NHS Lothian Board Meeting 01 April 2015.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -
Frommer's Scotland 8Th Edition
Scotland 8th Edition by Darwin Porter & Danforth Prince Here’s what the critics say about Frommer’s: “Amazingly easy to use. Very portable, very complete.” —Booklist “Detailed, accurate, and easy-to-read information for all price ranges.” —Glamour Magazine “Hotel information is close to encyclopedic.” —Des Moines Sunday Register “Frommer’s Guides have a way of giving you a real feel for a place.” —Knight Ridder Newspapers About the Authors Darwin Porter has covered Scotland since the beginning of his travel-writing career as author of Frommer’s England & Scotland. Since 1982, he has been joined in his efforts by Danforth Prince, formerly of the Paris Bureau of the New York Times. Together, they’ve written numerous best-selling Frommer’s guides—notably to England, France, and Italy. Published by: Wiley Publishing, Inc. 111 River St. Hoboken, NJ 07030-5744 Copyright © 2004 Wiley Publishing, Inc., Hoboken, New Jersey. All rights reserved. No part of this publication may be reproduced, stored in a retrieval sys- tem or transmitted in any form or by any means, electronic, mechanical, photo- copying, recording, scanning or otherwise, except as permitted under Sections 107 or 108 of the 1976 United States Copyright Act, without either the prior written permission of the Publisher, or authorization through payment of the appropriate per-copy fee to the Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923, 978/750-8400, fax 978/646-8600. Requests to the Publisher for per- mission should be addressed to the Legal Department, Wiley Publishing, Inc., 10475 Crosspoint Blvd., Indianapolis, IN 46256, 317/572-3447, fax 317/572-4447, E-Mail: [email protected]. -

28415 NDR Credits
28415 NDR Credits Billing Primary Liable party name Full Property Address Primary Liable Party Contact Add Outstanding Debt Period British Airways Plc - (5), Edinburgh Airport, Edinburgh, EH12 9DN Cbre Ltd, Henrietta House, Henrietta Place, London, W1G 0NB 2019 -5,292.00 Building 320, (54), Edinburgh Airport, Edinburgh, Building 319, World Cargo Centre, Manchester Airport, Manchester, Alpha Lsg Ltd 2017 -18,696.00 EH12 9DN M90 5EX Building 320, (54), Edinburgh Airport, Edinburgh, Building 319, World Cargo Centre, Manchester Airport, Manchester, Alpha Lsg Ltd 2018 -19,228.00 EH12 9DN M90 5EX Building 320, (54), Edinburgh Airport, Edinburgh, Building 319, World Cargo Centre, Manchester Airport, Manchester, Alpha Lsg Ltd 2019 -19,608.00 EH12 9DN M90 5EX The Maitland Social Club Per The 70a, Main Street, Kirkliston, EH29 9AB 70 Main Street, Kirkliston, West Lothian, EH29 9AB 2003 -9.00 Secretary/Treasurer 30, Old Liston Road, Newbridge, Midlothian, EH28 The Royal Bank Of Scotland Plc C/O Gva , Po Box 6079, Wolverhampton, WV1 9RA 2019 -519.00 8SS 194a, Lanark Road West, Currie, Midlothian, Martin Bone Associates Ltd (194a) Lanark Road West, Currie, Midlothian, EH14 5NX 2003 -25.20 EH14 5NX C/O Cbre - Corporate Outsourcing, 55 Temple Row, Birmingham, Lloyds Banking Group 564, Queensferry Road, Edinburgh, EH4 6AT 2019 -2,721.60 B2 5LS Unit 3, 38c, West Shore Road, Edinburgh, EH5 House Of Fraser (Stores) Ltd Granite House, 31 Stockwell Street, Glasgow, G1 4RZ 2008 -354.00 1QD Tsb Bank Plc 210, Boswall Parkway, Edinburgh, EH5 2LX C/O Cbre, 55 Temple -

Scottish Health Service Costs
