Scientific Advisory Board
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medicine with Deeper, More Biochemical Conception Of
Edinburgh Medical Journal May 1951 APPLICATIONS of chemical defence research IN MEDICINET? By Professor R. A. PETERS to be invited It is a great responsibility, as well as a great honour, to Cameron lecturers give this lecture ; and I expect that with other I this ancient seat of share a sense of awe upon standing here in is learning. For me it is an awe tinged with much feeling (it possible that this is partly because some forebears of my mother came from near to recent of the this ; it is in part due the perusal city) perhaps " address here Froude in on the Times of John Knox, given by 1865 " " entitled Influence of the Reformation upon the Scottish Character ; this address drives home to the Sassenach the sterner stuff of which all of us in the the Scots are made ; but I really think it is more that as south, even if we come as I do from a Medical School as ancient the Hospital of St Bartholomew, know full well that Edinburgh stands high indeed in the world of Medical Schools as Scotland itself stands in the world of intellect. Elsewhere I have discussed fully the historical background of our for me back researches upon Chemical Defence substances, which go to World War I.23 Again in my Dixon lecture,24 I have indicated some of the interest for pharmacology. The outlook for medicine has not the been reviewed so far. Therefore I propose to-day to discuss of British influence upon the future of therapeutics of the discovery anti-lewisite and of some of the other researches upon war gas but substances ; and to consider not only the leads towards therapy, the possible newer trends given to medicine itself. -

Decision-Making in Chemical Warfare Agent (CWA) Response There Is a Lot of Fear Associated with Chemical Will Act Accordingly
Application Note: 102 Decision-Making in Chemical Warfare Agent (CWA) Response There is a lot of fear associated with Chemical will act accordingly. If the first responders Warfare Agents (CWAs). The misnomer over-react and immediately jump into full “Nerve Gas” quickly brings horrible images to encapsulation protection it could panic the the minds of many civilians. But if we lay aside public and cause unnecessary worry and the politics and fear, CWA detection should even injury. treated like other gas/vapor detection challenges. It should be a collaborative Over Protection Can Be Dangerous process encompassing physical clues, threat to the Responder scenario, biological clues, and a variety of Heat stress is the number one injury in sensing technologies. No one clue or HazMat response and immediately jumping technology is always correct. Experience and into full Level A encapsulation is a good way the use of multiple clues and technologies are of overheating oneself. Level A the keys to successful CWA response. encapsulation also makes one much more Understanding what the clues are and how to susceptible to slip, trip and fall injuries. layer them to make a decision is critical to Finally, over protection makes it harder to get successful CWA response. things done. When properly used, detection allows responders to respond at lower levels Why is Gas Detection Important? of Personal Protective Equipment (PPE) to Responders cannot rely on their senses for provide the highest levels of safety to decision-making. Without effectively knowing themselves and to the community that they how to use detection techniques responders protect. -
Warning: the Following Lecture Contains Graphic Images
What the новичок (Novichok)? Why Chemical Warfare Agents Are More Relevant Than Ever Matt Sztajnkrycer, MD PHD Professor of Emergency Medicine, Mayo Clinic Medical Toxicologist, Minnesota Poison Control System Medical Director, RFD Chemical Assessment Team @NoobieMatt #ITLS2018 Disclosures In accordance with the Accreditation Council for Continuing Medical Education (ACCME) Standards, the American Nurses Credentialing Center’s Commission (ANCC) and the Commission on Accreditation for Pre-Hospital Continuing Education (CAPCE), states presenters must disclose the existence of significant financial interests in or relationships with manufacturers or commercial products that may have a direct interest in the subject matter of the presentation, and relationships with the commercial supporter of this CME activity. The