Selection of Vasodilator Therapy for Severe Raynaud's Phenomenon by Sequential Arterial Infusion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Index Vol. 12-15
353 INDEX VOL. 12-15 Die Stichworte des Sachregisters sind in der jeweiligen Sprache der einzelnen Beitrage aufgefiihrt. Les termes repris dans la Table des matieres sont donnes selon la langue dans laquelle l'ouvrage est ecrit. The references of the Subject Index are given in the language of the respective contribution. 14 AAG (Alpha-acid glycoprotein) 120 14 Adenosine 108 12 Abortion 151 12 Adenosine-phosphate 311 13 Abscisin 12, 46, 66 13 Adenosine-5'-phosphosulfate 148 14 Absorbierbarkeit 317 13 Adenosine triphosphate 358 14 Absorption 309, 350 15 S-Adenosylmethionine 261 13 Absorption of drugs 139 13 Adipaenin (Spasmolytin) 318 14 - 15 12 Adrenal atrophy 96 14 Absorptionsgeschwindigkeit 300, 306 14 - 163, 164 14 Absorptionsquote 324 13 Adrenal gland 362 14 ACAI (Anticorticocatabolic activity in 12 Adrenalin(e) 319 dex) 145 14 - 209, 210 12 Acalo 197 15 - 161 13 Aceclidine (3-Acetoxyquinuclidine) 307, 13 {i-Adrenergic blockers 119 308, 310, 311, 330, 332 13 Adrenergic-blocking activity 56 13 Acedapsone 193,195,197 14 O(-Adrenergic blocking drugs 36, 37, 43 13 Aceperone (Acetabutone) 121 14 {i-Adrenergic blocking drugs 38 12 Acepromazin (Plegizil) 200 14 Adrenergic drugs 90 15 Acetanilid 156 12 Adrenocorticosteroids 14, 30 15 Acetazolamide 219 12 Adrenocorticotropic hormone (ACTH) 13 Acetoacetyl-coenzyme A 258 16,30,155 12 Acetohexamide 16 14 - 149,153,163,165,167,171 15 1-Acetoxy-8-aminooctahydroindolizin 15 Adrenocorticotropin (ACTH) 216 (Slaframin) 168 14 Adrenosterone 153 13 4-Acetoxy-1-azabicyclo(3, 2, 2)-nonane 12 Adreson 252 -