Scottish Health Service Costs Year ended 31st March, 2001 i Blank Page SCOTTISH HEALTH SERVICE COSTS 2000/01 FOREWORD Introduction Scottish Health Service Costs provides financial and related activity information in sets of published tables. Most of the information relates to individual hospitals. An analysis of healthcare commissioned, practitioner services costs and community services costs is also included for each health board area. Divisional costs and Ambulance Service costs are included for the Common Services Agency. Costs of the Scottish Breast Screening Programme are included for each administrative area. The information may be used by managers at all levels as an aid to decision making, planning and control. It also provides a set of indicators of performance for comparison purposes. The Costs Book information may identify some problems and highlight questions to be asked: however, it will not provide answers by itself. These can only be found by looking at more detailed information in, for example, local information systems and also by considering the particular circumstances which pertain at the location. Source of Information The information contained in this publication is derived mainly from the financial and statistical information prepared as part of the annual accounts cycle of the Scottish Health Service and is unaudited. The annual accounts of health boards for 1992/93 were completely revised to bring them more closely into line with standard commercial accounts. Further minor changes have been made subsequently. The annual accounts of health boards and Scottish Financial Returns (SFRs) are prepared using common accounting principles as described in the Scottish Accounting Manual. The annual accounts of NHS trusts are prepared in accordance with the NHS Trusts Manual for Accounts. -

Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12
BOARD MEETING DATE: WEDNESDAY 4 FEBRUARY 2015 TIME: 9:30 A.M. - 12:00 P.M. VENUE: BOARDROOM, WAVERLEY GATE, 2-4 WATERLOO PLACE, EDINBURGH EH1 3EG Members are reminded that they should declare any financial and non-financial interests they have in the items of business for consideration, identifying the relevant agenda item and the nature of their interest. It is also a member’s duty under the Code of Conduct to ensure that any changes in circumstances are reported to the Corporate Services Manager within one month of them changing. AGENDA Agenda Lead Item Member Welcome to Members of the Public and the Press Apologies for Absence 1. Items for Approval 1.1. Minutes of the Board Meeting held on 3 December 2014 BH * 1.2. Minutes of the Special Board Meeting held on 14 January 2015 BH * 1.3. Running Action Note BH * 1.4. Performance Management AMcM * 1.5. Corporate Risk Register DF * 1.6. Committee Memberships BH * 1.7. Audit & Risk Committee - Minutes of 8 December 2014 JB * 1.8. Healthcare Governance Committee - Minutes of 25 November 2014 MB * 1.9. Finance & Resources Committee - Minutes of 12 November 2014 GW * 1.10. Strategic Planning Committee - Minutes of 13 November & 11 BH * December 2014 1.11. East Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12. Edinburgh Health & Social Care Partnership Shadow Board - RH * Minutes of 18 July 2014 1.13. Midlothian Health & Social Care Partnership Shadow Board Minutes PJ * of 23 October 2014 1.14. West Lothian Health & Care Partnership-Committee Sub - FT * Minutes of 18 December 2014 1.15. -

Public 143 MINUTE of MEETING of the EAST LIVINGSTON and EAST
DATA LABEL: Public 143 MINUTE of MEETING of the EAST LIVINGSTON AND EAST CALDER LOCAL AREA COMMITTEE of WEST LOTHIAN COUNCIL held within COUNCIL CHAMBERS, WEST LOTHIAN CIVIC CENTRE, on 1 SEPTEMBER 2016. Present – Councillors Frank Toner (Chair), Dave King, Frank Anderson and Carl John Apologies – Sandy Young, Almond Housing Association In Attendance – David Maule, Lead Officer WLC, Des Donnelly (SFRS), Sergeant Kris Linejs (Police Scotland), David Lees, Nets & Land Service WLC, Phyllis McFadyen, Housing WLC, Clare Stewart, Community Regeneration WLC, Ted Finch & Michelle Kirkbright, Parkrun and Suzie Young & Donna Paterson, Inveralmond Community High School. 1. ORDER OF BUSINESS The Chair ruled in terms of Standing Order 11 that Agenda Item 8 (Fire Services Performance Report) would be considered immediately following consideration of the Minute to facilitate attendance by fire service personnel. 