A034047-100 Top Secrets.Qxd 5/18/06 2:32 PM Page 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
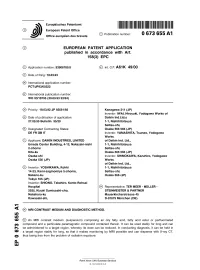
Mri Contrast Medium and Diagnostic Method
Europa.schesP— || | MMMMI 1 1||||| 1 1 1 1 1 1||| || J European Patent Office _ o it r- a 4 © Publication number: 0 673 655 A1 Office_„. europeen des brevets © EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC © Application number: 93906789.8 © Int. CI.6: A61 K 49/00 @ Date of filing: 18.03.93 © International application number: PCT/JP93/00322 © International publication number: WO 93/18795 (30.09.93 93/24) ® Priority: 19.03.92 JP 93561/92 Kanagawa 211 (JP) Inventor: IWAI, Hlroyuki, Yodogawa Works of @ Date of publication of application: Daikin Ind.Ltd.s 27.09.95 Bulletin 95/39 1-1, Nlshlhltotsuya Settsu-shl, © Designated Contracting States: Osaka 566 566 (JP) DE FR GB IT Inventor: YAMASHITA, Tsuneo, Yodogawa Works © Applicant: DAIKIN INDUSTRIES, LIMITED of Daikin Ind. Ltd., Umeda Center Building, 4-12, Nakazaki-nishi 1-1, Nishihitotsuya 2-chome Settsu-shi, Kita-ku Osaka 566 566 (JP) Osaka-shi Inventor: SHIMOKAWA, Kazuhiro, Yodogawa Osaka 530 (JP) Works of Daikin Ind. Ltd., © Inventor: YOSHIKAWA, Kohki 1-1, Nishihitotsuya 14-23, Kami-saginomiya 5-chome, Settsu-shi, Nakano-ku Osaka 566 (JP) Tokyo 165 (JP) Inventor: SHIONO, Takahiro, Kanto Rohsai Hospital © Representative: TER MEER - MULLER - 2035, Kizuki Sumiyoshi-cho, STEINMEISTER & PARTNER Nakahara-ku Mauerkircherstrasse 45 Kawasaki-shi, D-81679 Munchen (DE) ^ © MRI CONTRAST MEDIUM AND DIAGNOSTIC METHOD. in m CO © An MRI contrast medium (suspension) comprising an oily fatty acid, fatty acid ester or perfluorinated compound and a particulate paramagnetic compound contained therein. It can be used stably for long and can ^ be administered to a target region, whereby its dose can be reduced. -

Genitourinary Pathology (Including Renal Tumors)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS GENITOURINARY PATHOLOGY (INCLUDING RENAL TUMORS) (776-992) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -

Caracterización Fisicoquímica Y Clínica De Los Medios De Contraste Intravasculares Iodados
Anales de Radiología México 2008;2:129-140. ARTÍCULOS DE REVISIÓN Dra. Patricia Rodríguez Nava,1 Dr. Ernesto J. Dena Espinoza,1 Caracterización fisicoquímica y Dr. Roberto Basile Lenge,2 Dra. Margarita Fuentes García,3 clínica de los medios de contraste Dr. Gustavo Fink Josephi,4 Dr. Eduardo Marbez Namnum1 intravasculares iodados RESUMEN Objetivo: El propósito de sido aceptado por algunos ra- este artículo es realizar una re- diólogos. La lopromida puede Introducción: El uso de visión bibliográfica sobre las ca- ser considerada un agente uni- medios de contraste intravascu- racterísticas, clasificación, pro- versal para todas las explora- lares no iónicos (gas, sustancia piedades físico-químicas, así ciones y procedimientos radio- hidrosoluble o liposoluble) en como los efectos secundarios lógicos. imagenología ha proliferado (quimiotoxicidad) de los medios en los últimos años debido a su de contraste intravasculares no Palabras clave: Medios de excepcional tolerancia por los iónicos. contraste intravasculares ioda- pacientes. La baja osmolalidad Conclusiones: Un factor que dos, medios de contraste ióni- de este tipo de medios de con- interviene en la incidencia de cos, medios de contraste no ió- traste aporta beneficios como reacciones idiosincráticas o aler- nicos. bajo incremento del volumen goides puede ser el estado psi- sanguíneo, baja toxicidad, bajo cológico del paciente. El trata- efecto sobre la barrera hema- miento previo con antihitamíni- toencefálica. cos, corticosteroides o ambos ha continúa en la pág. 130 1 Del Servicio de Radiología e Imagen “Dr. Carlos Coqui” del Hospital General de México osmolalidad o iso-osmolares. En los Estados Unidos 2 3 O.D. De la Universidad de Buenos Aires Cardiología. -

