People in Distress (Mental Health Issues)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glasgow City Community Health Partnership Service Directory 2014 Content Page
Glasgow City Community Health Partnership Service Directory 2014 Content Page About the CHP 1 Glasgow City CHP Headquarters 2 North East Sector 3 North West Sector 4 South Sector 5 Adult Protection 6 Child Protection 6 Emergency and Out-of-Hours care 6 Addictions 7 - 9 Asylum Seekers 9 Breast Screening 9 Breastfeeding 9 Carers 10 - 12 Children and Families 13 - 14 Dental and Oral Health 15 Diabetes 16 Dietetics 17 Domestic Abuse / Violence 18 Employability 19 - 20 Equality 20 Healthy Living 21 Health Centres 22 - 23 Hospitals 24 - 25 Housing and Homelessness 26 - 27 Learning Disabilities 28 - 29 Mental Health 30 - 40 Money Advice 41 Nursing 41 Physiotherapy 42 Podiatry 42 Respiratory 42 Rehabilitation Services 43 Sexual Health 44 Rape and Sexual Assault 45 Stop Smoking 45 Transport 46 Volunteering 46 Young People 47-49 Public Partnership Forum 50 Comments and Complaints 51-21 About Glasgow City Community Health Partnership Glasgow City Community Health Partnership (GCCHP) was established in November 2010 and provides a wide range of community based health services delivered in homes, health centres, clinics and schools. These include health visiting, health improvement, district nursing, speech and language therapy, physiotherapy, podiatry, nutrition and dietetic services, mental health, addictions and learning disability services. As well as this, we host a range of specialist services including: Specialist Children’s Services, Homeless Services and The Sandyford. We are part of NHS Greater Glasgow & Clyde and provide services for 584,000 people - the entire population living within the area defined by the LocalAuthority boundary of Glasgow City Council. Within our boundary, we have: 154 GP practices 136 dental practices 186 pharmacies 85 optometry practices (opticians) The CHP has more than 3,000 staff working for it and is split into three sectors which are aligned to local social work and community planning boundaries. -

Open Space Strategy Consultative Draft
GLASGOW OPEN SPACE STRATEGY CONSULTATIVE DRAFT Prepared For: GLASGOW CITY COUNCIL Issue No 49365601 /05 49365601 /05 49365601 /05 Contents 1. Executive Summary 1 2. Glasgu: The Dear Green Place 11 3. What should open space be used for? 13 4. What is the current open space resource? 23 5. Place Setting for improved economic and community vitality 35 6. Health and wellbeing 59 7. Creating connections 73 8. Ecological Quality 83 9. Enhancing natural processes and generating resources 93 10. Micro‐Climate Control 119 11. Moving towards delivery 123 Strategic Environmental Assessment Interim Environment Report 131 Appendix 144 49365601 /05 49365601 /05 1. Executive Summary The City of Glasgow has a long tradition in the pursuit of a high quality built environment and public realm, continuing to the present day. This strategy represents the next steps in this tradition by setting out how open space should be planned, created, enhanced and managed in order to meet the priorities for Glasgow for the 21st century. This is not just an open space strategy. It is a cross‐cutting vision for delivering a high quality environment that supports economic vitality, improves the health of Glasgow’s residents, provides opportunities for low carbon movement, builds resilience to climate change, supports ecological networks and encourages community cohesion. This is because, when planned well, open space can provide multiple functions that deliver numerous social, economic and environmental benefits. Realising these benefits should be undertaken in a way that is tailored to the needs of the City. As such, this strategy examines the priorities Glasgow has set out and identifies six cross‐cutting strategic priority themes for how open space can contribute to meeting them. -

This Is the Title. It Is Arial 16Pt Bold
