Tissue-Nonspecific Alkaline Phosphatase
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Coronal and Lambdoid Suture Evolution Following Total Vault Remodeling for Scaphocephaly
NEUROSURGICAL FOCUS Neurosurg Focus 50 (4):E4, 2021 Coronal and lambdoid suture evolution following total vault remodeling for scaphocephaly Pierre-Aurélien Beuriat, MD, PhD,1,2,4 Alexandru Szathmari, MD, PhD,1,2 Julie Chauvel-Picard, MD,1,3,4 Arnaud Gleizal, MD, PhD,1,3,4 Christian Paulus, MD,1,3 Carmine Mottolese, MD, PhD,1,2 and Federico Di Rocco, MD, PhD1,2,4 1French Referral Center for Craniosynostosis; Departments of 2Pediatric Neurosurgery and 3Pediatric Maxillo-Facial Surgery, Hôpital Femme Mère Enfant; and 4Université de Lyon, France OBJECTIVE Different types of surgical procedures are utilized to treat craniosynostosis. In most procedures, the fused suture is removed. There are only a few reports on the evolution of sutures after surgical correction of craniosynostosis. To date, no published study describes neosuture formation after total cranial vault remodeling. The objective of this study was to understand the evolution of the cranial bones in the area of coronal and lambdoid sutures that were removed for complete vault remodeling in patients with sagittal craniosynostosis. In particular, the investigation aimed to confirm the possibility of neosuture formation. METHODS CT images of the skulls of children who underwent operations for scaphocephaly at the Hôpital Femme Mère Enfant, Lyon University Hospital, Lyon, France, from 2004 to 2014 were retrospectively reviewed. Inclusion crite- ria were diagnosis of isolated sagittal synostosis, age between 4 and 18 months at surgery, and availability of reliable postoperative CT images obtained at a minimum of 1 year after surgical correction. Twenty-six boys and 11 girls were included, with a mean age at surgery of 231.6 days (range 126–449 days). -

Epigenome-Wide Association Study of Wellbeing
Twin Research and Human Genetics Volume 18 Number 6 pp. 710–719 C The Author(s) 2015 doi:10.1017/thg.2015.85 Epigenome-Wide Association Study of Wellbeing Bart M. L. Baselmans,1,2 Jenny van Dongen,1,2 Michel G. Nivard,1 Bochao D. Lin,1 BIOS Consortium,3 Nuno R. Zilhao,˜ 1 Dorret I. Boomsma,1,2,4 and Meike Bartels1,2,4 1Department of Biological Psychology, VU University, Amsterdam, the Netherlands 2EMGO+ Institute for Health and Care Research, VU University Medical Center, Amsterdam, the Netherlands 3The Biobank-Based Integrative Omics Study (BIOS) Consortium 4Neuroscience Campus Amsterdam, Amsterdam, the Netherlands Wellbeing (WB) is a major topic of research across several scientific disciplines, partly driven by its strong association with psychological and mental health. Twin-family studies have found that both genotype and environment play an important role in explaining the variance in WB. Epigenetic mechanisms, such as DNA methylation, regulate gene expression, and may mediate genetic and environmental effects on WB. Here, for the first time, we apply an epigenome-wide association study (EWAS) approach to identify differentially methylated sites associated with individual differences in WB. Subjects were part of the longitudinal survey studies of the Netherlands Twin Register (NTR) and participated in the NTR biobank project between 2002 and 2011. WB was assessed by a short inventory that measures satisfaction with life (SAT). DNA methylation was measured in whole blood by the Illumina Infinium HumanMethylation450 BeadChip (HM450k array) and the association between WB and DNA methylation level was tested at 411,169 autosomal sites. Two sites (cg10845147, p = 1.51 ∗ 10-8 and cg01940273, p = 2.34 ∗ 10-8) reached genome-wide significance following Bonferonni correction. -