Poster: Publikace 2008
Publikované Práce lékařů Šiklova Patologicko – anatomického ústavu a bioPtické laboratoře s.r.o. za rok 2008 Časopisy s „impact“ faktorem syringofibroadenoma associated with well-differentiated squamous cell 28. Kuroda N., Katto K., Yamaguchi T., Kawada T., ImamuraY., Hes O., Michal M., 42. Vazmitel M., Spagnolo D.V., Němcová J., Michal M., Kazakov D.V.: 1. Alvarado-Cabrero I., Perez-Montiel D.M., Hes, O.: Multicystic urothelial carcinoma. Am J Dermatopathol, 30, 572-574, 2008. Shuin T., Lee G.H.: Chromophobe renal cell carcinoma: Diagnostic ancillary Hidradenoma papilliferum with a ductal carcinoma in situ component. Case report and review of the literature. Am J Dermatopathol, 30, 392-394, 2008. carcinoma of the bladder with gland-like lumina and with signet-ring cells. 17. Kacerovska D., Michal M., Kreuzberg B., Mukensnabl P., Kazakov DV.: application of imprint cytology and fluorescencein situ hybridization of Acral calcified vascular leiomyoma of the skin: a rare clinicopathological chromosomes 10 and 21 in two cases of typical and eosinophilic variants. 43. Vazmitel M., Michal M., Kazakov D.V.: Merkel cell carcinoma with a A case report. Diagn Pathol, 3, 36, 2008. follicular lymphocytic infiltrate: report of two cases. Am J Dermatopathol, 2. Beneš Z., Chlumská A., Antoš Z., Kohout P., Sequens R.: Detection of variant of cutaneous vascular leiomyomas: report of 3 cases. J Amer Acad Med Mol Morphol, 41, 227-232, 2008. 29. Kuroda N., Kato K., Tamura M., Shiotsu T., Hes O., Michal M., Hagashima 30, 389-391, 2008. carcinoma by means of endoscopic cytoscopy in the area of ulcerative colitis. Dermatology, 59,1000-1004, 2008. -

Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours
Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours Hellquist, Henrik; Paiva-Correia, António; Vander Poorten, Vincent; Quer, Miquel; Hernandez- Prera, Juan C; Andreasen, Simon; Zbären, Peter; Skalova, Alena; Rinaldo, Alessandra; Ferlito, Alfio Published in: Advances in Therapy DOI: 10.1007/s12325-019-01007-3 Publication date: 2019 Document version Publisher's PDF, also known as Version of record Document license: CC BY-NC Citation for published version (APA): Hellquist, H., Paiva-Correia, A., Vander Poorten, V., Quer, M., Hernandez-Prera, J. C., Andreasen, S., Zbären, P., Skalova, A., Rinaldo, A., & Ferlito, A. (2019). Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours. Advances in Therapy, 36(8), 1950-1974. https://doi.org/10.1007/s12325-019-01007-3 Download date: 01. okt.. 2021 Adv Ther (2019) 36:1950–1974 https://doi.org/10.1007/s12325-019-01007-3 ORIGINAL RESEARCH Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours Henrik Hellquist . Anto´nio Paiva-Correia . Vincent Vander Poorten . Miquel Quer . Juan C. Hernandez-Prera . Simon Andreasen . Peter Zba¨ren . Alena Skalova . Alessandra Rinaldo . Alfio Ferlito Received: May 2, 2019 / Published online: June 17, 2019 Ó The Author(s) 2019 ABSTRACT to investigate whether an accurate histological diagnosis of the 11 different types of benign Introduction: A vast increase in knowledge of epithelial salivary gland tumours is correlated to numerous aspects of malignant salivary gland any differences in their clinical behaviour. tumours has emerged during the last decade Methods: A search was performed for histolog- and, for several reasons, this has not been the ical classifications, recurrence rates and risks for case in benign epithelial salivary gland malignant transformation, treatment modali- tumours. -