2. DECLARATIONS OF INTEREST No declarations of interest were made. 3. MINUTE The committee confirmed the Minute of its meeting held on 16 June 2016. The Minute was thereafter signed by the Chair. 4. EAST LIVINGSTON & EAST CALDER MULTI-MEMBER WARD PERFORMANCE REPORT The committee considered a report (copies of which had been circulated) by the Scottish Fire and Rescue Service providing an update on the activity within the ward for the period up to 30 June 2016. Attached to the report at Appendix 1 was a summary report that provided a series of graphs showing details of accidental fire dwellings, deliberate fires, fires in non-domestic properties, non-fatal non-fire emergencies and unwanted fire alarm signals; each of the graphs demonstrated the statistics as they related to the whole of Scotland, the whole of West Lothian and for the ward. -
Certificate of Registration
CERTIFICATE OF REGISTRATION This is to certify that Walker Healthcare Limited - Central office Alderstone House MacMillan Road LIVINGSTON West Lothian EH54 7AW has been audited and found to meet the requirements of standard ISO 9001:2015 Quality Management System Scope of certification NHS Continuing Care Facility, Administration of Hotel Services, Estates & Facilities Management, Non-Clinical Services and the Interaction of same. Excluded from the Quality System are Clinical Services, Confidential Information and Related Therapies. Certificate number: 638 Karen Prendergast Sector Director - Certification Issue number: 2018-01 Exova BM TRADA Certificate start date: 3 December 2015 Exova (UK) Ltd, (T/A Exova BM TRADA), Chiltern House, Stocking Lane, High Wycombe, Buckinghamshire, HP14 4ND, UK Registered Office: Exova (UK) Ltd, Lochend Industrial Estate, Newbridge, Midlothian EH28 8PL United Kingdom. Reg No. SCO70429. Certificate expiry date: 2 December 2018 This certificate remains the property of Exova (UK) Ltd. This certificate and all copies or reproductions of the certificate shall be returned to Exova (UK) Ltd or destroyed if requested. Further clarification regarding the scope of this certificate and verification of the certificate is Date of initial certification: 31 March 1998 available through Exova BM TRADA or at the above address or at www.exovabmtrada.com The use of the UKAS accreditation mark indicates accreditation in respect of those activities covered by the accreditation certification 012 Multisite clients – The scope of certification shown above includes the participating sites shown in appendix A Appendix A The network of participating sites shown below is included in the scope of certification shown on certificate number (638) Branch Address Mearnskirk Road Newton Mearns Mearnskirk House Ltd Glasgow Scotland G77 5RZ Owens Farm Road Offerton The Meadows (Stockport) Ltd Stockport SK2 5EQ 100 Pilton Drive Edinburgh Ferryfield House Ltd Midlothian EH5 2HF Carnbee Avenue Edinburgh Ellen's Glen House Ltd Midlothian EH16 6FF . -
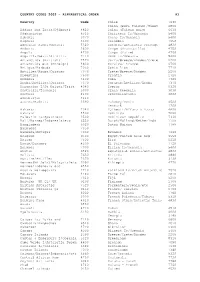
Country Codes 2002 – Alphabetical Order A1
COUNTRY CODES 2002 – ALPHABETICAL ORDER A1 Country Code Chile 7640 China (excl Taiwan)/Tibet 6800 Affars and Issas/Djibouti 4820 China (Taiwan only) 6630 Afghanistan 6510 Christmas Is/Oceania 5400 Albania 3070 Cocos Is/Oceania 5400 Algeria 3500 Colombia 7650 American Samoa/Oceania 5320 Comoros/Antarctic Foreign 4830 Andorra 2800 Congo (Brazzaville) 4750 Angola 4700 Congo (Zaire) 4760 Anguilla/Nevis/St Kitts 7110 Cook Is/Oceania 5400 Antarctica (British) 7520 Corfu/Greece/Rhodes/Crete 2200 Antarctica etc (Foreign) 4830 Corsica/ France 0700 Antigua/Barbuda 7030 Costa Rica 7710 Antilles/Aruba/Curacao 7370 Crete/Greece/Rhodes 2200 Argentina 7600 Croatia 2720 Armenia 3100 Cuba 7320 Aruba/Antilles/Curacao 7370 Curacao/Antilles/Aruba 7370 Ascension I/St Helena/Trist 4040 Cyprus 0320 Australia/Tasmania 5000 Czech Republic 3030 Austria 2100 Czechoslovakia 3020 