: Trends and U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Compendium of the Findings of the OPCAST Pandemic Subgroup 12
1 A Compendium of the Findings of the Obama PCAST Ad Hoc Subgroup on Pandemic Preparedness and Response December 23, 2020 Introduction A subset of the former members of President Obama’s Council of Advisors on Science and Technology (here OPCAST)—ten individuals who played particularly important roles in producing the six OPCAST reports between 2009 and 2016 that dealt with issues related to pandemic preparedness and response1—came together starting in March of this year to consider how insights from those studies might be combined with more recent research and current observations to develop suggestions about how the U.S. response to the COVID-19 pandemic could be improved. The Subgroup has produced six reports, addressing • the national strategic pandemic-response stockpile (May 20) • the role of contact tracing (June 18) • the role of public health data in controlling the spread of COVID-19 (July 28) • testing for the pathogen (August 18) • recommendations for the coming COVID-19 commission (September 21) • needs for improved epidemiological modeling (September 28) Each report was distributed, upon completion, to selected members of the Trump COVID-19 team and the Biden campaign staff, selected governors and members of Congress, selected public health experts outside government, and the media. The reports have also been posted on the OPCAST team’s website, http://opcast.org, together with a few opinion pieces based on them. In the current volume, we have assembled all six reports in full, preceded by a set of brief summaries. Four of the reports are followed by short updates taking account of developments since the reports first came out. -

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -
Pneumococcal Vaccine
Vaccines for Primary Care Pneumococcal, Shingles, Pertussis Devang Patel, M.D. Assistant Professor Chief of Service, MICU ID Service University of Maryland School of Medicine Pneumococcal Vaccine Pneumococcal Disease • 2nd most common cause of vaccine preventable death in the US • Major Syndromes – Pneumonia – Bacteremia – Meningitis Active Bacterial Core Surveillance (ABCs) Report Emerging Infections Program Network Streptococcus pneumoniae, 2010 (ORIG) Vaccine Target • Polysaccharide capsule allows bacteria to resist phagocytosis • Antibodies to capsule facilitate phagocytosis • >90 different pneumococcal capsular serotypes • Vaccines contain most common serotypes causing disease Pneumococcal Vaccines Pneumococcal Vaccines • Pneumococcal polysaccharide vaccine (PPSV23; Pneumovax) – Contains capsular polysaccharides – 23 most commonly infecting serotypes • Cause 60% of all pneumococcal infections in adults – Not recommended for children <2 due to poor immunogenicity of polysaccharides Pneumococcal Vaccines • Pneumococcal conjugate vaccine (PCV13, Prevnar) – Polysaccharides linked to nontoxic protein • higher antigenicity – Stimulates mucosal antibody • Eliminates nasal carriage in young children • Herd effect in adults – Reduction in PCV7 serotype disease >90% Prevnar 13 • 2000 - PCV7 approved for infants toddlers • 2010 - PCV13 recommended for infants and toddlers • 2012 – ACIP recommended PCV13 for high- risk adults • 2014 – recommended for adults >65 • 2018 – ACIP will revisit PCV13 use in adults – Childhood vaccines may eliminate -
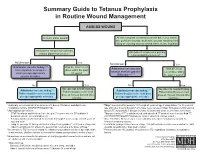
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

YF-VAX® Rx Only AHFS Category
YF-VAX® Rx Only Laboratory Personnel AHFS Category: 80:12 Laboratory personnel who handle virulent yellow fever virus or concentrated preparations Rx only of the yellow fever vaccine virus strains may be at risk of exposure by direct or indirect Yellow Fever Vaccine contact or by aerosols. (14) DESCRIPTION CONTRAINDICATIONS ® Hypersensitivity YF-VAX , Yellow Fever Vaccine, for subcutaneous use, is prepared by culturing the YF-VAX is contraindicated in anyone with a history of acute hypersensitivity reaction to any 17D-204 strain of yellow fever virus in living avian leukosis virus-free (ALV-free) chicken component of the vaccine. (See DESCRIPTION section.) Because the yellow fever virus embryos. The vaccine contains sorbitol and gelatin as a stabilizer, is lyophilized, and is used in the production of this vaccine is propagated in chicken embryos, do not administer hermetically sealed under nitrogen. No preservative is added. Each vial of vaccine is YF-VAX to anyone with a history of acute hypersensitivity to eggs or egg products due to supplied with a separate vial of sterile diluent, which contains Sodium Chloride Injection a risk of anaphylaxis. Less severe or localized manifestations of allergy to eggs or to USP – without a preservative. YF-VAX is formulated to contain not less than 4.74 log10 feathers are not contraindications to vaccine administration and do not usually warrant plaque forming units (PFU) per 0.5 mL dose throughout the life of the product. Before vaccine skin testing. (See PRECAUTIONS section, Testing for Hypersensitivity Re- reconstitution, YF-VAX is a pinkish color. After reconstitution, YF-VAX is a slight pink-brown actions subsection.) Generally, persons who are able to eat eggs or egg products may suspension. -