Structural Characterization of Polysaccharides from Cordyceps Militaris and Their Hypolipidemic Effects Cite This: RSC Adv.,2018,8,41012 in High Fat Diet Fed Mice†
RSC Advances View Article Online PAPER View Journal | View Issue Structural characterization of polysaccharides from Cordyceps militaris and their hypolipidemic effects Cite this: RSC Adv.,2018,8,41012 in high fat diet fed mice† Zhen-feng Huang, ‡ Ming-long Zhang,‡ Song Zhang,* Ya-hui Wang and Xue-wen Jiang Cordyceps militaris is a crude dietary therapeutic mushroom with high nutritional and medicinal values. Mushroom-derived polysaccharides have been found to possess antihyperglycemic and antihyperlipidemic activities. This study aimed to partially clarify the structural characterization and comparatively evaluate hypolipidemic potentials of intracellular- (IPCM) and extracellular polysaccharides of C. militaris (EPCM) in high fat diet fed mice. Results indicated that IPCM-2 is a-pyran polysaccharide with an average molecular weight of 32.5 kDa, was mainly composed of mannose, glucose and galactose with mass percentages of 51.94%, 10.54%, and 37.25%, respectively. EPCM-2 is an a-pyran Creative Commons Attribution 3.0 Unported Licence. polysaccharide with an average molecular weight of 20 kDa that is mainly composed of mannose, glucose and galactose with mass percentages of 44.51%, 18.33%, and 35.38%, respectively. In in vivo study, EPCM-1 treatment (100 mg kgÀ1 dÀ1) showed potential effects on improving serum lipid profiles of hyperlipidemic mice, reflected by decreasing serum total cholesterol (TC), triglyceride (TG) and low density lipoprotein-cholesterol (LDL-C) levels by 20.05%, 45.45% and 52.63%, respectively, while IPCM-1 treatment -

Epithelial Delamination Is Protective During Pharmaceutical-Induced Enteropathy
Epithelial delamination is protective during pharmaceutical-induced enteropathy Scott T. Espenschieda, Mark R. Cronana, Molly A. Mattya, Olaf Muellera, Matthew R. Redinbob,c,d, David M. Tobina,e,f, and John F. Rawlsa,e,1 aDepartment of Molecular Genetics and Microbiology, Duke University School of Medicine, Durham, NC 27710; bDepartment of Chemistry, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; cDepartment of Biochemistry, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; dDepartment of Microbiology and Immunology, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; eDepartment of Medicine, Duke University School of Medicine, Durham, NC 27710; and fDepartment of Immunology, Duke University School of Medicine, Durham, NC 27710 Edited by Dennis L. Kasper, Harvard Medical School, Boston, MA, and approved July 15, 2019 (received for review February 12, 2019) Intestinal epithelial cell (IEC) shedding is a fundamental response to in mediating intestinal responses to injury remains poorly un- intestinal damage, yet underlying mechanisms and functions have derstood for most xenobiotics. been difficult to define. Here we model chronic intestinal damage in Gastrointestinal pathology is common in people using phar- zebrafish larvae using the nonsteroidal antiinflammatory drug maceuticals, including nonsteroidal antiinflammatory drugs (NSAID) Glafenine. Glafenine induced the unfolded protein response (NSAIDs) (11). While gastric ulceration has historically been a (UPR) and inflammatory pathways in IECs, leading to delamination. defining clinical presentation of NSAID-induced enteropathy, Glafenine-induced inflammation was augmented by microbial colo- small intestinal pathology has also been observed, although the nizationandassociatedwithchanges in intestinal and environmental incidence may be underreported due to diagnostic limitations microbiotas. -