REGISTRATION DOCUMENT 2017 Sommaire
REGISTRATION DOCUMENT 2017 sommaire Interview with History 4 Yves L’Épine, Chief Executive Officer 2 Key figures 6 1 4 THE GUERBET GROUP 9 MANAGEMENT REPORT 55 1.1 History of the Company 9 4.1 Analysis of the Group’s activity and results 55 1.2 Mission and ambition 10 4.2 Major events since the start of 2018 58 1.3 Main consolidated data 10 4.3 Information about internal control 59 1.4 Overview of activities 11 4.4 Risk management and risk factors 60 1.5 Industrial and logistics activity 17 4.5 Other legal information 64 1.6 Research and Development 18 1.7 The Group’s governance structure at December 31, 2017 22 5 CORPORATE SOCIAL RESPONSIBILITY 69 2 Employee information 70 CORPORATE GOVERNANCE 27 5.1 5.2 Environmental information 76 2.1 Report of the Board of Directors on 5.3 Social information 80 corporate governance 27 5.4 Report by one of the Statutory Auditors, 2.2 Board of Directors 27 designated as an independent third-party, 2.3 General Management 38 on the consolidated human resources, 2.4 Compensation of company officers 38 environmental and social information 2.5 Agreements referred to in Article L. 225- included in the management report 82 37-4-2° of the French Commercial Code 45 2.6 Provisions in the articles of association 6 relating to General Meetings of Shareholders 46 FINANCIAL STATEMENTS 2.7 Deviations from the recommendations for the composition of the Board of AND RELATED NOTES 85 Directors and the Committees 47 6.1 Consolidated financial statements and notes 86 2.8 Other information from the corporate 6.2 Statutory -

Structure and Properties of X-Ray Contrast Media
STRUCTURE AND PROPERTIES OF X-RAY CONTRAST MEDIA Optimal use of CM in radiology requires a knowl- edge of the nature and relevant properties of the available substances. This chapter describes the properties of currently used and newly developed contrast-giving agents that infuence their behav- ior in the human body, their side effects, and their practical utility. The main X-ray contrast agents in use today are insoluble barium sulfate for the diagnostic evalu- ation of the GI tract and water-soluble CM for the radiological assessment of the different vascular systems, body cavities and organs. In addition, a water-soluble CM based on tri-iodobenzene is the alternative agent of choice for oral use when bari- um sulfate is contraindicated. Barium Sulfate Barium is used in the form of the insoluble sulfate for radiography of the GI tract. If perforation is suspected, however, only water-soluble, iodinated agents (Gastrografn, Ultravist-370) can be used since the body is virtually incapable of eliminating barium sulfate once it has entered the peritoneum. Barium sulfate is available either as a powder to be prepared directly before use or as a ready-to-use suspension. For double-contrast examinations (fll- ing of the lumen with gas, coating of the wall with barium sulfate), barium sulfate is either mixed with a carbon dioxide additive, or a gas-forming agent is taken in addition. © The Author(s) 2018 20 U. Speck, X-Ray Contrast Media, https://doi.org/10.1007/978-3-662-56465-3_3 Common to all barium preparations is concentra- tion of barium sulfate which may diluted according to the needs of the examination. -