Vaccines for Preteens
| DISEASES and the VACCINES THAT PREVENT THEM | INFORMATION FOR PARENTS Vaccines for Preteens: What Parents Should Know Last updated JANUARY 2017 Why does my child need vaccines now? to get vaccinated. The best time to get the flu vaccine is as soon as it’s available in your community, ideally by October. Vaccines aren’t just for babies. Some of the vaccines that While it’s best to be vaccinated before flu begins causing babies get can wear off as kids get older. And as kids grow up illness in your community, flu vaccination can be beneficial as they may come in contact with different diseases than when long as flu viruses are circulating, even in January or later. they were babies. There are vaccines that can help protect your preteen or teen from these other illnesses. When should my child be vaccinated? What vaccines does my child need? A good time to get these vaccines is during a yearly health Tdap Vaccine checkup. Your preteen or teen can also get these vaccines at This vaccine helps protect against three serious diseases: a physical exam required for sports, school, or camp. It’s a tetanus, diphtheria, and pertussis (whooping cough). good idea to ask the doctor or nurse every year if there are any Preteens should get Tdap at age 11 or 12. If your teen didn’t vaccines that your child may need. get a Tdap shot as a preteen, ask their doctor or nurse about getting the shot now. What else should I know about these vaccines? These vaccines have all been studied very carefully and are Meningococcal Vaccine safe. -
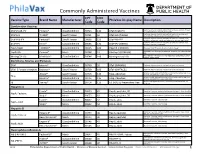
Commonly Administered Vaccines
Commonly Administered Vaccines CPT CVX Vaccine Type Brand Name Manufacturer PhilaVax Display Name Description Code Code Combination Vaccines Diptheria, tetanus toxoids and acellular pertussis vaccine, Hepati- DTaP-HepB-IPV Pediarix® GlaxoSmithKline 90723 110 DTaP-HepB-IPV tis B and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine and DTaP-Hib TriHIBit® Sanofi Pasteur 90721 50 DTaP-Hib (TriHIBit) Haemophilus influenzae type b conjugate vaccine Diptheria, tetanus toxoids and acellular pertussis vaccine, Hae- DTaP-Hib-IPV Pentacel® Sanofi Pasteur 90698 120 DTaP-Hib-IPV mophilus influenzae type b, and poliovirus vaccine, inactivated Diptheria, tetanus toxoids and acellular pertussis vaccine, and DTaP-IPV Kinrix® GlaxoSmithKline 90696 130 DTaP-IPV (KINRIX) poliovirus vaccine, inactivated HepA-HepB TWINRIX® GlaxoSmithKline 90636 104 HepA/B (TWINRIX) Hepatisis A and Hepatitis B vaccine, adult dosage Hepatitis B and Hemophilus influenza b vaccine, for intramuscular HepB-Hib Comvax® Merck 90748 51 Hib-Hep B (COMVAX) use Haemophilus influenza b and meningococcal sero groups C and Y MeningC/Y-Hib Menhibrix® GlaxoSmithKline 90644 148 Meningococcal-Hib vaccine, 4 dose series Diphtheria, Tetanus and Pertussis DTaP Infanrix® GlaxoSmithKline 90700 20 DTaP (INFANRIX) Diptheria, tetanus toxoids and acellular pertussis vaccine DTaP, 5 Pertussis Antigens Daptacel® Sanofi Pasteur 90700 106 DTaP (DAPTACEL) Diptheria, tetanus toxoids and acellular pertussis vaccine Tetanus toxoid, reduced diphtheria toxoid, and acellular -