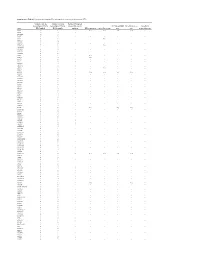
Table S1 the Four Gene Sets Derived from Gene Expression Profiles of Escs and Differentiated Cells
Table S1 The four gene sets derived from gene expression profiles of ESCs and differentiated cells Uniform High Uniform Low ES Up ES Down EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol EntrezID GeneSymbol 269261 Rpl12 11354 Abpa 68239 Krt42 15132 Hbb-bh1 67891 Rpl4 11537 Cfd 26380 Esrrb 15126 Hba-x 55949 Eef1b2 11698 Ambn 73703 Dppa2 15111 Hand2 18148 Npm1 11730 Ang3 67374 Jam2 65255 Asb4 67427 Rps20 11731 Ang2 22702 Zfp42 17292 Mesp1 15481 Hspa8 11807 Apoa2 58865 Tdh 19737 Rgs5 100041686 LOC100041686 11814 Apoc3 26388 Ifi202b 225518 Prdm6 11983 Atpif1 11945 Atp4b 11614 Nr0b1 20378 Frzb 19241 Tmsb4x 12007 Azgp1 76815 Calcoco2 12767 Cxcr4 20116 Rps8 12044 Bcl2a1a 219132 D14Ertd668e 103889 Hoxb2 20103 Rps5 12047 Bcl2a1d 381411 Gm1967 17701 Msx1 14694 Gnb2l1 12049 Bcl2l10 20899 Stra8 23796 Aplnr 19941 Rpl26 12096 Bglap1 78625 1700061G19Rik 12627 Cfc1 12070 Ngfrap1 12097 Bglap2 21816 Tgm1 12622 Cer1 19989 Rpl7 12267 C3ar1 67405 Nts 21385 Tbx2 19896 Rpl10a 12279 C9 435337 EG435337 56720 Tdo2 20044 Rps14 12391 Cav3 545913 Zscan4d 16869 Lhx1 19175 Psmb6 12409 Cbr2 244448 Triml1 22253 Unc5c 22627 Ywhae 12477 Ctla4 69134 2200001I15Rik 14174 Fgf3 19951 Rpl32 12523 Cd84 66065 Hsd17b14 16542 Kdr 66152 1110020P15Rik 12524 Cd86 81879 Tcfcp2l1 15122 Hba-a1 66489 Rpl35 12640 Cga 17907 Mylpf 15414 Hoxb6 15519 Hsp90aa1 12642 Ch25h 26424 Nr5a2 210530 Leprel1 66483 Rpl36al 12655 Chi3l3 83560 Tex14 12338 Capn6 27370 Rps26 12796 Camp 17450 Morc1 20671 Sox17 66576 Uqcrh 12869 Cox8b 79455 Pdcl2 20613 Snai1 22154 Tubb5 12959 Cryba4 231821 Centa1 17897 -

Global Analysis of Protein Folding Thermodynamics for Disease State Characterization
Global Analysis of Protein Folding Thermodynamics for Disease State Characterization and Biomarker Discovery by Jagat Adhikari Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Michael C. Fitzgerald, Supervisor ___________________________ Kenneth Kreuzer ___________________________ Terrence G. Oas ___________________________ Jiyong Hong ___________________________ Seok-Yong Lee Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Biochemistry in the Graduate School of Duke University 2015 ABSTRACT Global Analysis of Protein Folding Thermodynamics for Disease State Characterization and Biomarker Discovery by Jagat Adhikari Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Michael C. Fitzgerald, Supervisor ___________________________ Kenneth Kreuzer ___________________________ Terrence G. Oas ___________________________ Jiyong Hong ___________________________ Seok-Yong Lee An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Biochemistry in the Graduate School of Duke University 2015 Copyright by Jagat Adhikari 2015 Abstract Protein biomarkers can facilitate the diagnosis of many diseases such as cancer and they can be important for the development of effective therapeutic interventions. Current large-scale biomarker discovery and disease state characterization -

Frontosphenoidal Synostosis: a Rare Cause of Unilateral Anterior Plagiocephaly
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Childs Nerv Syst (2007) 23:1431–1438 DOI 10.1007/s00381-007-0469-4 ORIGINAL PAPER Frontosphenoidal synostosis: a rare cause of unilateral anterior plagiocephaly Sandrine de Ribaupierre & Alain Czorny & Brigitte Pittet & Bertrand Jacques & Benedict Rilliet Received: 30 March 2007 /Published online: 22 September 2007 # Springer-Verlag 2007 Abstract Conclusion Frontosphenoidal synostosis must be searched Introduction When a child walks in the clinic with a in the absence of a coronal synostosis in a child with unilateral frontal flattening, it is usually associated in our anterior unilateral plagiocephaly, and treated surgically. minds with unilateral coronal synostosis. While the latter might be the most common cause of anterior plagiocephaly, Keywords Craniosynostosis . Pediatric neurosurgery. it is not the only one. A patent coronal suture will force us Anterior plagiocephaly to consider other etiologies, such as deformational plagio- cephaly, or synostosis of another suture. To understand the mechanisms underlying this malformation, the development Introduction and growth of the skull base must be considered. Materials and methods There have been few reports in the Harmonious cranial growth is dependent on patent sutures, literature of isolated frontosphenoidal suture fusion, and and any craniosynostosis might lead to an asymmetrical we would like to report a series of five cases, as the shape of the skull. The anterior skull base is formed of recognition of this entity is important for its treatment. different bones, connected by sutures, fusing at different ages. The frontosphenoidal suture extends from the end of Presented at the Consensus Conference on Pediatric Neurosurgery, the frontoparietal suture, anteriorly and inferiorly in the Rome, 1–2 December 2006. -

