Comparison of Immunological Characteristics Between Paired
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Variants and Clinical Significance of Pediatric Acute Lymphoblastic Leukemia
296 Original Article Page 1 of 11 Genetic variants and clinical significance of pediatric acute lymphoblastic leukemia Hong-Hong Zhang1,2#, Hong-Sheng Wang1,2#, Xiao-Wen Qian1,2, Cui-Qing Fan2, Jun Li1,2, Hui Miao1,2, Xiao-Hua Zhu1,2, Yi Yu1,2, Jian-Hua Meng1,2, Ping Cao1,2, Jun Le1,2, Jun-Ye Jiang1,2, Wen-Jing Jiang1,2, Ping Wang1,2, Xiao-Wen Zhai1,2 1Department of Hematology and Oncology, 2Department of Pediatrics, Children’s Hospital of Fudan University, Shanghai 201102, China Contributions: (I) Conception and design: HH Zhang, HS Wang; (II) Administrative support: XW Zhai; (III) Provision of study materials or patients: XW Qian, J Li, WJ Jiang, P Wang; (IV) Collection and assembly of data: H Miao, XH Zhu, JY Jiang, CQ Fan, J Le; (V) Data analysis and interpretation: Y Yu, JH Meng, P Cao, HH Zhang, HS Wang; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Xiao-Wen Zhai. Department of Hematology and Oncology, Children’s Hospital of Fudan University, 399 Wanyuan Road, Shanghai 201102, China. Email: [email protected]. Background: Acute lymphoblastic leukemia (ALL), the most common childhood malignancy, is characterized by molecular aberrations. Recently, genetic profiling has been fully investigated on ALL; however, the interaction between its genetic alterations and clinical features is still unclear. Therefore, we investigated the effects of genetic variants on ALL phenotypes and clinical outcomes. Methods: Targeted exome sequencing technology was used to detect molecular profiling of 140 Chinese pediatric patients with ALL. -

Ras Pathway Mutation Feature in the Same Individuals at Diagnosis and Relapse of Childhood Acute Lymphoblastic Leukemia
12 Original Article Ras pathway mutation feature in the same individuals at diagnosis and relapse of childhood acute lymphoblastic leukemia Hong-Hong Zhang1#, Hong-Sheng Wang1#, Xiao-Wen Qian1, Xiao-Hua Zhu1, Hui Miao1, Yi Yu1, Jian-Hua Meng1, Jun Le1, Jun-Ye Jiang1, Ping Cao1, Wen-Jing Jiang1, Ping Wang1, Yang Fu1, Jun Li1, Mao-Xiang Qian2, Xiao-Wen Zhai1 1Department of Hematology, 2Institute of Pediatrics, Children’s hospital of Fudan University, Shanghai 201102, China Contributions: (I) Conception and design: HH Zhang, HS Wang; (II) Administrative support: XW Zhai; (III) Provision of study materials or patients: XW Qian, XH Zhu, H Miao, Y Yu; (IV) Collection and assembly of data: JH Meng, J Le, Y Fu, JY Jiang, WJ Jiang, MX Qian; (V) Data analysis and interpretation: P Cao, P Wang, J Li, HH Zhang, HS Wang, XW Zhai; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Xiao-Wen Zhai. Department of Hematology, Children’s hospital of Fudan University, No. 399 Wanyuan Road, Shanghai 201102, China. Email: [email protected]. Background: Acute lymphoblastic leukemia (ALL) is the most common malignancy in children, while relapse and refractory ALL remains a leading cause of death in children. However, paired ALL samples of initial diagnosis and relapse subjected to next-generation sequencing (NGS) could construct clonal lineage changes, and help to explore the key issues in the evolutionary process of tumor clones. Therefore, we aim to analyze gene alterations during the initial diagnosis and relapse of ALL patients and to explore the underlying mechanism. -

Tongguang Zhai ————————————————————————————————
Tongguang Zhai ———————————————————————————————— Tel no: (859) 257-4958 (office) Postal address: 163B F. Paul Anderson Tower (859) 396-0924 (home) Department of Chemical & Materials Engineering E-mail: [email protected] University of Kentucky Lexington, Kentucky 40506, USA Academic Degrees D.Phil. (Ph.D.), 9/1994 B.Sc., 7/1983 University of Oxford, England University of Science and Technology Beijing, China Research Interests • Fatigue life prediction: identification of fatigue weak-link density and strength distribution, quantification of fatigue crack initiation and resistance to fatigue crack growth due to crack deflection at grain boundaries, • Optimum alloy design through micro- and macro-texture control, • Failure analysis, Materials characterisation, processing and modelling, etc. Education and Career 6/2007—Present Associate Professor Department of Chemical and Materials Engineering University of