Green Flag Award Park Winners 2017 Local Authority Park Name New Aberdeen City Council Duthie Park Aberdeen City Council Hazlehead Park Aberdeen City Council Johnston Gardens Y Aberdeen City Council Seaton Park Aberdeenshire Council Aden Country Park Aberdeenshire Council Haddo Park Dumfries & Galloway Council Dock Park Dundee City Council Barnhill Rock Garden Dundee City Council Baxter Park Trottick Mill Ponds Local Nature Dundee City Council Reserve Dundee City Council Dundee Law Y Dundee City Council Templeton Woods East Renfrewshire Council Rouken Glen Park Edinburgh Braidburn Valley Park Edinburgh Burdiehouse Burn Valley Park Edinburgh Corstorphine Hill Edinburgh Craigmillar Castle Park Edinburgh Easter Craiglockhart Hill Edinburgh Ferniehill Community Park Edinburgh Ferry Glen & Back Braes Edinburgh Figgate Burn Park www.keepscotlandbeautiful.org 1 Edinburgh Hailes Quarry Park Edinburgh Harrison Park Hermitage of Braid inc Blackford Hill Edinburgh & Pond Edinburgh Hopetoun Crescent Gardens Edinburgh Inverleith Park Edinburgh King George V Park, Eyre Place Edinburgh Lochend Park Edinburgh London Road Gardens Edinburgh Morningside Park Edinburgh Muirwood Road Park Edinburgh Pentland Hills Regional Park Edinburgh Portobello Community Garden Edinburgh Prestonfield Park Edinburgh Princes Street Gardens Edinburgh Ravelston Park & Woods Edinburgh Rosefield Park Edinburgh Seven Acre Park Edinburgh Spylaw Park Edinburgh St Margarets Park Edinburgh Starbank Park Edinburgh Station Road Pk, S Queensferry Edinburgh Victoria Park Falkirk Community -
Fare4all? Report of the Enquiry Into Public Transport in Glasgow
Fare4All? Report of the Enquiry into Public Transport in Glasgow March 2006 Contents Fare4All? Steering Group 3 Fare4All? Key Findings 4 Fare4All? Suggestions for Improvements 5 1. Fare4All? 6 2. The Work of Fare4All? 7 3. Some Background to Bus Policy and Provision 8 Glasgow – A City Perspective Some Facts on the Communities who need to use Public Transport 4. Key Findings of the Fare4All? Survey 11 5. Perspectives of Older People 13 6. Perspectives of Parents with Children 14 7. Perspectives of People with Learning Disabilities 15 8. The Impact of Transport on Community Life: A Profile of North Glasgow 16 9. Fare4All? Transport Summit 18 10. Suggestions for Improvement 21 11. References 22 2 Fare4All? Steering Group The Fare4All? Steering Group is chaired by Paul Martin MSP. The members are: Allan Comrie Strathclyde Passenger Transport Executive Arlene Cooke North Glasgow Healthy Living Community Frank Creighton Healthy Castlemilk Irene Forrest North Area Transport Association John Halliday Strathclyde Passenger Transport Executive Fran Lundie Glasgow City Council Community Safety Department Agnes McGroarty West of Scotland Seniors’ Forum Niall McGrogan NHS Greater Glasgow Helen McNeil Glasgow Council for Voluntary Services Marie Montgomery Age Concern Jim Thompson Fair Deal Jess Thomson The Friends of the Victoria Kate Munro Community Engagement Manager, NHS Greater Glasgow Dan Harley Community Engagement Manager, NHS Greater Glasgow Mark McAllister Community Engagement Manager, NHS Greater Glasgow The content of this report reflects the views of the Fare4All? Steering Group or individual contributors and not necessarily those of any named organisation. This report is also available in large print and on-line. -

Cardowan Moss Is a Beezer Ae a Place
Scottish Scottish Lowlands Lowlands Easterhouse For more information please contact: A Beezer ae a Place Forestry Commission Scotland Cardowan Moss is a beezer ae a place. Cardowan Scottish Lowlands Forest District There’s bonnie flooers, lowpin puddocks Five Sisters House and swallows swallaein midgies. There’s Five Sisters Business Park even a china hingin aboot haufway doon Moss West Calder the path. Ye’ll no get much chat oot ae EH558PNCardowan Moss him though – the big yin’s made fae iron. Tel: 01555 660190 email:[email protected] Bishop Loch Todds Well Map 2 in a series of 5 Lochend Burn Map 2 in a series of 5 Callander Cardowan Moss STIRLINGSTIRLING R Teith Water Voles and Iron Men Dunblane R Forth WEST Alloa DUNBARTOONSHIRE Explore this network of Stirling A907 © Crown copyright and database right [2013]. well-managed trails around Ordnance Survey Licence number [100021242]. 9 A985 A875 EAST M876 M9 A811 DUNBARTONSHIRE 3 Cardowan Moss A809 8 7 A8 M80 2 1 Denny 1 and you’ll 8 6 Kilsyth 7 5 A891 4 3 find more 6 Falkirk A82 A803 M80 A801 than 5 FALKIRK West Maryston 31 Cumbernauld 4 A73 1 3 Mo Roghainn Carr Domhainn INVERCLYDE 30 beautiful M8 3 M73 A761 M8 2 2a 3 A89 3a Carr, no boglach, domhainn a bh’ ann uaireigin. 26 17 1/13 Easterhouse woodland. 15 10 4 29 25 19 M8 22 8/2 Airdrie 5 Ach an-diugh: sgaoilteachd chraobhan, flùraichean 1 A8 You might 2 3 4/1 6 Paisley 2 A7 4 ioma-dhathte, agus gille iarainn ’nan àrainn. -