TNAP As a New Player in Chronic Inflammatory Conditions And
International Journal of Molecular Sciences Review TNAP as a New Player in Chronic Inflammatory Conditions and Metabolism Stephanie Graser 1,*, Daniel Liedtke 2,† and Franz Jakob 1,† 1 Bernhard-Heine-Center for Locomotion Research, Department of Orthopedics, Julius-Maximilians-University Würzburg, 97076 Würzburg, Germany; [email protected] 2 Institute for Human Genetics, Biocenter, Julius-Maximilians-University Würzburg, 97074 Würzburg, Germany; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: This review summarizes important information on the ectoenzyme tissue-nonspecific alkaline phosphatase (TNAP) and gives a brief insight into the symptoms, diagnostics, and treatment of the rare disease Hypophosphatasia (HPP), which is resulting from mutations in the TNAP encoding ALPL gene. We emphasize the role of TNAP beyond its well-known contribution to mineralization processes. Therefore, above all, the impact of the enzyme on central molecular processes in the nervous system and on inflammation is presented here. Keywords: TNAP; Hypophosphatasia; HPP; mineralization; nervous system; inflammation 1. Structure, Function, and Substrates of TNAP Tissue-nonspecific alkaline phosphatase (TNAP) or liver/bone/kidney alkaline phos- phatase is an ectoenzyme that is anchored to the outer cell membrane (e.g. in osteoblasts) Citation: Graser, S.; Liedtke, D.; and to extracellular vesicles via its glycosyl-inositol-phosphate (GPI)-anchor [1,2]. TNAP Jakob, F. TNAP as a New Player in belongs to the family of alkaline phosphatases (AP) that comprises in humans three addi- Chronic Inflammatory Conditions tional tissue-specific isoforms: placental (PLAP, ALPP National Center for Biotechnology and Metabolism. Int. -

(PDE 1 B 1) Correlates with Brain Regions Having Extensive Dopaminergic Innervation
The Journal of Neuroscience, March 1994, 14(3): 1251-l 261 Expression of a Calmodulin-dependent Phosphodiesterase lsoform (PDE 1 B 1) Correlates with Brain Regions Having Extensive Dopaminergic Innervation Joseph W. Polli and Randall L. Kincaid Section on Immunology, Laboratory of Molecular and Cellular Neurobiology, National Institute on Alcohol Abuse and Alcoholism, Rockville, Maryland 20852 Cyclic nucleotide-dependent protein phosphorylation plays PDE implies an important physiological role for Ca2+-regu- a central role in neuronal signal transduction. Neurotrans- lated attenuation of CAMP-dependent signaling pathways mitter-elicited increases in cAMP/cGMP brought about by following dopaminergic stimulation. activation of adenylyl and guanylyl cyclases are downre- [Key words: CAMP, cyclase, striatum, dopamine, basal gulated by multiple phosphodiesterase (PDE) enzymes. In ganglia, DARPP-321 brain, the calmodulin (CaM)-dependent isozymes are the major degradative activities and represent a unique point of Cyclic nucleotides, acting as “second messengers”or via direct intersection between the cyclic nucleotide- and calcium effects, regulate a diverse array of neuronal functions, from ion (Ca*+)-mediated second messenger systems. Here we de- channel conductance to gene expression. Hydrolysis of 3’,5’- scribe the distribution of the PDEl Bl (63 kDa) CaM-depen- cyclic nucleotidesto 5’-nucleosidemonophosphates is the major dent PDE in mouse brain. An anti-peptide antiserum to this mechanismfor decreasingintracellular cyclic nucleotide levels. isoform immunoprecipitated -3O-40% of cytosolic PDE ac- This reaction is catalyzed by cyclic nucleotide phosphodiester- tivity, whereas antiserum to PDElA2 (61 kDa isoform) re- ase (PDE) enzymes that constitute a large superfamily (Beavo moved 60-70%, demonstrating that these isoforms are the and Reifsynder, 1990). -