Adrenoceptors Regulating Cholinergic Activity in the Guinea-Pig Ileum 1978) G.M
- + ! ,' Br. J. Pharmac. (1978), 64, 293-300. F'(O t.,," e reab- ,ellular PHARMACOLOGICAL CHARACTERIZATION OF THE PRESYNAPTIC _-ADRENOCEPTORS REGULATING CHOLINERGIC ACTIVITY IN THE GUINEA-PIG ILEUM 1978) G.M. Departmentof Pharmacology,Allen and HzmburysResearchLimited, Ware, Hertfordshire,SG12 ODJ I The presynaptic ct-adrenoceptors located on the terminals of the cholinergic nerves of the guinea- pig myenteric plexus have been characterized according to their sensitivities to at-adrenoceptor agonists and antagonists. 2 Electrical stimulation of the cholinergic nerves supplying the longitudinal muscle of the guinea-pig ! ileum caused a twitch response. Clonidine caused a concentration-dependent inhibition of the twitch i response; the maximum inhibition obtained was 80 to 95_o of the twitch response. Oxymetazoline and xylazine were qualitatively similar to clonidine but were about 5 times less potent. Phenylephrine and methoxamine also inhibited the twitch response but were at least 10,000 times less potent than clonidine. 3 The twitch-inhibitory effects of clonidine, oxymetazoline and xylazine, but not those of phenyl- ephrine or methoxamine, were reversed by piperoxan (0.3 to 1.0 lag/ml). 4 Lysergic acid diethylamide (LSD) inhibited the twitch response, but also increased the basal tone of the ileum. Mepyramine prevented the increase in tone but did not affect the inhibitory action of LSD. Piperoxan or phentolamine only partially antagonized the inhibitory effect of LSD. 5 Phentolamine, yohimbine, piperoxan and tolazoline were potent, competitive antagonists of the inhibitory effect of clonidine with pA2 values of 8.51, 7.78, 7.64 and 6.57 respectively. 6 Thymoxamine was a weak antagonist of clonidine; it also antagonized the twitch-inhibitory effect of morphine. -
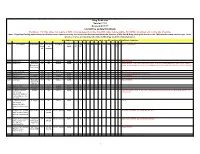
Drug Code List Version 11.2 Revised 9/11/17 List Will Be Updated Routinely
Drug Code List Version 11.2 Revised 9/11/17 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.hhs.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI IDT DC Special Instructions Requir of Limits OP OP F ed measure 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. 90296 diphtheria antitoxin No ML NONE X X X X 90371 hep b ig, im Bayhep B, Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -
![With [3H]Mepyramine (Trieyclic Antidepressants/Antihistamine/Neurotransmitter/Amitriptyline) VINH TAN TRAN, RAYMOND S](https://docslib.b-cdn.net/cover/2862/with-3h-mepyramine-trieyclic-antidepressants-antihistamine-neurotransmitter-amitriptyline-vinh-tan-tran-raymond-s-1512862.webp)
With [3H]Mepyramine (Trieyclic Antidepressants/Antihistamine/Neurotransmitter/Amitriptyline) VINH TAN TRAN, RAYMOND S
Proc. Nati. Acad. Sci. USA Vol. 75, No. 12, pp. 6290-6294,, December 1978 Neurobiology Histamine H1 receptors identified in mammalian brain membranes with [3H]mepyramine (trieyclic antidepressants/antihistamine/neurotransmitter/amitriptyline) VINH TAN TRAN, RAYMOND S. L. CHANG, AND SOLOMON H. SNYDER* Departments of Pharmacology and Experimental Therapeutics, and Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205 Communicated by Julius Axelrod, August 30,1978 ABSTRACT The antihistamine [3H mepyramine binds to Male Sprague-Dawley rats (150-200 g) were killed by cer- HI histamine receptors in mammalian brain membranes. vical dislocation, their brains were rapidly removed and ho- Potencies of H1 antihistamines at the binding sites correlate mogenized with a Polytron for 30 min (setting 5) in 30 vol of with their pharmacological antihistamine effects in the guinea pig ileum. Specific [3Himepyramine binding is saturable with ice-cold Na/K phosphate buffer (50 mM, pH 7.5), and the a dissociation constant of about 4 nM in both equilibrium and suspension was centrifuged (50,000 X g for 10 min). The pellet kinetic experiments and a density of 10pmolper gram ofwhole was resuspended in the same volume of fresh buffer and cen- brain. Some tricyclic antidepressants are potent inhibitors of trifuged, and the final pellet was resuspended in the original secific [3Hmepamine binding. Regional variations of volume of ice-cold buffer by Polytron homogenization. Calf [3Hjmepyramine ing do not correlate with variations in brains were obtained from a local abattoir within 2 hr after the endogeneous histamine and histidine decarboxylase activity. death of the animals and transferred to the laboratory in ice- Histamine is a neurotransmitter candidate in mammalian brain cold saline. -

Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01 -

Redalyc.Effcts of Cassia Podocarpa Leaves Extracts on the Rat Ileum And
Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas ISSN: 0717-7917 [email protected] Universidad de Santiago de Chile Chile Akomolafe, R.O.; Adeoshun, I.O.; Elujoba, A. A.; Iwalewa, E.O.; Ayoka, A.O. Effcts of cassia podocarpa leaves extracts on the rat ileum and colon (in vitro) Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas, vol. 3, núm. 3, mayo, 2004, pp. 52-57 Universidad de Santiago de Chile Santiago, Chile Available in: http://www.redalyc.org/articulo.oa?id=85630303 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative BLACPMA Vol. 3 Nº 3 Mayo 2004 52 ARTICULOS stimulated by the extract. With this results therefore, C. podocarpa leaves could be EFFCTS OF CASSIA PODOCARPA substituted for C. acutifolia leaves as LEAVES EXTRACTS ON THE RAT vegetable laxative. ILEUM AND COLON (IN VITRO) KEY WORDS: Motility, Anthraquinone, Allosteric activation. 2* 1 R.O. AKOMOLAFE , I.O. ADEOSHUN , 3 4 A.A. ELUJOBA , E.O. IWALEWA RESUMEN: La etnofarmacología y los AND informes científicos indican el uso hojas de C. 1 A.O. AYOKA podocarpa como purgante. Este estudio intenta encontrar el efecto in vitro de su Recibido: 16 May 2003 infusión ácuosa (ACPL) y los methanolic Recibido corregido: 1 September 2003 (MCPL) en el intestines de ratas, usando Aceptado: 30 November 2003 hojas de C. acutifolia (ACAL y MCAL) como la norma de la referencia. -