Glasgow City Health and Social Care Partnership Health Contacts
Glasgow City Health and Social Care Partnership Health Contacts January 2017 Contents Glasgow City Community Health and Care Centre page 1 North East Locality 2 North West Locality 3 South Locality 4 Adult Protection 5 Child Protection 5 Emergency and Out-of-Hours care 5 Addictions 6 Asylum Seekers 9 Breast Screening 9 Breastfeeding 9 Carers 10 Children and Families 12 Continence Services 15 Dental and Oral Health 16 Dementia 18 Diabetes 19 Dietetics 20 Domestic Abuse 21 Employability 22 Equality 23 Health Improvement 23 Health Centres 25 Hospitals 29 Housing and Homelessness 33 Learning Disabilities 36 Maternity - Family Nurse Partnership 38 Mental Health 39 Psychotherapy 47 NHS Greater Glasgow and Clyde Psychological Trauma Service 47 Money Advice 49 Nursing 50 Older People 52 Occupational Therapy 52 Physiotherapy 53 Podiatry 54 Rehabilitation Services 54 Respiratory Team 55 Sexual Health 56 Rape and Sexual Assault 56 Stop Smoking 57 Volunteering 57 Young People 58 Public Partnership Forum 60 Comments and Complaints 61 Glasgow City Community Health & Care Partnership Glasgow Health and Social Care Partnership (GCHSCP), Commonwealth House, 32 Albion St, Glasgow G1 1LH. Tel: 0141 287 0499 The Management Team Chief Officer David Williams Chief Officer Finances and Resources Sharon Wearing Chief Officer Planning & Strategy & Chief Social Work Officer Susanne Miller Chief Officer Operations Alex MacKenzie Clincial Director Dr Richard Groden Nurse Director Mari Brannigan Lead Associate Medical Director (Mental Health Services) Dr Michael Smith -

Overview of Allocated Funding
Overview of allocated funding A combined total of £979,625 has been awarded to 116 community groups and workplaces through the Cycling Friendly programme with a further £821,991 awarded to registered social landlords across Scotland for improvement facilities to promote walking and cycling. More than 90,000 people will benefit from the funding. Setting Number funded Amount funded People impacted Community groups 48 £536,737 Data not collected Employers 68 £442,888 27,500 Social housing 33 £821,991 62,119 providers Total 149 £1,801,616 89,619 Kath Brough, Head of Behaviour Change at Cycling Scotland said: “We’re delighted to announce funding to 149 organisations across Scotland to encourage more people to cycle. Cycling Scotland work closely with partners to help employers, community groups and housing associations take advantage of the benefits of cycling and this round of funding will provide opportunity for over 90,000 people across Scotland to access improved cycling facilities.” Elderbank Housing Association, based in Govan, Glasgow, will receive £25,000 to install cycle parking for the 2,700 residents living across their properties, where currently there is no cycle parking. Jim Fraser, Estate Management Inspector, said “lack of storage has been a key issue for residents, especially those in older tenement buildings, so installing bike parking will remove a significant barrier to the uptake in bike ownership and cycling as a healthy activity. Govan is well established as an area of high deprivation and residents can often be found to have low household income and higher levels of household debt. This can impact greatly on people’s ability to access public transport beyond a limited geographical area and frequency due to a lack of sufficient finance. -
Campus Travel Guide Final 08092016 PRINT READY
