Epithelial Delamination Is Protective During Pharmaceutical-Induced Enteropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Global Analysis of Protein Folding Thermodynamics for Disease State Characterization
Global Analysis of Protein Folding Thermodynamics for Disease State Characterization and Biomarker Discovery by Jagat Adhikari Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Michael C. Fitzgerald, Supervisor ___________________________ Kenneth Kreuzer ___________________________ Terrence G. Oas ___________________________ Jiyong Hong ___________________________ Seok-Yong Lee Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Biochemistry in the Graduate School of Duke University 2015 ABSTRACT Global Analysis of Protein Folding Thermodynamics for Disease State Characterization and Biomarker Discovery by Jagat Adhikari Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Michael C. Fitzgerald, Supervisor ___________________________ Kenneth Kreuzer ___________________________ Terrence G. Oas ___________________________ Jiyong Hong ___________________________ Seok-Yong Lee An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Biochemistry in the Graduate School of Duke University 2015 Copyright by Jagat Adhikari 2015 Abstract Protein biomarkers can facilitate the diagnosis of many diseases such as cancer and they can be important for the development of effective therapeutic interventions. Current large-scale biomarker discovery and disease state characterization -
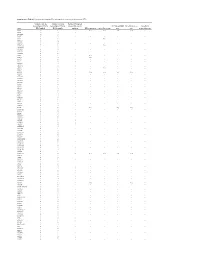
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Supplemental Materials Supplemental Table 1
Electronic Supplementary Material (ESI) for RSC Advances. This journal is © The Royal Society of Chemistry 2016 Supplemental Materials Supplemental Table 1. The differentially expressed proteins from rat pancreas identified by proteomics (SAP vs. SO) No. Protein name Gene name ratio P value 1 Metallothionein Mt1m 3.35 6.34E-07 2 Neutrophil antibiotic peptide NP-2 Defa 3.3 8.39E-07 3 Ilf2 protein Ilf2 3.18 1.75E-06 4 Numb isoform o/o rCG 3.12 2.73E-06 5 Lysozyme Lyz2 3.01 5.63E-06 6 Glucagon Gcg 2.89 1.17E-05 7 Serine protease HTRA1 Htra1 2.75 2.97E-05 8 Alpha 2 macroglobulin cardiac isoform (Fragment) 2.75 2.97E-05 9 Myosin IF (Predicted) Myo1f 2.65 5.53E-05 10 Neuroendocrine secretory protein 55 Gnas 2.61 7.60E-05 11 Matrix metallopeptidase 8 Mmp8 2.57 9.47E-05 12 Protein Tnks1bp1 Tnks1bp1 2.53 1.22E-04 13 Alpha-parvin Parva 2.47 1.78E-04 14 C4b-binding protein alpha chain C4bpa 2.42 2.53E-04 15 Protein KTI12 homolog Kti12 2.41 2.74E-04 16 Protein Rab11fip5 Rab11fip5 2.41 2.84E-04 17 Protein Mcpt1l3 Mcpt1l3 2.33 4.43E-04 18 Phospholipase B-like 1 Plbd1 2.33 4.76E-04 Aldehyde dehydrogenase (NAD), cytosolic 19 2.32 4.93E-04 (Fragments) 20 Protein Dpy19l2 Dpy19l2 2.3 5.68E-04 21 Regenerating islet-derived 3 alpha, isoform CRA_a Reg3a 2.27 6.74E-04 22 60S acidic ribosomal protein P1 Rplp1 2.26 7.22E-04 23 Serum albumin Alb 2.25 7.98E-04 24 Ribonuclease 4 Rnase4 2.24 8.25E-04 25 Cct-5 protein (Fragment) Cct5 2.24 8.52E-04 26 Protein S100-A9 S100a9 2.22 9.71E-04 27 Creatine kinase M-type Ckm 2.21 1.00E-03 28 Protein Larp4b Larp4b 2.18 1.25E-03 -
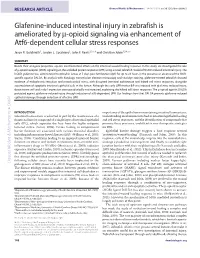
Glafenine-Induced Intestinal Injury in Zebrafish Is Ameliorated by -Opioid Signaling Via Enhancement of Atf6-Dependent Cellular Stress Responses
RESEARCH ARTICLE Disease Models & Mechanisms 6, 146-159 (2013) doi:10.1242/dmm.009852 Glafenine-induced intestinal injury in zebrafish is ameliorated by -opioid signaling via enhancement of Atf6-dependent cellular stress responses Jason R. Goldsmith1, Jordan L. Cocchiaro2, John F. Rawls2,3,*,‡ and Christian Jobin1,3,4,*,‡ SUMMARY Beside their analgesic properties, opiates exert beneficial effects on the intestinal wound healing response. In this study, we investigated the role of -opioid receptor (MOR) signaling on the unfolded protein response (UPR) using a novel zebrafish model of NSAID-induced intestinal injury. The NSAID glafenine was administered to zebrafish larvae at 5 days post-fertilization (dpf) for up to 24 hours in the presence or absence of the