Xylazine Tolazoline
United States Department of Agriculture Agricultural Marketing Service | National Organic Program Document Cover Sheet https://www.ams.usda.gov/rules-regulations/organic/national-list/petitioned Document Type: ☐ National List Petition or Petition Update A petition is a request to amend the USDA National Organic Program’s National List of Allowed and Prohibited Substances (National List). Any person may submit a petition to have a substance evaluated by the National Organic Standards Board (7 CFR 205.607(a)). Guidelines for submitting a petition are available in the NOP Handbook as NOP 3011, National List Petition Guidelines. Petitions are posted for the public on the NOP website for Petitioned Substances. ☒ Technical Report A technical report is developed in response to a petition to amend the National List. Reports are also developed to assist in the review of substances that are already on the National List. Technical reports are completed by third-party contractors and are available to the public on the NOP website for Petitioned Substances. Contractor names and dates completed are available in the report. Xylazine/Tolazoline Livestock 1 2 Identification of Petitioned Substance 3 4 Chemical Names: 43 5 Xylazine 44 Trade Names: 6 Xylazine 45 Xylazine 7 Xylazine Hydrochloride 46 AnaSed® LA 8 Xylazine Monohydrochloride 47 Rompun® 9 N-(2,6-Diphenylmethyl)-5,6-dihydro-4H-1,3- 48 TranquiVed Injection 10 thiazin-2-amine 49 X-Ject SA 11 N-(2,6-Diphenylmethyl)-5,6-dihydro-4H-1,3- 50 XylaMed™Celactal 12 thiazin-2-amine hydrochloride 51 13 52 -
Drugs, Poisons and Controlled Substances Act 1981
1834 ANNO TRICESIMO ELIZABETHAE SECUNDAE REGINAE VICTORIA Drugs, Poisons and Controlled Substances Act 1981 No. 9719 An Act to re-enact with Amendments the Law relating to Drugs, Poisons and Controlled Substances, to amend the Health Act 1958 and the Crimes Act 1958 and for other purposes. [Assented to 12 January 1982] BE IT ENACTED by the Queen's Most Excellent Majesty by and with the advice and consent of the Legislative Council and the Legislative Assembly of Victoria in this present ParUament assembled and by the authority of the same as follows (that is to say): Short tiUe. 1. (1) This Act may be cited as the Drugs, Poisons and Controlled Substances y4cM981. Commenco- (2) The several provisions of this Act shall come into operation ment. on a day or on the respective days to be fixed by proclamation or successive proclamations of the Governor in Council published in the Government Gazette. Arrangement (3) This Act is divided into Parts and Divisions as follows: of Act. Part I.—Introductory and Transitional ss. 2-11. Part II.—Poisons and Controlled Substances ss. 12-55. Division 1—Classification s. 12. Division 2—Authorized Persons ss. 13-14. Division 1981 Drugs, Poisons and Controlled Substances No. 9719 2335 Division 3—Poisons Advisory Committee ss. 15-18. Division 4—Licensed Persons s. 19. Division 5—Special Poisons s. 20. Division 6—Industrial, Educational and Laboratory Permits s. 21. Division 7—Issue of Licences and Permits s. 22. Division 8—Manufacture and Sale of Poisons or . Controlled Substances ss. 23-30. Division 9—Trade or Proprietary Poisons s. -

Mitigating the Inhibition of Human Bile Salt Export Pump by Drugs
DMD Fast Forward. Published on September 7, 2012 as DOI: 10.1124/dmd.112.047068 DMD FastThis Forward. article has not Published been copyedited on andSeptember formatted. The 7, final 2012 version as doi:10.1124/dmd.112.047068may differ from this version. DMD #47968 Mitigating the inhibition of human Bile Salt Export Pump by drugs: opportunities provided by physicochemical property modulation, in-silico modeling and structural modification Daniel J. Warner, Hongming Chen, Louis-David Cantin, J. Gerry Kenna, Simone Stahl, Clare L. Walker, Tobias Noeske. Department of Medicinal Chemistry, AstraZeneca R&D Montreal, Montreal, Quebec, H4S Downloaded from 1Z9, Canada (DJW, LDC) Computational Sciences, Discovery Sciences, AstraZeneca R&D Mölndal, Pepparedsleden dmd.aspetjournals.org 1, Mölndal 43183, Sweden (HC) Molecular Toxicology, Global Safety Assessment, AstraZeneca, Alderley Park, Macclesfield, Cheshire, SK10 4TG, UK (JGK, SS, CLW) Global Safety Assessment, AstraZeneca R&D Mölndal, Pepparedsleden 1, Mölndal 43183, at ASPET Journals on October 10, 2021 Sweden (TN) 1 Copyright 2012 by the American Society for Pharmacology and Experimental Therapeutics. DMD Fast Forward. Published on September 7, 2012 as DOI: 10.1124/dmd.112.047068 This article has not been copyedited and formatted. The final version may differ from this version. DMD #47968 Inhibition of the human Bile Salt Export Pump by drugs. Corresponding author: Tobias Noeske Global Safety Assessment AstraZeneca R&D Mölndal S-431 83 Mölndal, Sweden Phone: +46-31-7064002 Mobile: +46-727-158344 -