Lochfauld V Farm ersion 1.1 27 Forth and 44 Switchback Road Maryhill F C Road 6 Clyde Canal Road Balmore 1 0 GLASGOW TRANSPORT NETWORK 5 , 6 F 61 Acre0 A d Old Blairdardie oa R Drumchapel Summerston ch lo 20 til 23 High Knightswood B irkin e K F 6 a /6A r s de F 15 n R F 8 o Netherton a High d 39 43 Dawsholm 31 Possil Forth and Clyde Canal Milton Cadder Temple Gilshochill a 38 Maryhill 4 / 4 n F e d a s d /4 r a 4 a o F e River Lambhill R B d Kelvin F a Anniesland o 18 F 9 0 R 6 n /6A 1 40 r 6 u F M 30 a b g Springburn ry n h 20 i ill r R Ruchill p Kelvindale S Scotstounhill o a Balornock 41 d Possil G Jordanhill re Park C at 19 15 W es 14 te rn R 17 37 oa Old Balornock 2 d Forth and D um Kelvinside 16 Clyde b North art 11 Canal on Kelvin t Ro Firhill ad 36 ee 5 tr 1 42 Scotstoun Hamiltonhill S Cowlairs Hyndland 0 F F n e 9 Broomhill 6 F ac 0 r Maryhill Road V , a ic 6 S Pa tor Dowanhill d r ia a k D 0 F o S riv A 8 21 Petershill o e R uth 8 F 6 n F /6 G r A a u C 15 rs b R g c o u n Whiteinch a i b r 7 d e Partickhill F 4 p /4 S F a River Kelvin F 9 7 Hillhead 9 0 7 River 18 Craighall Road Port Sighthill Clyde Partick Woodside Forth and F 15 Dundas Clyde 7 Germiston 7 Woodlands Renfrew Road 10 Dob Canal F bie' 1 14 s Loa 16 n 5 River Kelvin 17 1 5 F H il 7 Pointhouse Road li 18 5 R n 1 o g 25A a t o Shieldhall F 77 Garnethill d M 15 n 1 14 M 21, 23 10 M 17 9 6 F 90 15 13 Alexandra Parade 12 0 26 Townhead 9 8 Linthouse 6 3 F Govan 33 16 29 Blyt3hswood New Town F 34, 34a Anderston © The University of Glasgo North Stobcross Street Cardonald -

Old Mines and Mine Masters of the Monklands” British Mining No.45, NMRS, Pp.66-86
BRITISH MINING No.45 MEMOIRS 1992 Skillen, B.S. 1992 “Old Mines and Mine Masters of the Monklands” British Mining No.45, NMRS, pp.66-86. Published by the THE NORTHERN MINE RESEARCH SOCIETY SHEFFIELD U.K. © N.M.R.S. & The Author(s) 1992. ISSN 0309-2199 BRITISH MINING No.45 OLD MINES AND MINES MASTERS OF THE MONKLANDS Brian S. Skillen SYNOPSIS The Monklands lie east of Glasgow, across economically worthwhile coal measures, which have been worked to a great extent. Additionally to coal it proved possible to work a good local ironstone. Mushet’s blackband ironstone proved the resource on which the Monklands rose to prosperity in the 19th century. A pot pourri of minerals was there to be worked and their exploitation may be traced back to the 17th century. Estate feuding provides the first clue to the early coal working of the Monklands. In 1616, Muirhead of Brydanhill was in dispute with Newlands of Kip ps. Such was the animosity of feeling, that the latter turned up at the tiny coal working at Brydanhill and together with his men smashed up Muirhead’s pit head.1 It is likely that Muirhead’s mine had answered purely local needs and certainly if mining did continue it was on this ephemeral basis, at least until the mid 18th century. The reasons are easy to find, fragile local markets that offered no encouragement to invest in mining and a lack of communications that stopped any hope of export. In any case the western markets were then answered by the many small coal pits about the Glasgow district, including satellite workings such as Barrachnie on the western extremity of Old Monkland Parish. -

Download Download
Scottish Tradition Vol. 27 2002 WORKING CLASS CULTURE, FAMILY LIFE AND DOMESTIC VIOLENCE ON CLYDESIDE, C 1918-1939: A VIEW FROM BELOW. ‘People have no idea how the poor lived in those days. They seemed to be at loggerheads all the time.’ 1 he inter-war years were distinguished by marked changes that affected the lives and neighbourhoods of Tmany working class men and women. These changes would prove to have positive and negative implications for working-class family life. New employment opportunities extended the breadth of jobs open to working class people, espe- cially in the new consumer industries that employed significant numbers of women. Correspondingly, the commercialisation of leisure expanded the possibilities of pleasure. Information on birth control and the greater ease of availability of contraceptives also offered a better potential to postpone marriage and reduce family size. Yet, the new employment opportunities did little to alter the ‘pin money’ wages of women and women’s economic dependency on marriage. Marriage was still seen as an attractive alternative to employment in the longer term.2 Marriage and motherhood were actively promoted as the natural and fulfilling aspirations for women by the