Pharmaceutical Co-Crystal Compositions of Celecoxib
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pain Management in Companion Animals
CONTINUING EDUCATION TAP OUR APP Pain Management in Companion Animals Download “NCPA Mobile” Today! by Ann Philbrick, PharmD, BCPS Don’t be left out of the latest news affecting community pharmacy—download our new app, NCPA Mobile! Receive real-time updates, join the conversation on Twitter with a built-in feed, Jul. 1, 2015 (expires Jul. 1, 2018) and never miss out on breaking news affecting community pharmacy. Keep the Activity Type: Application-based app on your phone year-round for updates, news, alerts, and more from NCPA. To earn continuing education credit: ACPE Program 0207-0000-15-007-H01-P; 0207-0000-15-007-H01-T Upon successful completion of this article, the pharmacist should be able to: 1. Describe the process of pain in the dog and cat including identification of ways they express pain. 2. Describe the appropriate use, mechanism of action, and precautions for use of analgesics in the treatment of pain in dogs and cats. 3. Explain the key issues that impair the prevention of diversion in compan- ion animal owners. Upon successful completion of this article, the pharmacist should be able to: 1. Describe the process of pain in the dog and cat including identification of ways they express pain. To get the free NCPA Mobile app: 2. Describe the appropriate use, mechanism of action, and precautions for FREE ONLINE CE. To take advantage use of analgesics in the treatment of pain in dogs and cats. of free continuing pharmacy educa- iPhone and iPad users—search “NCPA 3. Explain the key issues that impair the prevention of diversion in compan- tion (CPE) for this program, pharma- ion animal owners. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Epithelial Delamination Is Protective During Pharmaceutical-Induced Enteropathy
Epithelial delamination is protective during pharmaceutical-induced enteropathy Scott T. Espenschieda, Mark R. Cronana, Molly A. Mattya, Olaf Muellera, Matthew R. Redinbob,c,d, David M. Tobina,e,f, and John F. Rawlsa,e,1 aDepartment of Molecular Genetics and Microbiology, Duke University School of Medicine, Durham, NC 27710; bDepartment of Chemistry, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; cDepartment of Biochemistry, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; dDepartment of Microbiology and Immunology, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; eDepartment of Medicine, Duke University School of Medicine, Durham, NC 27710; and fDepartment of Immunology, Duke University School of Medicine, Durham, NC 27710 Edited by Dennis L. Kasper, Harvard Medical School, Boston, MA, and approved July 15, 2019 (received for review February 12, 2019) Intestinal epithelial cell (IEC) shedding is a fundamental response to in mediating intestinal responses to injury remains poorly un- intestinal damage, yet underlying mechanisms and functions have derstood for most xenobiotics. been difficult to define. Here we model chronic intestinal damage in Gastrointestinal pathology is common in people using phar- zebrafish larvae using the nonsteroidal antiinflammatory drug maceuticals, including nonsteroidal antiinflammatory drugs (NSAID) Glafenine. Glafenine induced the unfolded protein response (NSAIDs) (11). While gastric ulceration has historically been a (UPR) and inflammatory pathways in IECs, leading to delamination. defining clinical presentation of NSAID-induced enteropathy, Glafenine-induced inflammation was augmented by microbial colo- small intestinal pathology has also been observed, although the nizationandassociatedwithchanges in intestinal and environmental incidence may be underreported due to diagnostic limitations microbiotas. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -
Glafenine-Induced Intestinal Injury in Zebrafish Is Ameliorated by -Opioid Signaling Via Enhancement of Atf6-Dependent Cellular Stress Responses
RESEARCH ARTICLE Disease Models & Mechanisms 6, 146-159 (2013) doi:10.1242/dmm.009852 Glafenine-induced intestinal injury in zebrafish is ameliorated by -opioid signaling via enhancement of Atf6-dependent cellular stress responses Jason R. Goldsmith1, Jordan L. Cocchiaro2, John F. Rawls2,3,*,‡ and Christian Jobin1,3,4,*,‡ SUMMARY Beside their analgesic properties, opiates exert beneficial effects on the intestinal wound healing response. In this study, we investigated the role of -opioid receptor (MOR) signaling on the unfolded protein response (UPR) using a novel zebrafish model of NSAID-induced intestinal injury. The NSAID glafenine was administered to zebrafish larvae at 5 days post-fertilization (dpf) for up to 24 hours in the presence or absence of the MOR- specific agonist DALDA. By analysis with histology, transmission electron microscopy and vital dye staining, glafenine-treated zebrafish showed evidence of endoplasmic reticulum and mitochondrial stress, with disrupted intestinal architecture and halted cell stress responses, alongside accumulation of apoptotic intestinal epithelial cells in the lumen. Although the early UPR marker BiP was induced with glafenine-induced injury, downstream atf6 and s-xbp1 expression were paradoxically not increased, explaining the halted cell stress responses. The -opioid agonist DALDA protected against glafenine-induced injury through induction of atf6-dependent UPR. Our findings show that DALDA prevents glafenine-induced epithelial damage through induction of effective UPR. DMM INTRODUCTION importance of the epithelium in maintaining intestinal homeostasis, Intestinal homeostasis is achieved in part by the maintenance of a understanding mechanisms involved in intestinal epithelial healing functional barrier composed of a single layer of intestinal epithelial and cell stress responses, and the identification of compounds that cells (IEC), which separates the host from the highly antigenic promote these processes, could lead to new therapeutic strategies lumenal milieu (Sartor, 2008). -