Cleidocranial Dysplasia- a Case Report
Case Report Cleidocranial Dysplasia- A Case Report Akhilanand Chaurasia Department of Oral Medicine & Radiology, Faculty of Dental Sciences, King George Medical University, Lucknow E-mail: [email protected] ABSTRACT Cleidocranial dysplasia is a rare congenital disease. It is characterized by autosomal dominant inheritance pattern which is caused due to mutations in the Cbfa1 gene (Runx2) located on chromosome 6p21. It primarily affects bones which are formedby intra-membranous ossification and have equal sex distribution. It is also known as Marie and Sainton disease, Mutational dysostosis and cleidocranialdysostosis. The skeletal deformities of cleidocranial dysplasia are characterized by partial or complete absence of clavicles, late closure of the fontanels, presence of open skull sutures and multiple wormian bones. This rare syndrome is of utmost importance in dentistry due to presence of multiple supernumerary teeth, facial bones deformities and deranged eruption patterns. We are reporting a classical case of cleidocranial dysplasia in 20 year old patient. Keywords: Cleidocranial dysplasia, Marie and Sainton disease, Mutational dysostosis, Cleidocranialdysostosis, Autosomal dominant Access this article online mandibular symphysis are less common findings of Quick Response cleidocranial dysostosis1,10,11. Code: Website: Dental findings in cleidocranialdysostosis are www.innovativepublication.com characterized by a decreased eruptive force of both primary and permanent dentition, prolonged retention of primary teeth12 and an increase in odontogenesis DOI: 10.5958/2395-6194.2015.00009.0 leading to an excessive number of supernumerary teeth13. The clinical findings of cleidocranialdysostosis although present at birth are often either missed or INTRODUCTION diagnosed at a much later time. Cleidocranialdysostosis Cleidocranialdysostosis is a rare congenital defect may be identified by family history, excessive mobility primarily affecting bones which undergo intra- of shoulders and radiographic pathognomonic findings membranous ossification i.e. -
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Reduction of Pectinesterase Activity in a Commercial Enzyme Preparation
Journal of the Science of Food and Agriculture J Sci Food Agric 85:1613–1621 (2005) DOI: 10.1002/jsfa.2154 Reduction of pectinesterase activity in a commercial enzyme preparation by pulsed electric fields: comparison of inactivation kinetic models Joaquın´ Giner, Pascal Grouberman, Vicente Gimeno and Olga Martın´ ∗ Department of Food Technology, University of Lleida, CeRTA-UTPV, ETSEA, Avda Alcalde Rovira Roure 191, 25198-Lleida, Spain Abstract: The inactivation of pectinesterase (PE) in a commercial enzyme preparation (CEP) under high intensity pulsed electric fields (HIPEF) was studied. After desalting and water dilution of the raw CEP, samples were exposed to exponentially decay waveform pulses for up to 463 µs at electric field intensities ranging from 19 to 38 kV cm−1. Pulses were applied in monopolar mode. Experimental data were fitted to a first-order kinetic model as well as to models based on Fermi, Hulsheger¨ or Weibull equations to describe PE inactivation kinetics. Characteristic parameters for each model were calculated. Relationships between some of the parameters and process variables were obtained. The Weibull model yielded the best accuracy factor. The relationship between residual PE and input of electrical energy density was found to be that of exponential decay. 2005 Society of Chemical Industry Keywords: pulsed electric fields; kinetics; pectinesterase; model; inactivation INTRODUCTION It has become customary to use CEPs in fruit and Pectinesterase (PE; EC 3.1.1.11) is a pectic enzyme vegetable juice technology. Depending