Azerbaijan 3110 Azores/Madeira 2390 Dahomey/Benin 4500 Denmark 1200 Bahamas 7040 Djibouti/Affars & Issas 4820 Bahrain 5500 Dominica 7080 Balearic Is/Spain/etc 2500 Dominican Republic 7330 Bali/Borneo/Indonesia/etc 6550 Dutch/Holland/Netherlnds 1100 Bangladesh 6020 Dutch Guiana 7780 Barbados 7050 Barbuda/Antigua 7030 Ecuador 7660 Belgium 0500 Egypt/United Arab Rep 3550 Belize 7500 Eire 0210 Benin/Dahomey 4500 El Salvador 7720 Bermuda 7000 Ellice Is/Oceania 5400 Bhutan 6520 Equatorial Guinea/Antarctic 4830 Bolivia 7630 Eritrea 4840 Bonaire/Antilles 7370 Estonia 3130 Borneo(NE Soln)/Malaysia/etc 6050 Ethiopia 4770 Borneo/Indonesia etc 6550 Bosnia Herzegovina 2710 Falkland Is/Brtsh Antarctic -

Lothian's Palliative and End of Life Care Strategy for 2010
Living & Dying Well in Lothian Final Version - March 2010 Contents 1. EXECUTIVE SUMMARY .......................................................................................................... 3 2. DEFINITION OF PALLIATIVE CARE, TRAJECTORIES OF DYING, & POLICY CONTEXT ... 5 Definitions...........................................................................................................5 Trajectories of Dying...........................................................................................5 Policy context in Scotland...................................................................................6 3. BACKGROUND ........................................................................................................................ 8 Living and Dying in Lothian.................................................................................8 4. INTRODUCTION..................................................................................................................... 12 Challenges in palliative care, and new concepts and models...........................12 5. HOW THIS STRATEGY HAS BEEN DEVELOPED................................................................ 13 6. OUR VISION........................................................................................................................... 14 7. MODEL OF CARE .................................................................................................................. 15 8. WHAT WE HAVE ALREADY COMMITTED TO DO .............................................................. -

The Scottish Government Consolidated Accounts for the Year Ended 31 March 2018
The Scottish Government Consolidated Accounts for the year ended 31 March 2018 Laid before the Scottish Parliament By the Scottish Ministers 27 September 2018 SG/2018/160 Foreword As Chief Financial Officer for the Scottish Government, it is my responsibility to oversee the processes that produce the financial reporting by and for the Scottish Government. I lead a team of finance professionals who support Scottish Ministers in their financial decision-making to secure the regularity, propriety and value for money of the funds provided by taxpayers to deliver devolved government in Scotland. I am pleased to introduce these accounts, which are an important part of the reporting on the stewardship of the whole Scottish Budget approved by the Scottish Parliament. The accounts cover the bodies within the accounting boundary and present the financial outturn compared to the spending plans of Scottish Ministers for those elements for the financial year 2017-18 authorised by the Budget (Scotland) Act 2017 and are prepared in accordance with international accounting standards and related accounting guidance. I am pleased that the Auditor General’s opinion on these accounts is, once again, unqualified. It is important to note that these accounts are not a Ministerial document: it is the Principal Accountable Officer’s responsibility to produce accounts, and a primary purpose of these accounts is to report on the stewardship of the sums authorised. It is also important to recognise that these accounts are not the full picture of the fiscal activity of Scottish Ministers. Our financial reporting outputs are developing alongside the Scottish Government’s increasing fiscal responsibility and in tandem with the developments associated with the implementation of the Budget Process Review Group recommendations: • building on this account, a separate statement to Parliament brings together the Financial Outturn of the bodies within the Scottish Administration, to report against the statutory limit authorised by the Scottish Parliament in the Budget processes. -