presenter does not consider that it will influence their presentation. Dr. Sztajnkrycer does not have a significant financial relationship to report. Dr. Sztajnkrycer is on the Editorial Board of International Trauma Life Support. Specific CW Agents Classes of Chemical Agents: The Big 5 The “A” List Pulmonary Agents Phosgene Oxime, Chlorine Vesicants Mustard, Phosgene Blood Agents CN Nerve Agents G, V, Novel, T Incapacitating Agents Thinking Outside the Box - An Abbreviated List Ammonia Fluorine Chlorine Acrylonitrile Hydrogen Sulfide Phosphine Methyl Isocyanate Dibotane Hydrogen Selenide Allyl Alcohol Sulfur Dioxide TDI Acrolein Nitric Acid Arsine Hydrazine Compound 1080/1081 Nitrogen Dioxide Tetramine (TETS) Ethylene Oxide Chlorine Leaks Phosphine Chlorine Common Toxic Industrial Chemical (“TIC”). Why use it in war/terror? Chlorine Density of 3.21 g/L. Heavier than air (1.28 g/L) sinks. Concentrates in low-lying areas. Like basements and underground bunkers. Reacts with water: Hypochlorous acid (HClO) Hydrochloric acid (HCl). -

Medical Aspects of Chemical Warfare
Medical Diagnostics Chapter 22 MEDICAL DIAGNOSTICS † ‡ § BENEDICT R. CAPACIO, PHD*; J. RICHARD SMITH ; RICHARD K. GORDON, PHD ; JULIAN R. HAIGH, PHD ; JOHN ¥ ¶ R. BARR, PHD ; AND GENNADY E. PLATOFF JR, PHD INTRODUCTION NERVE AGENTS SULFUR MUSTARD LEWISITE CYANIDE PHOSGENE 3-QUINUCLIDINYL BENZILATE SAMPLE CONSIDERATIONS Summary * Chief, Medical Diagnostic and Chemical Branch, Analytical Toxicology Division, US Army Medical Research Institute of Chemical Defense, 3100 Rickets Point Road, Aberdeen Proving Ground, Maryland 21010-5400 † Chemist, Medical Diagnostic and Chemical Branch, Analytical Toxicology Division, US Army Medical Research Institute of Chemical Defense, 3100 Rickets Point Road, Aberdeen Proving Ground, Maryland 21010-5400 ‡ Chief, Department of Biochemical Pharmacology, Biochemistry Division, Walter Reed Army Institute of Research, 503 Robert Grant Road, Silver Spring, Maryland 20910-7500 § Research Scientist, Department of Biochemical Pharmacology, Biochemistry Division, Walter Reed Army Institute of Research, 503 Robert Grant Road, Silver Spring, Maryland 20910-7500 ¥ Lead Research Chemist, Centers for Disease Control and Prevention, 4770 Buford Highway, Mailstop F47, Atlanta, Georgia 30341 ¶ Colonel, US Army (Retired); Scientific Advisor, Office of Biodefense Research, National Institute of Allergies and Infectious Disease, National Institutes of Health, 6610 Rockledge Drive, Room 4069, Bethesda, Maryland 20892-6612 691 Medical Aspects of Chemical Warfare INTRODUCTION In the past, issues associated with chemical war- an -

744 Hydrolysis of Chiral Organophosphorus Compounds By
[Frontiers in Bioscience, Landmark, 26, 744-770, Jan 1, 2021] Hydrolysis of chiral organophosphorus compounds by phosphotriesterases and mammalian paraoxonase-1 Antonio Monroy-Noyola1, Damianys Almenares-Lopez2, Eugenio Vilanova Gisbert3 1Laboratorio de Neuroproteccion, Facultad de Farmacia, Universidad Autonoma del Estado de Morelos, Morelos, Mexico, 2Division de Ciencias Basicas e Ingenierias, Universidad Popular de la Chontalpa, H. Cardenas, Tabasco, Mexico, 3Instituto de Bioingenieria, Universidad Miguel Hernandez, Elche, Alicante, Spain TABLE OF CONTENTS 1. Abstract 2. Introduction 2.1. Organophosphorus compounds (OPs) and their toxicity 2.2. Metabolism and treatment of OP intoxication 2.3. Chiral OPs 3. Stereoselective hydrolysis 3.1. Stereoselective hydrolysis determines the toxicity of chiral compounds 3.2. Hydrolysis of nerve agents by PTEs 3.2.1. Hydrolysis of V-type agents 3.3. PON1, a protein restricted in its ability to hydrolyze chiral OPs 3.4. Toxicity and stereoselective hydrolysis of OPs in animal tissues 3.4.1. The calcium-dependent stereoselective activity of OPs associated with PON1 3.4.2. Stereoselective hydrolysis commercial OPs pesticides by alloforms of PON1 Q192R 3.4.3. PON1, an enzyme that stereoselectively hydrolyzes OP nerve agents 3.4.4. PON1 recombinants and stereoselective hydrolysis of OP nerve agents 3.5. The activity of PTEs in birds 4. Conclusions 5. Acknowledgments 6. References 1. ABSTRACT Some organophosphorus compounds interaction of the racemic OPs with these B- (OPs), which are used in the manufacturing of esterases (AChE and NTE) and such interactions insecticides and nerve agents, are racemic mixtures have been studied in vivo, ex vivo and in vitro, using with at least one chiral center with a phosphorus stereoselective hydrolysis by A-esterases or atom. -