Kentucky, Lexington, KY 40506-0046, USA 8/2001—5/2007 Assistant Professor Department of Chemical and Materials Engineering University of Kentucky, Lexington, KY 40506-0046, USA 8/2000—6/2001 Postdoctoral Research Associate Light metals research center, Department of Chemical and Materials Engineering, University of Kentucky, Lexington, KY 40506-0046, USA 1/1995—7/2000 Research fellow Department of Materials, University of Oxford 10/1994—12/1994 Research Assistant Fraunhofer Institute for NDT (IzfP), University Building 37, 66123 Saarbrueken, Germany 10/1991—9/1994 D. Phil. student Department of Materials, University of Oxford Academic Awards and Honours ● NSF CAREER AWARD: 7/2007-6/2012 ● Visiting Professorship: University of Hong Kong (June, 2009), Sichuan University (June, 2005). ● Excellent Teacher Award by College of Engineering, University of Kentucky, 2002/2003. ● Buehler Technical Merit Paper Award, 4/1994, jointly by International Metallography Society and Materials Characterisation, Paper 48) in the publication list. -
Deanxit Relieves Symptoms in a Patient with Jackhammer Esophagus: a Case Report
Submit a Manuscript: http://www.f6publishing.com World J Gastrointest Endosc 2017 December 16; 9(12): 590-593 DOI: 10.4253/wjge.v9.i12.590 ISSN 1948-5190 (online) CASE REPORT Deanxit relieves symptoms in a patient with jackhammer esophagus: A case report Jin-Ying Li, Wen-Huan Zhang, Chun-Ling Huang, Dang Huang, Guo-Wen Zuo, Lie-Xin Liang Jin-Ying Li, Wen-Huan Zhang, Chun-Ling Huang, Dang Huang, Revised: October 25, 2017 Guo-Wen Zuo, Lie-Xin Liang, Department of Gastroenterology, Accepted: November 11, 2017 People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning Article in press: November 11, 2017 530021, Guangxi Zhuang Autonomous Region, China Published online: December 16, 2017 ORCID number: Jin-Ying Li (0000-0002-4101-1553); Wen- Huan Zhang (0000-0002-4362-7378); Chun-Ling Huang (0000- 0001-5512-173X); Dang Huang (0000-0003-2447-8319); Guo- Wen Zuo (0000-0002-3100-937X); Lie-Xin Liang (0000- Abstract 0002-2029-5059). Jackhammer (hypercontractile) esophagus presents with dysphagia and chest pain. Current treatments are Author contributions: Zuo GW designed the report; Li JY limited. We describe a 60-year-old man who presented collected references and prepared the manuscript, with the help with dysphagia, chest pain and heartburn for a period of Huang D; Zhang WH and Huang CL provided the figures; Zuo of 1 year. His workup showed Barrett’s esophagus on GW and Liang LX supervised the preparation of the manuscript. endoscopy and high-resolution manometry demonstrated Informed consent statement: The patient involved in this jackhammer esophagus with esophagogastric junction study gave his written informed consent authorizing use and outflow obstruction. -
Gateless Gate Has Become Common in English, Some Have Criticized This Translation As Unfaithful to the Original
Wú Mén Guān The Barrier That Has No Gate Original Collection in Chinese by Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Page ii Frontspiece “Wú Mén Guān” Facsimile of the Original Cover Page iii Page iv Wú Mén Guān The Barrier That Has No Gate Chán Master Wúmén Huìkāi (1183-1260) Questions and Additional Comments by Sŏn Master Sǔngan Compiled and Edited by Paul Dōch’ŏng Lynch, JDPSN Sixth Edition Before Thought Publications Huntington Beach, CA 2010 Page v BEFORE THOUGHT PUBLICATIONS HUNTINGTON BEACH, CA 92648 ALL RIGHTS RESERVED. COPYRIGHT © 2010 ENGLISH VERSION BY PAUL LYNCH, JDPSN NO PART OF THIS BOOK MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM OR BY ANY MEANS, GRAPHIC, ELECTRONIC, OR MECHANICAL, INCLUDING PHOTOCOPYING, RECORDING, TAPING OR BY ANY INFORMATION STORAGE OR RETRIEVAL SYSTEM, WITHOUT THE PERMISSION IN WRITING FROM THE PUBLISHER. PRINTED IN THE UNITED STATES OF AMERICA BY LULU INCORPORATION, MORRISVILLE, NC, USA COVER PRINTED ON LAMINATED 100# ULTRA GLOSS COVER STOCK, DIGITAL COLOR SILK - C2S, 90 BRIGHT BOOK CONTENT PRINTED ON 24/60# CREAM TEXT, 90 GSM PAPER, USING 12 PT. GARAMOND FONT Page vi Dedication What are we in this cosmos? This ineffable question has haunted us since Buddha sat under the Bodhi Tree. I would like to gracefully thank the author, Chán Master Wúmén, for his grace and kindness by leaving us these wonderful teachings. I would also like to thank Chán Master Dàhuì for his ineptness in destroying all copies of this book; thankfully, Master Dàhuì missed a few so that now we can explore the teachings of his teacher. -