MOR- specific agonist DALDA. By analysis with histology, transmission electron microscopy and vital dye staining, glafenine-treated zebrafish showed evidence of endoplasmic reticulum and mitochondrial stress, with disrupted intestinal architecture and halted cell stress responses, alongside accumulation of apoptotic intestinal epithelial cells in the lumen. Although the early UPR marker BiP was induced with glafenine-induced injury, downstream atf6 and s-xbp1 expression were paradoxically not increased, explaining the halted cell stress responses. The -opioid agonist DALDA protected against glafenine-induced injury through induction of atf6-dependent UPR. Our findings show that DALDA prevents glafenine-induced epithelial damage through induction of effective UPR. DMM INTRODUCTION importance of the epithelium in maintaining intestinal homeostasis, Intestinal homeostasis is achieved in part by the maintenance of a understanding mechanisms involved in intestinal epithelial healing functional barrier composed of a single layer of intestinal epithelial and cell stress responses, and the identification of compounds that cells (IEC), which separates the host from the highly antigenic promote these processes, could lead to new therapeutic strategies lumenal milieu (Sartor, 2008). -

MALE Protein Name Accession Number Molecular Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean H Mean PDAC Mean T-Test PDAC Vs. H T-Test
MALE t-test t-test Accession Molecular H PDAC PDAC vs. PDAC vs. Protein Name Number Weight CP1 CP2 H1 H2 PDAC1 PDAC2 CP Mean Mean Mean H CP PDAC/H PDAC/CP - 22 kDa protein IPI00219910 22 kDa 7 5 4 8 1 0 6 6 1 0.1126 0.0456 0.1 0.1 - Cold agglutinin FS-1 L-chain (Fragment) IPI00827773 12 kDa 32 39 34 26 53 57 36 30 55 0.0309 0.0388 1.8 1.5 - HRV Fab 027-VL (Fragment) IPI00827643 12 kDa 4 6 0 0 0 0 5 0 0 - 0.0574 - 0.0 - REV25-2 (Fragment) IPI00816794 15 kDa 8 12 5 7 8 9 10 6 8 0.2225 0.3844 1.3 0.8 A1BG Alpha-1B-glycoprotein precursor IPI00022895 54 kDa 115 109 106 112 111 100 112 109 105 0.6497 0.4138 1.0 0.9 A2M Alpha-2-macroglobulin precursor IPI00478003 163 kDa 62 63 86 72 14 18 63 79 16 0.0120 0.0019 0.2 0.3 ABCB1 Multidrug resistance protein 1 IPI00027481 141 kDa 41 46 23 26 52 64 43 25 58 0.0355 0.1660 2.4 1.3 ABHD14B Isoform 1 of Abhydrolase domain-containing proteinIPI00063827 14B 22 kDa 19 15 19 17 15 9 17 18 12 0.2502 0.3306 0.7 0.7 ABP1 Isoform 1 of Amiloride-sensitive amine oxidase [copper-containing]IPI00020982 precursor85 kDa 1 5 8 8 0 0 3 8 0 0.0001 0.2445 0.0 0.0 ACAN aggrecan isoform 2 precursor IPI00027377 250 kDa 38 30 17 28 34 24 34 22 29 0.4877 0.5109 1.3 0.8 ACE Isoform Somatic-1 of Angiotensin-converting enzyme, somaticIPI00437751 isoform precursor150 kDa 48 34 67 56 28 38 41 61 33 0.0600 0.4301 0.5 0.8 ACE2 Isoform 1 of Angiotensin-converting enzyme 2 precursorIPI00465187 92 kDa 11 16 20 30 4 5 13 25 5 0.0557 0.0847 0.2 0.4 ACO1 Cytoplasmic aconitate hydratase IPI00008485 98 kDa 2 2 0 0 0 0 2 0 0 - 0.0081 - 0.0 -

Product Monograph
PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets NSAID Analgesic Agent Novopharm Limited Date of Revision: Toronto, Canada August 02, 2007 Control Number 112565 PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets THERAPEUTIC CLASSIFICATION NSAID Analgesic Agent ACTION AND CLINICAL PHARMACOLOGY NOVO-KETOROLAC (ketorolac tromethamine) is a non-steroidal anti-inflammatory drug (NSAID) that has analgesic activity. It is considered to be a peripherally acting analgesic. It is thought to inhibit the cyclo-oxygenase enzyme system, thereby inhibiting the synthesis of prostaglandins. At analgesic doses it has minimal anti-inflammatory and antipyretic activity. The peak analgesic effect occurs at 2 to 3 hours post-dosing with no evidence of a statistically significant difference over the recommended dosage range. The greatest difference between large and small doses of administered ketorolac is in the duration of analgesia. Following oral administration, ketorolac tromethamine is rapidly and completely absorbed, and pharmacokinetics are linear following single and multiple dosing. Steady state plasma levels are