Ensuring the World's Poorest Children Benefit from Lifesaving Vaccines
WHAT WE’RE LEARNING Ensuring the World’s Poorest Children Benefit from Lifesaving Vaccines “Supporting children’s immunization is undoubtedly the best investment we’ve ever made.” —Bill and Melinda Gates Program Area pertussis) vaccine. When GAVI was The Challenge launched, 71 percent of the world’s Global Health Most people in rich nations do not children were receiving DTP vaccine. realize how difficult it is simply to By 2004, the rate had increased to survive early childhood in many parts Our Goal 78 percent. of the world. Every year, more than Prevent needless deaths in the world’s GAVI has concentrated the greatest 10 million children are buried before poorest countries by increasing access percentage of its resources on speeding they reach their fifth birthday. Of these, to basic vaccines and speeding the the introduction of newer, more about 1.4 million die from diseases that introduction of new vaccines. expensive vaccines, including those for existing vaccines can prevent—including hepatitis B, Haemophilus influenzae B measles, pertussis, and tetanus. Another Our Progress in Brief (Hib), and yellow fever. The vaccine 1.1 million die from diseases for which The Global Alliance for Vaccines for hepatitis B, for example, had been we will soon have vaccines. Because and Immunization (GAVI), which widely used in rich countries for childhood death is so frequent, parents the foundation helped to launch in 20 years but was severely underutilized in some countries in Africa and Asia 1999, has made significant progress. in the developing world because of a don’t even name their babies until they Children’s immunization is no longer a lack of political will and the vaccine’s reach several months of age. -
Association Between Thimerosal-Containing Vaccine and Autism
BRIEF REPORT Association Between Thimerosal-Containing Vaccine and Autism Anders Hviid, MSc Context Mercuric compounds are nephrotoxic and neurotoxic at high doses. Thi- Michael Stellfeld, MD merosal, a preservative used widely in vaccine formulations, contains ethylmercury. Thus it has been suggested that childhood vaccination with thimerosal-containing vac- Jan Wohlfahrt, MSc cine could be causally related to neurodevelopmental disorders such as autism. Mads Melbye, MD, PhD Objective To determine whether vaccination with a thimerosal-containing vaccine is associated with development of autism. IGH DOSES OF MERCURIC COM- Design, Setting, and Participants Population-based cohort study of all children pounds are nephrotoxic and born in Denmark from January 1, 1990, until December 31, 1996 (N=467450) com- neurotoxic.1 Thimerosal, an paring children vaccinated with a thimerosal-containing vaccine with children vacci- organic compound that con- nated with a thimerosal-free formulation of the same vaccine. Htains ethylmercury, has been widely used Main Outcome Measures Rate ratio (RR) for autism and other autistic-spectrum since the 1930s as a preservative in cer- disorders, including trend with dose of ethylmercury. tain vaccines. In the 1990s, an increas- Results During 2986654 person-years, we identified 440 autism cases and 787 cases ing number of different vaccines con- of other autistic-spectrum disorders. The risk of autism and other autistic-spectrum taining thimerosal were introduced in disorders did not differ significantly between children vaccinated with thimerosal- immunization schedules around the containing vaccine and children vaccinated with thimerosal-free vaccine (RR, 0.85 [95% world, and thus the average cumula- confidence interval {CI}, 0.60-1.20] for autism; RR, 1.12 [95% CI, 0.88-1.43] for other tive exposure to thimerosal in infants has autistic-spectrum disorders). -