Edinburgh's Joint Commissioning Plan for Older People 2012-22
‘Live Well in Later Life’ Edinburgh’s Joint Commissioning Plan for Older People 2012-22 In partnership with Foreword Older people use our health and social care services more than any other group of service users. We also know that the number of older people is growing faster than any other age group and their preferences and expectations are changing. In order to meet the needs of older people in Edinburgh, now and in the future, it is essential that we have robust plans in place. It is key that these plans are developed and delivered in partnership with all providers of health, social care and support for older people, whether these be in the NHS, Council, voluntary or independent sector. It is only by working together that we can deliver the best outcomes for older people within the challenging financial and demographic context that we face. This ten year plan sets out the strategic direction for older people’s services ranging from acute hospital care through to lower levels of support provided within the community. The plan covers a wide range of services and support and recognises the important contribution made to the health and wellbeing of older people living in Edinburgh. Within the lifetime of this plan, the health and social care landscape will change significantly. National policy changes including the Integration of Health and Social Care and the Personalisation of services (which includes the introduction of Self Directed Support legislation) will transform the way that care and support is delivered. We are working with our partners to deliver this transformational change, to give older people more choice and control over the care and support they receive and to ensure that health and social care services are of high quality, are joined up and are focused on individuals. -

2709-Mental Health Incidents
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 12/07/2018 Your Ref: Our Ref: 2709 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] Dear FREEDOM OF INFORMATION – MENTAL HEALTH INCIDENTS I write in response to your request for information in relation to mental health incidents within NHS Lothian. I have been provided with information to help answer your request by the Quality Improvement Team, Workforce Planning Department and Analytical Services Department of NHS Lothian. Question: 1. How often have physical restraints been used in health facilities in each of the past four years. I would like this information in the following format • NAME OF FACILITY YEAR 1 YEAR 2 YEAR 3 YEAR 3 Eg Central Hospital 10 5 9 14 Answer: 2014/15 2015/16 2016/18 2017/18 Civic Centre ≤5 ≤5 0 ≤5 Craigshill Care Facility 147 219 43 32 Ellen's Glen House 0 0 ≤5 0 Herdmanflat Hospital 50 10 ≤5 ≤5 Midlothian Community Hospital 65 62 39 60 St Johns 101 149 123 166 Tippethill House 6 7 ≤5 ≤5 CAMHS 205 114 76 137 Findlay House 0 ≤5 13 0 FME Service 0 0 0 ≤5 Orchard Clinic 78 81 112 101 Royal Edinburgh Hospital 546 649 700 563 Royal Infirmary Little France ≤5 ≤5 0 0 The Esk Centre 0 0 ≤5 0 Mental health incidents - July 2018 Cambridge Street House ≤5 0 ≤5 ≤5 Craigroyston Health Clinic 0 0 ≤5 0 Ellen's Glen House 21 22 67 33 Ferryfield House ≤5 15 17 34 Findlay House 9 57 208 113 Total 1,235 1,390 1,410 1,249 Question: 2.