Title Acta Urologica Japonica Vol. 35, 1989 Author(S)
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Title Acta Urologica Japonica Vol. 35, 1989 Author(s) Citation 泌尿器科紀要 (1989), 35(12): xii-xxvii Issue Date 1989-12 URL http://hdl.handle.net/2433/116762 Right Type Others Textversion publisher Kyoto University xll Acta Urologica Japonica Vol. 35, 1989 Vol. 35, No. 1January 1989 Study on Urinary (3-Glucuronidaseand Alkaline Phosphatase Activities as Indicators of CDDP Renal Toxicity ...............T. Takahashi et al.••• I Transurethral Ureterolithotripsy under Hydraulic Ureteral Dilatation .................................................................................Y. Mori et al.••• 7 Significanceof Isoantigen in the Managemantof the Urinary Bladder Tumor —A Basic Study of ABO Isoantigen in Step Sections of Entire Bladder—.................................................................................T. Ogawa et al.••• 13 An Experimental Study on Bladder Carcinogenesisin Dogs by N-Butyl-N-(4-Hydroxybutyl)Nitrosamine (BBN) and its Urinary Metabolites ............................................................S. Morishita et al.••• 27 A New Clinical Trial Intravesical Chemotherapywith Instillation of Peplomycin Preparation Emulsion in Hydroxypropylcellulosum —PreliminaryStudy of Patients with Bladder Tumor—.........M. Asakawa et al.••• 39 Studies of the New Parameter Based Urinary Flow Rate Curve in Benign Prostatic Hypertrophy ......................................................C. Haraguchi••• -

Comprehensive Inherited Cancer Precision Panel Overview
Comprehensive Inherited Cancer Precision Panel Overview Hereditary cancer syndromes are encountered in all medical specialties. Although they account for about 5% of all malignancies, it is of special importance to identify these patients because, unlike patients with sporadic cancers, they require special, long-term care as their predisposition can cause them to develop certain tumors at a relatively early age. These cancers can arise in the lungs, kidneys, liver, pancreas, skin, eyes, heart. Most hereditary cancers are associated with a “germline mutation” that will be present in every cell of the human body. Identification of patients at risk of inherited cancer susceptibility is dependent upon the ability to characterize genes and alterations associated with increased cancer risk as well as gathering a detailed personal and family history aiding in the identification of the mode of inheritance as well as other family members at risk of suffering from this susceptibility. Most hereditary cancer syndromes follow an autosomal dominant inheritance, and the penetrance is high. The Igenomix Comprehensive Inherited Cancer Precision Panel provides a comprehensive analysis of the most common hereditary cancer syndromes using next-generation sequencing (NGS) to fully understand the spectrum of relevant cancer predisposition genes. Indications The Igenomix Comprehensive Inherited Caner Precision Panel is indicated as a screening and diagnostic test in those cases where there are: ‐ Multiple relatives on the same side of the family with the same or related forms of cancer ‐ Cancer at an early age ‐ Early presentation of an aggressive cancer type ‐ Multiple primary cancers in an individual 1 Clinical Utility The clinical utility of this panel is: ‐ Early and accurate genetic diagnosis allowing the most appropriate clinical management of a patient with personal or family history suggestive of a hereditary cancer syndrome. -

Q35;Ql3) Breakpoint
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/25861 Please be advised that this information was generated on 2021-09-25 and may be subject to change. ELSEVIER Fine Mapping of the Human Renal Oncocytoma- Associated Translocation (5;ll)(q35;ql3) Breakpoint Richard J. Sinke, Trynie Dijkhuizen, Bert Janssen, Daniël Olde Weghuis, Gérard Merkx, Eva van den Berg, Ed Schuuring, Aurelia M. Meloni, Bauke de Jong, and Ad Geurts van Kessel ABSTRACT: Recent cytogenetic analysis of a series of human renal oncocytomas revealed the presence of a recurring chromosomal translocation (5;ll)(q35;ql3) as sole anomaly in a subset of the tumors. The molecular characterization of this translocation was initiated using two primary t(5;ll)-positive renal oncocytomas and a panel of soma tic cell hybrids derived from one of these tumors, in conjunction with fluorescence in situ hybridization (FISH) and Southern blot analysis. The breakpoint in chromosome band llql3 could be located within a genomic interval of at maximum 400 Kb immediately centromeric to the BCLl locus. © Elsevier Science Inc., 1997 INTRODUCTION cytogenetic anomaly in at least 3 independent cases and, as such, should be considered as a primary change. Deletion of Oncocytomas are benign tumors that occur predominantly 3p material that occurs in the majority of renal cell carci in the kidney, accounting for approximately 5% of all pri nomas [16,17] has not been observed in renal oncocytomas. mary tumors at that site. -