Enzymatic Degradation of Organophosphorus Pesticides and Nerve Agents by EC: 3.1.8.2
catalysts Review Enzymatic Degradation of Organophosphorus Pesticides and Nerve Agents by EC: 3.1.8.2 Marek Matula 1, Tomas Kucera 1 , Ondrej Soukup 1,2 and Jaroslav Pejchal 1,* 1 Department of Toxicology and Military Pharmacy, Faculty of Military Health Sciences, University of Defence, Trebesska 1575, 500 01 Hradec Kralove, Czech Republic; [email protected] (M.M.); [email protected] (T.K.); [email protected] (O.S.) 2 Biomedical Research Center, University Hospital Hradec Kralove, Sokolovska 581, 500 05 Hradec Kralove, Czech Republic * Correspondence: [email protected] Received: 26 October 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: The organophosphorus substances, including pesticides and nerve agents (NAs), represent highly toxic compounds. Standard decontamination procedures place a heavy burden on the environment. Given their continued utilization or existence, considerable efforts are being made to develop environmentally friendly methods of decontamination and medical countermeasures against their intoxication. Enzymes can offer both environmental and medical applications. One of the most promising enzymes cleaving organophosphorus compounds is the enzyme with enzyme commission number (EC): 3.1.8.2, called diisopropyl fluorophosphatase (DFPase) or organophosphorus acid anhydrolase from Loligo Vulgaris or Alteromonas sp. JD6.5, respectively. Structure, mechanisms of action and substrate profiles are described for both enzymes. Wild-type (WT) enzymes have a catalytic activity against organophosphorus compounds, including G-type nerve agents. Their stereochemical preference aims their activity towards less toxic enantiomers of the chiral phosphorus center found in most chemical warfare agents. Site-direct mutagenesis has systematically improved the active site of the enzyme. These efforts have resulted in the improvement of catalytic activity and have led to the identification of variants that are more effective at detoxifying both G-type and V-type nerve agents. -
Chapter 6 PRETREATMENT for NERVE AGENT EXPOSURE
Pretreatment for Nerve Agent Exposure Chapter 6 PRETREATMENT FOR NERVE AGENT EXPOSURE MICHAEL A. DUNN, M.D., FACP*; BRENNIE E. HACKLEY, JR., PH.D.†; AND FREDERICK R. SIDELL, M.D.‡ INTRODUCTION AGING OF NERVE AGENT–BOUND ACETYLCHOLINESTERASE PYRIDOSTIGMINE, A PERIPHERALLY ACTING CARBAMATE COMPOUND Efficacy Safety Wartime Use Improved Delivery CENTRALLY ACTING NERVE AGENT PRETREATMENTS NEW DIRECTIONS: BIOTECHNOLOGICAL PRETREATMENTS SUMMARY *Colonel, Medical Corps, U.S. Army; Director, Clinical Consultation, Office of the Assistant Secretary of Defense (Health Affairs), Washing- ton, D.C. 20301-1200; formerly, Commander, U.S. Army Medical Research Institute of Chemical Defense, Aberdeen Proving Ground, Mary- land 21010-5425 †Scientific Advisor, U.S. Army Medical Research Institute of Chemical Defense, Aberdeen Proving Ground, Maryland 21010-5425 ‡Formerly, Chief, Chemical Casualty Care Office, and Director, Medical Management of Chemical Casualties Course, U.S. Army Medical Research Institute of Chemical Defense, Aberdeen Proving Ground, Maryland 21010-5425; currently, Chemical Casualty Consultant, 14 Brooks Road, Bel Air, Maryland 21014 181 Medical Aspects of Chemical and Biological Warfare INTRODUCTION Nerve agents are rapidly acting chemical com- cal as well and may impair physical and mental pounds that can cause respiratory arrest within performance. A pretreatment must be administered minutes of absorption. Their speed of action im- to an entire force under a nerve agent threat. Any poses a need for rapid and appropriate reaction by resulting performance decrement, even a compara- exposed soldiers, their buddies, or medics, who tively minor one, would make pretreatment use must administer antidotes quickly enough to save unacceptable in battlefield situations requiring lives. A medical defense against nerve agents that maximum alertness and performance for survival. -
Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L
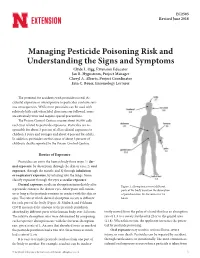