PRESYNAPTIC O-ADRENOCEPTORS REGULATING CHOLINERGIC ACTIVITY in the GUINEA-PIG ILEUM
Br. J. Pharmac. (1978), 64, 293-300. PHARMACOLOGICAL CHARACTERIZATION OF THE PRESYNAPTIC o-ADRENOCEPTORS REGULATING CHOLINERGIC ACTIVITY IN THE GUINEA-PIG ILEUM G.M. DREW Department of Pharmacology, Allen and Hanburys Research Limited, Ware, Hertfordshire, SG12 ODJ 1 The presynaptic ax-adrenoceptors located on the terminals of the cholinergic nerves of the guinea- pig myenteric plexus have been characterized according to their sensitivities to a-adrenoceptor agonists and antagonists. 2 Electrical stimulation of the cholinergic nerves supplying the longitudinal muscle of the guinea-pig ileum caused a twitch response. Clonidine caused a concentration-dependent inhibition of the twitch response; the maximum inhibition obtained was 80 to 95% of the twitch response. Oxymetazoline and xylazine were qualitatively similar to clonidine but were about 5 times less potent. Phenylephrine and methoxamine also inhibited the twitch response but were at least 10,000 times less potent than clonidine. 3 The twitch-inhibitory effects of clonidine, oxymetazoline and xylazine, but not those of phenyl- ephrine or methoxamine, were reversed by piperoxan (0.3 to 1.0 jg/ml). 4 Lysergic acid diethylamide (LSD) inhibited the twitch response, but also increased the basal tone of the ileum. Mepyramine prevented the increase in tone but did not affect the inhibitory action of LSD. Piperoxan or phentolamine only partially antagonized the inhibitory effect of LSD. 5 Phentolamine, yohimbine, piperoxan and tolazoline were potent, competitive antagonists of the inhibitory effect of clonidine with pA2 values of 8.51, 7.78, 7.64 and 6.57 respectively. 6 Thymoxamine was a weak antagonist of clonidine; it also antagonized the twitch-inhibitory effect of morphine. -

The Blocking Effects of Tolazoline and Propranolol on Axial Movements of Incisor Teeth and on Changes in Arterial Blood Pressure Induced by Adrenaline in Rats
Jpn. J. Oral Biol.,40: 497-505, 1998. ORIGINAL The blocking effects of tolazoline and propranolol on axial movements of incisor teeth and on changes in arterial blood pressure induced by adrenaline in rats Hiroko Yamazaki and Shizuyo Yamaguchi Department of Pharmacology, School of Dental Medicine, Tsurumi University 2-1-3 Tsurumi, Tsurumi-ku, Yokohama 230-8501, Japan 〔Received on June 26, 1998; Accepted on August 3, 1998〕 Key words: adrenaline/adrenergic blocker/tooth movement/rat incisor/blood pressure Abstract: Axial tooth movements and arterial blood pressure were measured following intravenous injec- tion of adrenaline,1hr before, and 1 and 2hr after the injection of tolazoline (an α-adrenergic blocking agent) or propranolol (a β-adrenergic blocking agent). The initial increase in blood pressure induced by adrenaline was significantly suppressed and the successive decrease in blood pressure was markedly enhanced by pretreatment with tolazoline. In contrast to blood pressure changes, the initial extrusive tooth movement induced by adrenaline was not suppressed, and successive intrusive tooth movements induced by adrenaline were not potentiated, but suppressed. The initial increase in blood pressure induced by adrenaline was enhanced and the successive decrease in blood pressure was suppressed by pretreatment with pro- pranolol. On the other hand, the initial extrusive tooth movement induced by adrenaline was not significantly potentiated, but successive intnsive tooth movements induced by adrenaline were markedly suppressed. Pressure within the socket that may induce axial tooth movements might be regulated by various factors, such as resistance of the blood vessels, blood flow in the socket, and systemic arterial blood pressure, all of which are liable to change following an injection of adrenaline under the influence of α-or β-adrenergic blockers.