Lothian's Palliative and End of Life Care Strategy for 2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Payments Over £25K January 2019
NHS LOTHIAN January PAYMENTS OVER £25,000 Payments through Accounts Payable Payee Name Date Paid Amount Description of Expenditure Evoc 07/01/2019 170,625.00 community link workers April,july,Oct and Jan 19 Direct Debit-workman Llp Gpg No1 Scotland 10/01/2019 121,562.50 Qtr 4 Rent costs for Strathbrock Partnership Centre National Procurement Nhs Scotland 04/01/2019 2,096,023.35 NATIONAL DISTRIBUTION COSTS Fife Nhs Board 04/01/2019 53,737.00 Service Level Agreement - Monthly Payment Nhs Forth Valley 04/01/2019 100,913.00 Service Level Agreement - Monthly Payment Nhs Highland 04/01/2019 27,801.00 Service Level Agreement - Monthly Payment Nhs Lanarkshire 04/01/2019 81,473.00 Service Level Agreement - Monthly Payment Nhs Greater Glasgow And Clyde 04/01/2019 48,687.00 Service Level Agreement - Exclusions to contract Tayside Nhs Board 04/01/2019 54,780.00 Service Level Agreement - Monthly Payment Nhs National Services Scotland 04/01/2019 44,363.42 Immunology testing Oct 18 Fife Nhs Board 04/01/2019 176,228.00 Endoscopy unit Oct -Dec 18 Csl Behring Uk Ltd 04/01/2019 29,800.00 DRUGS R P Slight And Sons Ltd 16/01/2019 41,668.40 Fit fire door sets - St Johns Hospital Adt Fire And Security Plc 11/01/2019 45,595.00 materials Consort Healthcare 04/01/2019 1,187,185.69 Advanced Billing Apr-June 19 Consort Healthcare 04/01/2019 127,500.00 Advanced Billing Apr-June 19 Rmf Health Limited 25/01/2019 32,747.10 payment certificate no7 western general renal Rmf Health Limited 09/01/2019 47,695.32 payment certificate no6 western general oncology Rmf Health -

LHB1/62-112A
LHB 1 ROYAL INFIRMARY OF EDINBURGH 62 Annual Statistics of Patients, 1854-1864 Bound volumes giving an annual analysis of cases treated at the Infirmary. The first table gives the types of categories to be considered, with the total number of male and female patients treated for each category of disease; also numbers of cures and of deaths. Subsequent tables examine the separate categories in more detail, giving breakdowns of numbers according to such factors as age, month of the year, etc. Individual categories include fevers, nervous diseases, diseases of the respiratory system, and different types of operation. Manuscript. 1 1854–1855 Compiled by Robert Brown, Surgeon, 1856. 2 wanting 3 1856–1857 Compiled by James Welsh, Surgeon, Madras Army. 4 [1857–1858] Compiled by L Thomson Welsh. 5 1858–1859 Compiled by L Thomson Welsh. 6 1859–1860 Compiled by L Thomson Welsh. 7 1860–1861 Compiled by L Thomson Welsh. 8 1861–1862 Compiled by J Douglas Watson 9 1862–1863 Compiled by J Douglas Watson 10 1863–1864 Compiled by J Douglas Watson LHB 1 ROYAL INFIRMARY OF EDINBURGH 63 Registers of Beds and Patients, 1877-1965 Bound ledgers of weekly returns. The week’s page is divided into surgical wards and medical wards. The physician or surgeon in charge of each ward is given, along with the number of patients in that ward. At the foot of the page is a summary of the number of patients, and results of treatment in that week. 1 Mar 1877–Feb 1879 Returns for Mar 1879 have been stuck in, interleaved with entries for 31 Mar – 5 May 1877. -

LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothia
LHB37 LOTHIAN HEALTH BOARD Introduction 1 Agenda of Meetings of Lothian Health Board, 1987-1995 2 Agenda of Meetings of Lothian Health Board Committees, 1987-1989 2A Minutes of Board, Standing Committees and Sub-Committees, 1973-1986 2B Draft Minutes of Board Meetings, 1991-2001 2C [not used] 2D Area Executive Group Minutes, 1973-1986 2E Area Executive Group Agendas and Papers, 1978-1985 2F Agenda Papers for Contracts Directorate Business Meetings, 1993-1994 2G Agenda Papers of Finance, Manpower and Establishment Committee, 1975-1979 2H Agenda papers of the Policy and Commissioning Team Finance and Corporate Services Sub- Group, 1994-1995 2I [not used] 2J Minutes and Papers of the Research Ethics Sub-Committees, 1993-1995 3 Annual Reports, 1975-2004 4 Annual Reports of Director of Public Health, 1989-2008 5 Year Books, 1977-1992 6 Internal Policy Documents and Reports, 1975-2005 7 Publications, 1960-2002 8 Administrative Papers, 1973-1994 8A Numbered Administrative Files, 1968-1993 8B Numbered Registry Files, 1970-1996 8C Unregistered Files, 1971-1997 8D Files of the Health Emergency Planning Officer, 1978-1993 9 Annual Financial Reviews, 1974-1987 10 Annual Accounts, 1976-1992 10A Requests for a major item of equipment, 1987-1990 LHB37 LOTHIAN HEALTH BOARD 11 Lothian Medical Audit Committee, 1988-1997 12 Records of the Finance Department, 1976-1997 13 Endowment Fund Accounts, 1972-2004 14 Statistical Papers, 1974-1990 15 Scottish Health Service Costs, 1975-1987 16 Focus on Health , 1982-1986 17 Lothian Health News , 1973-2001 18 Press -

Scottish Health Service Costs
Scottish Health Service Costs Year ended 31st March, 2001 i Blank Page SCOTTISH HEALTH SERVICE COSTS 2000/01 FOREWORD Introduction Scottish Health Service Costs provides financial and related activity information in sets of published tables. Most of the information relates to individual hospitals. An analysis of healthcare commissioned, practitioner services costs and community services costs is also included for each health board area. Divisional costs and Ambulance Service costs are included for the Common Services Agency. Costs of the Scottish Breast Screening Programme are included for each administrative area. The information may be used by managers at all levels as an aid to decision making, planning and control. It also provides a set of indicators of performance for comparison purposes. The Costs Book information may identify some problems and highlight questions to be asked: however, it will not provide answers by itself. These can only be found by looking at more detailed information in, for example, local information systems and also by considering the particular circumstances which pertain at the location. Source of Information The information contained in this publication is derived mainly from the financial and statistical information prepared as part of the annual accounts cycle of the Scottish Health Service and is unaudited. The annual accounts of health boards for 1992/93 were completely revised to bring them more closely into line with standard commercial accounts. Further minor changes have been made subsequently. The annual accounts of health boards and Scottish Financial Returns (SFRs) are prepared using common accounting principles as described in the Scottish Accounting Manual. The annual accounts of NHS trusts are prepared in accordance with the NHS Trusts Manual for Accounts. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12
BOARD MEETING DATE: WEDNESDAY 4 FEBRUARY 2015 TIME: 9:30 A.M. - 12:00 P.M. VENUE: BOARDROOM, WAVERLEY GATE, 2-4 WATERLOO PLACE, EDINBURGH EH1 3EG Members are reminded that they should declare any financial and non-financial interests they have in the items of business for consideration, identifying the relevant agenda item and the nature of their interest. It is also a member’s duty under the Code of Conduct to ensure that any changes in circumstances are reported to the Corporate Services Manager within one month of them changing. AGENDA Agenda Lead Item Member Welcome to Members of the Public and the Press Apologies for Absence 1. Items for Approval 1.1. Minutes of the Board Meeting held on 3 December 2014 BH * 1.2. Minutes of the Special Board Meeting held on 14 January 2015 BH * 1.3. Running Action Note BH * 1.4. Performance Management AMcM * 1.5. Corporate Risk Register DF * 1.6. Committee Memberships BH * 1.7. Audit & Risk Committee - Minutes of 8 December 2014 JB * 1.8. Healthcare Governance Committee - Minutes of 25 November 2014 MB * 1.9. Finance & Resources Committee - Minutes of 12 November 2014 GW * 1.10. Strategic Planning Committee - Minutes of 13 November & 11 BH * December 2014 1.11. East Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12. Edinburgh Health & Social Care Partnership Shadow Board - RH * Minutes of 18 July 2014 1.13. Midlothian Health & Social Care Partnership Shadow Board Minutes PJ * of 23 October 2014 1.14. West Lothian Health & Care Partnership-Committee Sub - FT * Minutes of 18 December 2014 1.15. -
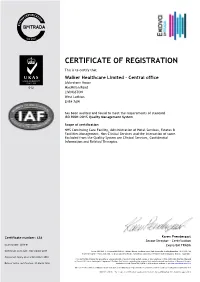
Certificate of Registration
CERTIFICATE OF REGISTRATION This is to certify that Walker Healthcare Limited - Central office Alderstone House MacMillan Road LIVINGSTON West Lothian EH54 7AW has been audited and found to meet the requirements of standard ISO 9001:2015 Quality Management System Scope of certification NHS Continuing Care Facility, Administration of Hotel Services, Estates & Facilities Management, Non-Clinical Services and the Interaction of same. Excluded from the Quality System are Clinical Services, Confidential Information and Related Therapies. Certificate number: 638 Karen Prendergast Sector Director - Certification Issue number: 2018-01 Exova BM TRADA Certificate start date: 3 December 2015 Exova (UK) Ltd, (T/A Exova BM TRADA), Chiltern House, Stocking Lane, High Wycombe, Buckinghamshire, HP14 4ND, UK Registered Office: Exova (UK) Ltd, Lochend Industrial Estate, Newbridge, Midlothian EH28 8PL United Kingdom. Reg No. SCO70429. Certificate expiry date: 2 December 2018 This certificate remains the property of Exova (UK) Ltd. This certificate and all copies or reproductions of the certificate shall be returned to Exova (UK) Ltd or destroyed if requested. Further clarification regarding the scope of this certificate and verification of the certificate is Date of initial certification: 31 March 1998 available through Exova BM TRADA or at the above address or at www.exovabmtrada.com The use of the UKAS accreditation mark indicates accreditation in respect of those activities covered by the accreditation certification 012 Multisite clients – The scope of certification shown above includes the participating sites shown in appendix A Appendix A The network of participating sites shown below is included in the scope of certification shown on certificate number (638) Branch Address Mearnskirk Road Newton Mearns Mearnskirk House Ltd Glasgow Scotland G77 5RZ Owens Farm Road Offerton The Meadows (Stockport) Ltd Stockport SK2 5EQ 100 Pilton Drive Edinburgh Ferryfield House Ltd Midlothian EH5 2HF Carnbee Avenue Edinburgh Ellen's Glen House Ltd Midlothian EH16 6FF . -