MERS-Cov Data Sharing Case Study Report November 2018
MERS-CoV Data Sharing Case Study Report November 2018 1. Introduction a. Background to the ongoing MERS-CoV outbreak: In September 2012, Dr Ali Mohamed Zaki reported the isolation of a novel betacoronavirus on ProMED-mail, the internet infectious disease alert system run by the International Society for Infectious Diseases.1 The patient, a 60-year-old male from Saudi Arabia presenting with pneumonia- like symptoms died from an unknown viral infection in June 2012.2 Later dubbed the Middle East Respiratory Syndrome Coronavirus (MERS-CoV),3 this emerging infectious disease has now been responsible for more than 2,200 laboratory-confirmed infections in people from 27 countries, and close to 800 deaths.4 The vast majority of these cases have been recorded in Saudi Arabia, however MERS-CoV is considered a severe emerging disease with the potential to cause a major global health emergency.5 Epidemiological investigations have revealed that primary human infections with MERS-CoV are often, but not always associated with contact with dromedary camels around the Arabian Peninsula.6 Human-to-human transmission of MERS-CoV has been responsible for case clusters in family groups and healthcare facilities. The incidence of hospital-acquired infections have been reduced with the employment of strict infection control measures,7 and the international public health community remain on high alert for new introductions. In 2015, South Korea saw the largest outbreak of MERS- CoV outside of the Eastern Mediterranean with 186 confirmed cases and 38 deaths.7 New cases of MERS-CoV infection continue to be reported mostly from the Eastern Mediterranean. -

Diphtheria Tetanus and Pertussis Vaccine Supply Update October 2016
Diphtheria Tetanus and Pertussis Vaccine Supply Update UNICEF Supply Division October 2016 0 Diphtheria Tetanus and Pertussis Vaccine Supply Update October 2016 This update provides information on diphtheria, tetanus, and whole cell pertussis (DTwP) vaccines and UNICEF’s long-term arrangement issuance to two manufacturers with significant production capacity. Lead times for delivery through UNICEF have now reduced to eight weeks. DTP vaccine containing acellular pertussis (DTaP) availability through UNICEF remains limited and currently unavailable through 2018. 1. Summary The DTwP vaccine market remains fragile, characterized by low-demand volumes. While multiple DTwP vaccine manufacturers of WHO prequalified DTwP exist, only two currently offer prequalified DTwP vaccine through UNICEF. DTwP vaccine lead-time for delivery from manufacturers through UNICEF has reduced from six months to eight weeks from purchase order placement, as a result of additional supply availability, and procurement no longer being dependent on a single manufacturer. However, globally, standalone DTwP vaccine availability has decreased as manufacturers allocate existing DTwP bulk to produce DTwP-containing combination vaccines, particularly pentavalent DTwP-containing combination vaccines with antigens against Hepatitis B and Haemophilus Influenzae type b. UNICEF DTwP vaccine procurement since 2012 declined from approximately 20 million doses to reach an average 5 million doses per year, mainly as countries switched to other DTwP combination vaccines. Countries continue to seek to secure access to DTaP combination vaccines through UNICEF. However, global supply availability remains very limited and currently unavailable through UNICEF. UNICEF anticipates earliest availability end 2018-2019. 2. Background & Procurement History DTP vaccines have been part of the Expanded Programme of Immunization (EPI) vaccination schedule since 1974.1 Historically, several manufacturers with sufficient supply met global DTP vaccine demand. -

Alex Haslam Is a Social Psychologist and an Australian Laureate Fellow at the University of Queensland, Australia
Alex Haslam is a social psychologist and an Australian Laureate Fellow at the University of Queensland, Australia. He is also a Senior Fellow of CIFAR’s Social Interactions, Identity & Well-Being program. His work examines how social identities and group memberships influence our interactions with others. He researches such questions as: How does belonging to groups and organizations shape the way we think, feel and behave? And how do individuals and groups in turn shape the nature of organizations and society? Dr. Haslam approaches these questions by identifying and explaining how people’s membership in groups and teams affects a range of social and organizational processes including stereotyping and prejudice, leadership and motivation, communication and decision-making, and stress and mental health. Dr Haslam is on the editorial board of seven international journals, including Scientific American Mind. He has published and edited 11 books on social and organizational psychology including the seminal book The Social Cure: Identity, Health and Well-being. His work has received numerous honours including the British Psychology Society's Award for Excellence in the Teaching of Psychology, and a National Teaching Fellowship from the Higher Education Academy. John Berry is a cross-cultural psychologist, and a member of CIFAR Advisory Board for the Social Interactions, Identity, & Well-being program. His research involves two domains. First is the examination of how individual behaviour is developed and displayed in different cultural contexts; much of the work has been with Indigenous Peoples in Canada, Africa and Asia. Second is research with immigrant and ethnocultural groups who are settled into plural societies in many parts of the world.