Download Product Insert (PDF)
PRODUCT INFORMATION Deracoxib Item No. 27371 CAS Registry No.: 169590-41-4 O H2N Formal Name: 4-[3-(difluoromethyl)-5-(3-fluoro- S O 4-methoxyphenyl)-1H-pyrazol-1- yl]-benzenesulfonamide F Synonym: SC-59046 O MF: C17H14F3N3O3S 397.4 FW: N Purity: ≥98% N UV/Vis.: λmax: 256 nm Supplied as: A solid Storage: -20°C F Stability: ≥2 years F Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Deracoxib is supplied as a solid. A stock solution may be made by dissolving the deracoxib in the solvent of choice, which should be purged with an inert gas. Deracoxib is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of deracoxib in ethanol is approximately 3 mg/ml and approximately 10 mg/ml in DMSO and DMF. Deracoxib is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, deracoxib should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Deracoxib has a solubility of approximately 0.1 mg/ml in a 1:8 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Deracoxib is a non-steroidal anti-inflammatory drug (NSAID) and selective inhibitor of COX-2 1 (IC50s = 0.63 and 23 μM for COX-2 and COX-1, respectively). In vivo, deracoxib (0.3-10 mg/kg) increases weight bearing and decreases lameness and joint effusion in a canine model of urate crystal-induced intraarticular synovitis.2 Deracoxib induces less lesion formation in the gastric mucosa of healthy canines than aspirin (Item No. -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine -

Product Monograph
PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets NSAID Analgesic Agent Novopharm Limited Date of Revision: Toronto, Canada August 02, 2007 Control Number 112565 PRODUCT MONOGRAPH NOVO–KETOROLAC (ketorolac tromethamine) 10 mg Tablets THERAPEUTIC CLASSIFICATION NSAID Analgesic Agent ACTION AND CLINICAL PHARMACOLOGY NOVO-KETOROLAC (ketorolac tromethamine) is a non-steroidal anti-inflammatory drug (NSAID) that has analgesic activity. It is considered to be a peripherally acting analgesic. It is thought to inhibit the cyclo-oxygenase enzyme system, thereby inhibiting the synthesis of prostaglandins. At analgesic doses it has minimal anti-inflammatory and antipyretic activity. The peak analgesic effect occurs at 2 to 3 hours post-dosing with no evidence of a statistically significant difference over the recommended dosage range. The greatest difference between large and small doses of administered ketorolac is in the duration of analgesia. Following oral administration, ketorolac tromethamine is rapidly and completely absorbed, and pharmacokinetics are linear following single and multiple dosing. Steady state plasma levels are achieved after one day of q.i.d. dosing. - 2 - Peak plasma concentrations of 0.7 to 1.1 µg/mL occurred at 44 minutes following a single oral dose of 10 mg. The terminal plasma elimination half-life ranged between 2.4 and 9 hours in healthy adults, while in the elderly subjects (mean age: 72 years) it ranged between 4.3 and 7.6 hours. A high fat meal decreased the rate but not the extent of absorption of oral ketorolac tromethamine, while antacid had no effect. In renally impaired patients there is a reduction in clearance and an increase in the terminal half- life of ketorolac tromethamine (See Table 1). -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

Dog Owner Information About ® Chewable Tablets (Carprofen)
Dog Owner Information about ® Chewable Tablets (carprofen) ® Caplets (carprofen, USP) Rimadyl® (pronounced “Rim-a-dill”) for Osteoarthritis and Post-Surgical Pain Generic name: carprofen (“car-pro-fen”) This summary contains important information about Rimadyl. You should read this What are the possible side effects that may occur in my dog during information before you start giving your dog Rimadyl and review it each time the Rimadyl therapy? prescription is refilled. This sheet is provided only as a summary and does not take Rimadyl, like other drugs, may cause some side effects. Serious but rare side effects the place of instructions from your veterinarian. Talk to your veterinarian if you do not have been reported in dogs taking NSAIDs, including Rimadyl. Serious side effects can understand any of this information or if you want to know more about Rimadyl. occur with or without warning and in rare situations result in death. What is Rimadyl? The most common NSAID-related side effects generally involve the stomach (such as Rimadyl is a nonsteroidal anti-inflammatory drug (NSAID) that is used to reduce pain bleeding ulcers), and liver or kidney problems. Look for the following side effects that and inflammation (soreness) due to osteoarthritis and pain following surgery in dogs. can indicate your dog may be having a problem with Rimadyl or may have another Rimadyl is a prescription drug for dogs. It is available as a caplet and chewable tablet medical problem: and is given to dogs by mouth. • Decrease or increase in appetite Osteoarthritis -
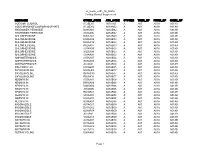
Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01