NHS Lothian Board Meeting 01 April 2015.Pdf
BOARD MEETING DATE: WEDNESDAY 1 APRIL 2015 TIME: 9:30 A.M. - 12:00 P.M. VENUE: BOARDROOM, WAVERLEY GATE, 2-4 WATERLOO PLACE, EDINBURGH EH1 3EG Members are reminded that they should declare any financial and non-financial interests they have in the items of business for consideration, identifying the relevant agenda item and the nature of their interest. It is also a member’s duty under the Code of Conduct to ensure that any changes in circumstances are reported to the Corporate Services Manager within one month of them changing. AGENDA Agenda Lead Item Member Welcome to Members of the Public and the Press Apologies for Absence 1. Items for Approval 1.1. Minutes of the Board Meeting held on 4 February 2015 BH * 1.2. Minutes of the Special Board Meeting held on 4 March 2015 BH * 1.3. Running Action Note BH * 1.4. Performance Management AMcM * 1.5. Royal Bank of Scotland Bulk Cash Service SG * 1.6. Strategic Planning Committee Revised Remit and Membership AMcM * 1.7. Corporate Risk Register DF * 1.8. Healthcare Associated Infection Update MJ * 1.9. Unscheduled Care MJ * 1.10. Edinburgh Partnership Community Plan 2015-18 AMcM * 1.11. Committee Chairs and Memberships BH * 1.12. Audit & Risk Committee - Minutes of 19 February 2015 JMcD * 1.13. Healthcare Governance Committee - Minutes of 21 January 2015 MB * 1.14. Finance & Resources Committee - Minutes of 21 January 2015 GW * 1.15. Strategic Planning Committee - Minutes of 15 January & 12 BH * February 2015 1.16. East Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 22 January 2015 1.17. -