2015 DQC Review of Answers
Question 1 A 55-year-old gentleman is referred for Mohs surgery of a biopsy positive metatypical basal cell carcinoma of the R lateral forehead. Based on the findings on this slide what additional tests would you consider? A. Send tissue for CK 20 staining. B. Order a CT to look for pulmonary changes/renal oncocytoma. C. Send tissue for MLH-1, and MSH-2 and 6 staining. D. Check thyroid function tests. Discussion Question 1 Correct Answer: C. Send tissue for MLH-1, and MSH-2 and 6 staining. Main Histologic Features: • Dermal neoplasm with sebaceous differentiation throughout the tumor • Significant mitotic activity with atypical mitoses • No peripheral palisading or peritumoral mucin • Incidental overlying squamous cell carcinoma in situ Differential Diagnosis: • Basal cell carcinoma with sebaceous differentiation • Sebaceoma • Trichilemmal carcinoma • Granular cell tumor Clinical Concerns: • Facial neoplasms can be associated with systemic syndromes: Fibrofolliculomas/trichodiscomas seen in Birt-Hogg-Dubé syndrome 80-90% risk of pulmonary cysts 15-20% risk of renal cancer, particularly oncocytoma Trichilemmomas seen in Cowden syndrome Thyroid involved in 66% of cases Malignancy develops in at least 40% of patients. • Sebaceous neoplasms can be seen in Muir-Torre syndrome (MTS) which carries an increased risk of colon, genitourinary, breast and hematologic malignancies. • MTS is more commonly associated with extraocular sebaceous carcinomas. • MTS can be screened for by using immunohistochemical tissue stains for MLH-1, MSH-2 and MSH-6 proteins (Muir-Torre panel). Absence of staining identifies tumors with mismatch repair deficiency and suggests MTS, which can then be confirmed by genetic testing. References: • Ansai S, Takeichi H, Arase S, Kawana S, Kimura T. -

Renal Oncocytoma with Invasive Histopathologic Features – Case Report
CASE REPORT Renal Oncocytoma with Invasive Histopathologic Features – Case Report Renálny onkocytóm s histologickými črtami invázie – kazuistika Kolníková G.1, Marinová P.1, Gál V.1, Mečiarová I.1, Mišanko V.2, Rampalová J.1, Jáni P.1, Orthová S.1, Ondriaš F.1, Caňo M.2 1 Division of Pathology, Alpha Medical Patologia l.t.d., Bratislava- Ružinov, Slovak Republic 2 Department of Urology, University Hospital Bratislava- Ružinov, Slovak Republic Summary Background: Renal oncocytoma is an uncommon tumor, classifi ed as a benign renal neoplasm Autoři deklarují, že v souvislosti s předmětem in the World Health Organisation classifi cation of renal tumours. Despite it there were descri- studie nemají žádné komerční zájmy. bed several reports with invasive histopathologic features. Case report: We describe a case of The authors declare they have no potential renal oncocytoma with bizzare cells and invasion of renal sinus fat tissue. We performed immu- confl icts of interest concerning drugs, products, nohistochemical analysis of the case and a review of relevant literature. Conclusion: In order to or services used in the study. set up the right dia gnosis the perfect co- operation of clinicians and pathologists is necessary. Redakční rada potvrzuje, že rukopis práce In our opinion, in accordance with other authors, the renal oncocytomas should be considered splnil ICMJE kritéria pro publikace zasílané do bi omedicínských časopisů. as having a very low rather than no malignant potential, in spite of clinically benign behavior, supplementing a hypothesis, whether renal oncocytomas may be considered as a precance- The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for rous lesion of chromophobe carcinoma.