EC2505 Revised June 2018 Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L. Ogg, Extension Educator Jan R. Hygnstrom, Project Manager Cheryl A. Alberts, Project Coordinator Erin C. Bauer, Entomology Lecturer The potential for accidents with pesticides is real. Ac- cidental exposure or overexposure to pesticides can have seri- ous consequences. While most pesticides can be used with relatively little risk when label directions are followed, some are extremely toxic and require special precautions. The Poison Control Centers receive about 90,000 calls each year related to pesticide exposures. Pesticides are re- sponsible for about 3 percent of all accidental exposures to children 5 years and younger and about 4 percent for adults. In addition, pesticides are the cause of about 3 percent of children’s deaths reported to the Poison Control Centers. Routes of Exposure Pesticides can enter the human body three ways: 1) der- mal exposure, by absorption through the skin or eyes; 2) oral exposure, through the mouth; and 3) through inhalation or respiratory exposure, by inhaling into the lungs. Some classify exposure through the eyes as ocular exposure. Dermal exposure results in absorption immediately after Figure 1. Absorption rates of different a pesticide contacts the skin or eyes. Absorption will contin- parts of the body based on the absorption ue as long as the pesticide remains in contact with the skin or of parathion into the forearm over 24 eyes. The rate at which dermal absorption occurs is different hours. for each part of the body (Figure 1). Maiback and Feldman (1974) measured the amount of the pesticide parathion absorbed by different parts of the human body over 24 hours. -

Things to Be Done
DRAFT MAY 2003 ANNEX 1: CHEMICAL AGENTS 1. Introduction The large-scale use of toxic chemicals as weapons first became possible during the First World War (1914–1918) thanks to the growth of the chemical industry. More than 110 000 tonnes were disseminated over the battlefields, the greater part on the western front. Initially, the chemicals were used, not to cause casualties in the sense of putting enemy combatants out of action, but rather to harass. Though the sensory irritants used were powerful enough to disable those who were exposed to them, they served mainly to drive enemy combatants out of the trenches or other cover that protected them from conventional fire, or to disrupt enemy artillery or supplies. About 10% of the total tonnage of chemical warfare agents used during the war were chemicals of this type, namely lacrimators (tear gases), sternutators and vomiting agents. However, use of more lethal chemicals soon followed the introduction of disabling chemicals. In all, chemical agents caused some 1.3 million casualties, including 90 000 deaths. During the First World War, almost every known noxious chemical was screened for its potential as a weapon, and this process was repeated during the Second World War (1939–1945), when substantial stocks of chemical weapons were accumulated, although rarely used in military operations. Between the two world wars, a high proportion of all the new compounds that had been synthesized, or isolated from natural materials, were examined to determine their utility as lethal or disabling chemical weapons. After 1945, these systematic surveys continued, together with a search for novel agents based on advances in biochemistry, toxicology and pharmacology. -
2020 Emergency Response Guidebook
2020 A guidebook intended for use by first responders A guidebook intended for use by first responders during the initial phase of a transportation incident during the initial phase of a transportation incident involving hazardous materials/dangerous goods involving hazardous materials/dangerous goods EMERGENCY RESPONSE GUIDEBOOK THIS DOCUMENT SHOULD NOT BE USED TO DETERMINE COMPLIANCE WITH THE HAZARDOUS MATERIALS/ DANGEROUS GOODS REGULATIONS OR 2020 TO CREATE WORKER SAFETY DOCUMENTS EMERGENCY RESPONSE FOR SPECIFIC CHEMICALS GUIDEBOOK NOT FOR SALE This document is intended for distribution free of charge to Public Safety Organizations by the US Department of Transportation and Transport Canada. This copy may not be resold by commercial distributors. https://www.phmsa.dot.gov/hazmat https://www.tc.gc.ca/TDG http://www.sct.gob.mx SHIPPING PAPERS (DOCUMENTS) 24-HOUR EMERGENCY RESPONSE TELEPHONE NUMBERS For the purpose of this guidebook, shipping documents and shipping papers are synonymous. CANADA Shipping papers provide vital information regarding the hazardous materials/dangerous goods to 1. CANUTEC initiate protective