state, state agencies, the clergy, religious organisations and the media. Adding to the appeal was the ideal of the ‘companionate marriage’ in which husbands were expected to share chores, child-care, leisure and provide love and companionship. It seems that this was a ‘fairly norma- tive’ aspiration amongst many sectors of the working class between the wars, at least amongst women. Change, however, was not just ideological.3 After World War I, the building of ‘homes fit for heroes’ and the growth of ‘new garden cities’, were linked with ideals of the companionate marriage, maternalism, privacy, respectable domesticity and the growth of male home- centred pastimes. -

New Stobhill Hospital the New Stobhill Ambulatory Care Hospital Belmont (ACH) Is Set in the Stobhill Campus
To Bishopbriggs FIF New Stobhill station E WAY New Stobhill Hospital The New Stobhill Ambulatory Care Hospital Belmont (ACH) is set in the Stobhill campus. The campus Hospital D Centre A O houses the hospital, a minor injuries unit, a R L L Marie Curie number of general and specialist mental health Walking and cycling guide 2021 HI Hospice Y facilities, and a brand new purpose-built Marie RA G Curie Cancer Care hospice. L BA A LORNOCK ROAD B The ACH provides outpatient clinics, day surgery and diagnostic services. There are hospital beds available to medics to extend the range of short B ALORNOCK ROAD stay surgical procedures offered to patients. B A L Skye House O At the main entrance there is a staffed help desk R N O and patient information points which provide C K R travel information, health promotion and other O A D advice. BELMONT ROAD Stobhill Hospital 2 new mental health wards are now on the campus. The two wards – Elgin and Appin – have space for up to 40 inpatients, with Elgin To Springburn dedicated to adult acute mental health inpatient station care and Appin focusing on older adults with functional mental health issues. Cycle Parking Entrance Rowanbank Bus stop Clinic BALORNOCK ROAD Active Travel Cycling to Work NHS Greater Glasgow & Clyde recognise that New Stobhill Hospital is well served by public transport The Cycle to Work scheme is a salary sacrifice scheme physical activity is essential for good health covering bus travel within the immediate area and available to NHS Greater Glasgow & Clyde staff*. -
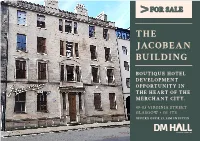
The Jacobean Building
FOR SALE THE JACOBEAN BUILDING BOUTIQUE HOTEL DEVELOPMENT OPPORTUNITY IN THE HEART OF THE MERCHANT CITY. 49-53 VIRGINIA STREET GLASGOW • G1 1TS OFFERS OVER £1.33M INVITED THE JACOBEAN BUILDING This Grade A listed building dates back to as far as • Rare hotel development 1760 in the times of wealthy merchants in Glasgow opportunity. such as Speirs, Buchanan and Bowmen. Whilst in more recent times it has been used for traditional • Full planning consent commercial purposes these have included yoga granted. studios, offices and for a cookery school. • Within the chic The accommodation is arranged over basement, Merchant City. ground and three upper floors and benefits from a very attractive courtyard to the rear. Within • Offers over £1.33M its current ownership, the building has been invited for the freehold consistently maintained and upgraded since the interest. early 1990s. The main entrance is taken from Virginia Street. The property is on the fringe of the vibrant Merchant City area, with its diverse mix of retailing, pubs, restaurant and residential accommodation much of which has been developed over recent years to include flats for purchase and letting plus serviced apartments. DEVELOPER’S PLANNING PACK The subjects are Category A listed. Full planning permission has been granted for bar and restaurant Our client has provided us with an extensive uses for the ground and basement as well for 18 information pack on the history of the building boutique style hotel rooms to be developed above as well as the planning consents now in place. The on the upper floors. Full information and plans are following documents are available, available on Glasgow City Council’s Planning Portal with particular reference to application numbers - Package of the planning permissions 18/01725/FUL and 18/01726/LBA.