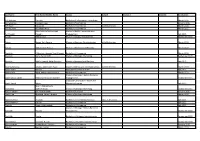
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation
Last Name First Name/Middle Name Course Award Course 2 Award 2 Graduation A/L Krishnan Thiinash Bachelor of Information Technology March 2015 A/L Selvaraju Theeban Raju Bachelor of Commerce January 2015 A/P Balan Durgarani Bachelor of Commerce with Distinction March 2015 A/P Rajaram Koushalya Priya Bachelor of Commerce March 2015 Hiba Mohsin Mohammed Master of Health Leadership and Aal-Yaseen Hussein Management July 2015 Aamer Muhammad Master of Quality Management September 2015 Abbas Hanaa Safy Seyam Master of Business Administration with Distinction March 2015 Abbasi Muhammad Hamza Master of International Business March 2015 Abdallah AlMustafa Hussein Saad Elsayed Bachelor of Commerce March 2015 Abdallah Asma Samir Lutfi Master of Strategic Marketing September 2015 Abdallah Moh'd Jawdat Abdel Rahman Master of International Business July 2015 AbdelAaty Mosa Amany Abdelkader Saad Master of Media and Communications with Distinction March 2015 Abdel-Karim Mervat Graduate Diploma in TESOL July 2015 Abdelmalik Mark Maher Abdelmesseh Bachelor of Commerce March 2015 Master of Strategic Human Resource Abdelrahman Abdo Mohammed Talat Abdelziz Management September 2015 Graduate Certificate in Health and Abdel-Sayed Mario Physical Education July 2015 Sherif Ahmed Fathy AbdRabou Abdelmohsen Master of Strategic Marketing September 2015 Abdul Hakeem Siti Fatimah Binte Bachelor of Science January 2015 Abdul Haq Shaddad Yousef Ibrahim Master of Strategic Marketing March 2015 Abdul Rahman Al Jabier Bachelor of Engineering Honours Class II, Division 1 -

The Historical Origin of the Chinese Taoist and Tai Chi
DOI: 10.7763/IPEDR. 2012. V58. 25 The Historical Origin of the Chinese Taoist and Tai Chi Jian-sheng Wen1and Min Su Department of Physical Education of Northwestern Polytechnical University, ShaanxiXi´an, 710072 Abstract. Chinese martial arts and Taoism has a long historical origin, this article reveals that the formation of tai chi means traditional Chinese Taoist culture having a clear external expression form, at the same time having bidirectional authentication method (inward regimen validated and outward fighting verified). When Chinese Taoists to Zhang Sanfeng, Inner life cultivation and life formed holographic deduction in the universe had been completed. Marking the Taoist introverted experience practicing was already clear and maturation. But the Taoist within the practice also needs external practicing avenue and intuitive form. Finally in the right historical period, Taoism and the martial art met. Keywords: Taoism, Chinese Martial Art, Tai Chi, Life Cultivation, Zhang San-feng. 1. Introduction Yang style, etc. every style tai chi respects Zhang San feng for the founder. Either from tai chi name or from the statue of the founder, Taoist and tai chi both have a deeply historical origin,and means that The two value orientations are convergence. In modern times, many tai chi practitioners, tai chi has become one of the world's most widespread categories of traditional Chinese culture. People can generally feel the the Taoist culture behind it, but the Taoist culture system is still to make people feel mysterious. What the intrinsic link is between the two? Whether can have a glimpse of the true face of the Taoist culture through tai chi? This article reveals that the formation of tai chi means traditional Chinese Taoist culture having a clear external expression form, at the same time having bidirectional authentication method (inward regimen validated and outward fighting verified). -

Clinical Significance of Common-Stem Lenticulostriate Arteries in Patients with Internal Watershed Infarction