achieved after one day of q.i.d. dosing. - 2 - Peak plasma concentrations of 0.7 to 1.1 µg/mL occurred at 44 minutes following a single oral dose of 10 mg. The terminal plasma elimination half-life ranged between 2.4 and 9 hours in healthy adults, while in the elderly subjects (mean age: 72 years) it ranged between 4.3 and 7.6 hours. A high fat meal decreased the rate but not the extent of absorption of oral ketorolac tromethamine, while antacid had no effect. In renally impaired patients there is a reduction in clearance and an increase in the terminal half- life of ketorolac tromethamine (See Table 1). -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine. -

Journal of Environment and Health Sciences
Journal of Environment and Health Sciences Review Article Organophosphorus Flame Retardants (OPFR): Neurotoxicity Mohamed B. Abou-Donia1* Mohamed Salama2, Mohamed Elgamal2, Islam Elkholi2,3, Qiangwei Wang1,4 1Department of Pharmacology and Cancer Biology, Duke University Medical Center, Durham, North Carolina, USA 2Medical Experimental Research Center (MERC), Faculty of Medicine, Mansoura University, Mansoura, Egypt 3Center for Aging and Associated Diseases (CAAD), Zewail City of Science and Technology, Giza 4Zhejiang University, China *Corresponding author: Mohamed B. Abou-Donia, Department of Pharmacology and Cancer Biology, Duke University Medical Center, Durham, North Carolina 277, USA, Tel: +919-68422/ Fax: 919-681-822, E-mail: [email protected] Citation: Abou-Donia, M.B., et al. Organophosphorus Flame Retardants (OPFR): Neurotoxicity. (2016) J Environ Health Sci 2(1): 1- 30 Received date: July 07, 2015 Accepted date: May 05, 2016 DOI: 10.15436/2378-6841.16.022 Published date: May 11, 2016 Abstract Organophosphorus flame retardants (OPFRs) are used as additives in plasticizers, foams, hydraulic fluids, anti-foam agents, and coatings for electronic components/devices to inhibit flames. These chemicals were developed and used as flame re- tardants because of environmental and health concerns of previously used brominated and chlorinated flame retardants (FRs). OPCFRs are divided into five main groups: organophosphates, organophosphonates, organophosphinates, organoposphine oxide, and organophosphites. Most of OPFRs are organophosphate esters that are further classified into the following five groups: 1. Ali- phatic, 2. Brominated aliphatic, 3. Chlorinated aliphatic, 4. Aromatic-aliphatic, and 5. Aromatic phosphates. These OPFRs have the following neurotoxic actions: 1. Cholinergic Neurotoxicity, 2. Organophosphate-Induced Delayed Neurotoxicity (OPIDN), and 3. -

Assessing the Role of APNH, a Gene Encoding for a Human Amiloride
Assessing the Role of APNH, a Gene Encoding for a Human Amiloride-Sensitive Na/H Antiporter, on the Interindividual Variation in Red Cell Na/Li Count ert ransport1 Christopher R.K. Dudley,2 Luis A. Giuffra, Anthony E.G. Rome, and Stephen T. Reeders correction of SIC values for known covariotes. There C.R.K. Dudley, S.T. Reeders, Department of Internal was no significant association between mean SIC Medicine. Yale University School of Medicine, New- values and any of the three possible genotypes of Haven, CT the APNH locus either before or after regressing out L.A. Giuffra, ST. Reeders, Department of Human Ge- covariates (F= 0.64 and P> 0.52; F= 0.63 and P> netics, Yale University School of Medicine, New- 0.53, respectively). Linkage analysis similarly foiled Haven, CT to demonstrate a relationship between the squared A.E.G. Rome, Department of Nephrology, The Royal difference In SIC values and the identity by descent Hospital of St. Bartholomew, London, England status for APNH as well as other loci that map close to APNH (D1S57, RH, and ALPI). Taking these results (J. Am. Soc. Nephrol. 1991; 2:937-943) together, we conclude that mutations at the APNH locus are not responsible for the observed variation in SIC values. ABSTRACT Key Words: Blood pressure, intermediate phenotype, associ- The “reverse genetic” approach to essential hyper- ation study, sib pair method, linkage analysis tension Is complicated by the tact that blood pres- sure is a heterogeneous, quantitative, complex trait. One strategy is to use Intermediate phenotypes” that are not only associated with hypertension but S ince the original observation by Canessa et at. -