actions. A consolidated version of the information found on shipping papers may 1-888-CANUTEC (226-8832) or 613-996-6666 * be found as follows: *666 (STAR 666) cellular (in Canada only) • Road – kept in the cab of a motor vehicle • Rail – kept in possession of a crew member UNITED STATES • Aviation – kept in possession of the pilot or aircraft employees • Marine – kept in a holder on the bridge of a vessel 1. CHEMTREC 1-800-424-9300 Information provided: (in the U.S., Canada and the U.S. Virgin Islands) • 4-digit identification number, UN or NA (go to yellow pages) For calls originating elsewhere: 703-527-3887 * • Proper shipping name (go to blue pages) • Hazard class or division number of material 2. -

3.2.2 Table B: List of Dangerous Goods in Alphabetical Order the Following
Copyright © United Nations, 2008 3.2.2 Table B: List of dangerous goods in alphabetical order The following Table B is an alphabetical list of the substances and articles which are listed in the UN numerical order in Table A of 3.2.1. It does not form an integral part of ADN. It has been prepared, with all necessary care by the Secretariat of the United Nations Economic Commission for Europe, in order to facilitate the consultation of Annexes A and B, but it cannot be relied upon as a substitute for the careful study and observance of the actual provisions of those annexed Regulations which, in case of conflict, are deemed to be authoritative. NOTE 1: For the purpose of determining the alphabetical order the following information has been ignored, even when it forms part of the proper shipping name: numbers; Greek letters; the abbreviations "sec" and "tert"; and the letters "N" (nitrogen), "n" (normal), "o" (ortho) "m" (meta), "p" (para) and "N.O.S." (not otherwise specified). NOTE 2: The name of a substance or article in block capital letters indicates a proper shipping name (see 3.1.2). NOTE 3: The name of a substance or article in block capital letters followed by the word "see" indicates an alternative proper shipping name or part of a proper shipping name (except for PCBs) (see 3.1.2.1). NOTE 4: An entry in lower case letters followed by the word "see" indicates that the entry is not a proper shipping name; it is a synonym. NOTE 5: Where an entry is partly in block capital letters and partly in lower case letters, the latter part is considered not to be part of the proper shipping name (see 3.1.2.1). -

Chemical Weapons Technology Section 4—Chemical Weapons Technology
SECTION IV CHEMICAL WEAPONS TECHNOLOGY SECTION 4—CHEMICAL WEAPONS TECHNOLOGY Scope Highlights 4.1 Chemical Material Production ........................................................II-4-8 4.2 Dissemination, Dispersion, and Weapons Testing ..........................II-4-22 • Chemical weapons (CW) are relatively inexpensive to produce. 4.3 Detection, Warning, and Identification...........................................II-4-27 • CW can affect opposing forces without damaging infrastructure. 4.4 Chemical Defense Systems ............................................................II-4-34 • CW can be psychologically devastating. • Blister agents create casualties requiring attention and inhibiting BACKGROUND force efficiency. • Defensive measures can be taken to negate the effect of CW. Chemical weapons are defined as weapons using the toxic properties of chemi- • Donning of protective gear reduces combat efficiency of troops. cal substances rather than their explosive properties to produce physical or physiologi- • Key to employment is dissemination and dispersion of agents. cal effects on an enemy. Although instances of what might be styled as chemical weapons date to antiquity, much of the lore of chemical weapons as viewed today has • CW are highly susceptible to environmental effects (temperature, its origins in World War I. During that conflict “gas” (actually an aerosol or vapor) winds). was used effectively on numerous occasions by both sides to alter the outcome of • Offensive use of CW complicates command and control and battles. A significant number of battlefield casualties were sustained. The Geneva logistics problems. Protocol, prohibiting use of chemical weapons in warfare, was signed in 1925. Sev- eral nations, the United States included, signed with a reservation forswearing only the first use of the weapons and reserved the right to retaliate in kind if chemical weapons were used against them.