Neurological Sciences (2019) 40:2303–2309 https://doi.org/10.1007/s10072-019-03953-w ORIGINAL ARTICLE Clinical significance of common-stem lenticulostriate arteries in patients with internal watershed infarction Wen -huo Chen1 & Ting-yu Yi1 & A-lai Zhan2 & Yan-min Wu1 & Mei-fang Zhang1 & Yi-min Li2 & Yan-yu Lu2 & Ding-lai Lin1 & Xiao-hui Lin1 & Zhi-nan Pan1 Received: 18 January 2019 /Accepted: 27 May 2019 /Published online: 16 June 2019 # Fondazione Società Italiana di Neurologia 2019 Abstract Background A common-stem origin of lenticulostriate arteries (CS-LSAs) is an anatomical variation that supplies a moderate to large section of the basal ganglia. We hypothesized that CS-LSAs with a patent orifice are located at distal positions of the acute- occluded middle cerebral artery (MCA) and that the blood flow of CS-LSAs is supplied by pail arterial anastomoses and results in hypoperfusion of CS-LSAs, similar to a deep watershed (DWS) infarction. Objective Our study evaluated the possibility of CS-LSAs in patients with DWS infarction and MCA occlusion and also assessed the safety of endovascular therapy (ET) in these patients. Methods A cohort of consecutive patients with DWS infarction and MCA occlusion and in whom full recanalization via ET was achieved were identified. Patients were divided into two groups based on the presence of CS-LSAs observed during ET. In addition, radiological and clinical data were retrospectively analyzed. Results Thirty-three patients were included, and CS-LSAs were observed in 48.5% (16/33) of patients. The possibility (72.2%, 13/18) of CS-LSAs was high in patients with DWS infarction companied with basal ganglia infarction. -

English Versions of Chinese Authors' Names in Biomedical Journals
Dialogue English Versions of Chinese Authors’ Names in Biomedical Journals: Observations and Recommendations The English language is widely used inter- In English transliteration, two-syllable Forms of Chinese Authors’ Names nationally for academic purposes. Most of given names sometimes are spelled as two in Biomedical Journals the world’s leading life-science journals are words (Jian Hua), sometimes as one word We recently reviewed forms of Chinese published in English. A growing number (Jianhua), and sometimes hyphenated authors’ names accompanying English- of Chinese biomedical journals publish (Jian-Hua). language articles or abstracts in various abstracts or full papers in this language. Occasionally Chinese surnames are Chinese and Western biomedical journals. We have studied how Chinese authors’ two syllables (for example, Ou-Yang, Mu- We found considerable inconsistency even names are presented in English in bio- Rong, Si-Ma, and Si-Tu). Editors who are within the same journal or issue. The forms medical journals. There is considerable relatively unfamiliar with Chinese names were in the following categories: inconsistency. This inconsistency causes may mistake these compound surnames for • Surname in all capital letters followed by confusion, for example, in distinguishing given names. hyphenated or closed-up given name, for surnames from given names and thus cit- China has 56 ethnic groups. Names example, ing names properly in reference lists. of minority group members can differ KE Zhi-Yong (Chinese Journal of In the current article we begin by pre- considerably from those of Hans, who Contemporary Pediatrics) senting as background some features of constitute most of the Chinese population. GUO Liang-Qian (Chinese Chinese names. -

Representing Talented Women in Eighteenth-Century Chinese Painting: Thirteen Female Disciples Seeking Instruction at the Lake Pavilion
REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION By Copyright 2016 Janet C. Chen Submitted to the graduate degree program in Art History and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. ________________________________ Chairperson Marsha Haufler ________________________________ Amy McNair ________________________________ Sherry Fowler ________________________________ Jungsil Jenny Lee ________________________________ Keith McMahon Date Defended: May 13, 2016 The Dissertation Committee for Janet C. Chen certifies that this is the approved version of the following dissertation: REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION ________________________________ Chairperson Marsha Haufler Date approved: May 13, 2016 ii Abstract As the first comprehensive art-historical study of the Qing poet Yuan Mei (1716–97) and the female intellectuals in his circle, this dissertation examines the depictions of these women in an eighteenth-century handscroll, Thirteen Female Disciples Seeking Instructions at the Lake Pavilion, related paintings, and the accompanying inscriptions. Created when an increasing number of women turned to the scholarly arts, in particular painting and poetry, these paintings documented the more receptive attitude of literati toward talented women and their support in the social and artistic lives of female intellectuals. These pictures show the women cultivating themselves through literati activities and poetic meditation in nature or gardens, common tropes in portraits of male scholars. The predominantly male patrons, painters, and colophon authors all took part in the formation of the women’s public identities as poets and artists; the first two determined the visual representations, and the third, through writings, confirmed and elaborated on the designated identities. -