Licofelone Enhances the Efficacy of Paclitaxel in Ovarian Cancer by Reversing Drug
Author Manuscript Published OnlineFirst on June 11, 2018; DOI: 10.1158/0008-5472.CAN-17-3993 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Licofelone enhances the efficacy of paclitaxel in ovarian cancer by reversing drug resistance and tumor stem-like properties Jeff Hirst1, Harsh B. Pathak1, Stephen Hyter1, Ziyan Y. Pessetto1, Thuc Ly1, Stefan Graw2, Devin C. Koestler2,3, Adam J. Krieg4,5, Katherine F. Roby3,6,7, and Andrew K. Godwin1,3 1Department of Pathology and Laboratory Medicine, University of Kansas Medical Center, Kansas City, KS, USA 2Department of Biostatistics, University of Kansas Medical Center, Kansas City, KS, USA 3University of Kansas Cancer Center, University of Kansas Medical Center, Kansas City, KS, USA 4Department of Obstetrics and Gynecology, Oregon Health & Science University, Portland, OR, USA 5Division of Reproductive and Developmental Sciences, Oregon National Primate Research Center, Beaverton, OR, USA 6Institute for Reproductive Health and Regenerative Medicine, University of Kansas Medical Center, Kansas City, KS, USA 7Department of Anatomy & Cell Biology, University of Kansas Medical Center, Kansas City, KS, USA Corresponding author: Andrew K. Godwin 3901 Rainbow Boulevard, MS 3040 Kansas City, KS 66160 Email: [email protected] Phone: 913-945-6373 Fax (913) 945-6327 DISCLOSURE OF POTENTIAL CONFLICT OF INTEREST -1- Downloaded from cancerres.aacrjournals.org on September 26, 2021. © 2018 American Association for Cancer Research. Author Manuscript Published OnlineFirst on June 11, 2018; DOI: 10.1158/0008-5472.CAN-17-3993 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. The authors declare no potential conflicts of interest. -

Does Paracetamol (Acetaminophen) Reduce the Pain of Osteoarthritis?: a Meta-Analysis of Randomised Controlled Trials W Zhang, a Jones, M Doherty
901 REVIEW Ann Rheum Dis: first published as 10.1136/ard.2003.018531 on 5 March 2004. Downloaded from Does paracetamol (acetaminophen) reduce the pain of osteoarthritis?: a meta-analysis of randomised controlled trials W Zhang, A Jones, M Doherty ............................................................................................................................... Ann Rheum Dis 2004;63:901–907. doi: 10.1136/ard.2003.018531 Objective: To assess the best available evidence for efficacy of paracetamol (acetaminophen) in the treatment of osteoarthritis (OA). Design: Systematic review and meta-analysis of randomised controlled trials (RCTs). Data sources: Medline, Embase, Scientific Citation Index, CINAHL, Cochrane Library, and conference abstracts in the past 2 years from the British Society for Rheumatology, the European League Against Rheumatism, the American College of Rheumatology, and the Osteoarthritis Research Society International. Subjects: 10 RCTs including 1712 patients with either symptomatic OA of the knee (6 trials) or hip/knee (3 trials) or multiple joints (1 trial). See end of article for authors’ affiliations Main outcome measures: (a) effect size (ES) for pain, stiffness, and functional scores from baseline to end ....................... point; (b) rate ratio (RR) and number needed to treat for clinical response rate and patient preference for treatment. Correspondence to: Dr W Zhang, Academic Results: Paracetamol was effective in relieving pain due to OA (ES = 0.21, 95% confidence interval (CI) Rheumatology, University 0.02 to 0.41). Non-steroidal anti-inflammatory drugs (NSAIDs) were better than paracetamol for pain of Nottingham, Clinical relief (ES = 0.20, 95% CI 0.10 to 0.30). Clinical response rate was higher with NSAIDs than with Sciences Building, City Hospital, Nottingham NG5 paracetamol (RR = 1.24, 95% CI 1.08 to 1.41), and the number of patients who preferred NSAIDs was 1PB, UK; weiya.zhang@ more than twice the number of those preferring paracetamol (RR = 2.46, 95% CI 1.51 to 4.12).