Names of Chinese People in Singapore
101 Lodz Papers in Pragmatics 7.1 (2011): 101-133 DOI: 10.2478/v10016-011-0005-6 Lee Cher Leng Department of Chinese Studies, National University of Singapore ETHNOGRAPHY OF SINGAPORE CHINESE NAMES: RACE, RELIGION, AND REPRESENTATION Abstract Singapore Chinese is part of the Chinese Diaspora.This research shows how Singapore Chinese names reflect the Chinese naming tradition of surnames and generation names, as well as Straits Chinese influence. The names also reflect the beliefs and religion of Singapore Chinese. More significantly, a change of identity and representation is reflected in the names of earlier settlers and Singapore Chinese today. This paper aims to show the general naming traditions of Chinese in Singapore as well as a change in ideology and trends due to globalization. Keywords Singapore, Chinese, names, identity, beliefs, globalization. 1. Introduction When parents choose a name for a child, the name necessarily reflects their thoughts and aspirations with regards to the child. These thoughts and aspirations are shaped by the historical, social, cultural or spiritual setting of the time and place they are living in whether or not they are aware of them. Thus, the study of names is an important window through which one could view how these parents prefer their children to be perceived by society at large, according to the identities, roles, values, hierarchies or expectations constructed within a social space. Goodenough explains this culturally driven context of names and naming practices: Department of Chinese Studies, National University of Singapore The Shaw Foundation Building, Block AS7, Level 5 5 Arts Link, Singapore 117570 e-mail: [email protected] 102 Lee Cher Leng Ethnography of Singapore Chinese Names: Race, Religion, and Representation Different naming and address customs necessarily select different things about the self for communication and consequent emphasis. -
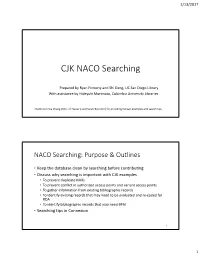
CJK NACO Searching
1/13/2017 CJK NACO Searching Prepared by Ryan Finnerty and Shi Deng, UC San Diego Library With assistance by Hideyuki Morimoto, Columbia University Libraries Thanks to Erica Chang (Univ. of Hawai’i) and Sarah Byun (LC) for providing Korean examples and search tips. NACO Searching: Purpose & Outlines • Keep the database clean by searching before contributing • Discuss why searching is important with CJK examples • To prevent duplicate NARs • To prevent conflict in authorized access points and variant access points • To gather information from existing bibliographic records • To identify existing records that may need to be evaluated and re‐coded for RDA • To identify bibliographic records that may need BFM • Searching tips in Connexion 2 1 1/13/2017 Why Search? To Prevent Duplicate NARs • Duplicates are normally created by inefficient searching and the 24‐ hour upload gap in the Name authority file. • Before creating a name authority record: 1. Search the OCLC authority file for the authorized access point, including variant forms of the access point. 2. In addition, search WorldCat for bibliographic records that contain the authorized access point or variant forms. • If you put your record in a save file, remember to search again if more than 24 hours have passed. • If you encounter duplicate records in the authority file, be sure to notify your NACO Coordinator so the records can be reported to LC. 3 Duplicate NARs for Personal Names (1) • 24 hours rule: If you put your record in a save file, remember to search again if more than 24 hours have passed. Entered: May 16, 2016 Entered: May 10, 2016 010 no2016066120 010 n 2016025569 046 ǂf 1983 ǂ2 edtf 046 ǂf 1983 ǂ2 edtf 1001 Tanaka, Yūsuke, ǂd 1983‐ 1001 Tanaka, Yūsuke, ǂd 1983‐ 4001 田中祐輔, ǂd 1983‐ 4001 田中祐輔, ǂd 1983‐ 670 Gendai Chūgoku no Nihongo kyōikushi, 2015: 670 Gendai Chūgoku no Nihongo kyōikushi, 2015: ǂbt.p.