The Scottish Government Consolidated Accounts for the Year Ended 31 March 2018
The Scottish Government Consolidated Accounts for the year ended 31 March 2018 Laid before the Scottish Parliament By the Scottish Ministers 27 September 2018 SG/2018/160 Foreword As Chief Financial Officer for the Scottish Government, it is my responsibility to oversee the processes that produce the financial reporting by and for the Scottish Government. I lead a team of finance professionals who support Scottish Ministers in their financial decision-making to secure the regularity, propriety and value for money of the funds provided by taxpayers to deliver devolved government in Scotland. I am pleased to introduce these accounts, which are an important part of the reporting on the stewardship of the whole Scottish Budget approved by the Scottish Parliament. The accounts cover the bodies within the accounting boundary and present the financial outturn compared to the spending plans of Scottish Ministers for those elements for the financial year 2017-18 authorised by the Budget (Scotland) Act 2017 and are prepared in accordance with international accounting standards and related accounting guidance. I am pleased that the Auditor General’s opinion on these accounts is, once again, unqualified. It is important to note that these accounts are not a Ministerial document: it is the Principal Accountable Officer’s responsibility to produce accounts, and a primary purpose of these accounts is to report on the stewardship of the sums authorised. It is also important to recognise that these accounts are not the full picture of the fiscal activity of Scottish Ministers. Our financial reporting outputs are developing alongside the Scottish Government’s increasing fiscal responsibility and in tandem with the developments associated with the implementation of the Budget Process Review Group recommendations: • building on this account, a separate statement to Parliament brings together the Financial Outturn of the bodies within the Scottish Administration, to report against the statutory limit authorised by the Scottish Parliament in the Budget processes. -

Edinburgh's Joint Commissioning Plan for Older People 2012-22
‘Live Well in Later Life’ Edinburgh’s Joint Commissioning Plan for Older People 2012-22 In partnership with Foreword Older people use our health and social care services more than any other group of service users. We also know that the number of older people is growing faster than any other age group and their preferences and expectations are changing. In order to meet the needs of older people in Edinburgh, now and in the future, it is essential that we have robust plans in place. It is key that these plans are developed and delivered in partnership with all providers of health, social care and support for older people, whether these be in the NHS, Council, voluntary or independent sector. It is only by working together that we can deliver the best outcomes for older people within the challenging financial and demographic context that we face. This ten year plan sets out the strategic direction for older people’s services ranging from acute hospital care through to lower levels of support provided within the community. The plan covers a wide range of services and support and recognises the important contribution made to the health and wellbeing of older people living in Edinburgh. Within the lifetime of this plan, the health and social care landscape will change significantly. National policy changes including the Integration of Health and Social Care and the Personalisation of services (which includes the introduction of Self Directed Support legislation) will transform the way that care and support is delivered. We are working with our partners to deliver this transformational change, to give older people more choice and control over the care and support they receive and to ensure that health and social care services are of high quality, are joined up and are focused on individuals. -

2709-Mental Health Incidents
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 12/07/2018 Your Ref: Our Ref: 2709 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] Dear FREEDOM OF INFORMATION – MENTAL HEALTH INCIDENTS I write in response to your request for information in relation to mental health incidents within NHS Lothian. I have been provided with information to help answer your request by the Quality Improvement Team, Workforce Planning Department and Analytical Services Department of NHS Lothian. Question: 1. How often have physical restraints been used in health facilities in each of the past four years. I would like this information in the following format • NAME OF FACILITY YEAR 1 YEAR 2 YEAR 3 YEAR 3 Eg Central Hospital 10 5 9 14 Answer: 2014/15 2015/16 2016/18 2017/18 Civic Centre ≤5 ≤5 0 ≤5 Craigshill Care Facility 147 219 43 32 Ellen's Glen House 0 0 ≤5 0 Herdmanflat Hospital 50 10 ≤5 ≤5 Midlothian Community Hospital 65 62 39 60 St Johns 101 149 123 166 Tippethill House 6 7 ≤5 ≤5 CAMHS 205 114 76 137 Findlay House 0 ≤5 13 0 FME Service 0 0 0 ≤5 Orchard Clinic 78 81 112 101 Royal Edinburgh Hospital 546 649 700 563 Royal Infirmary Little France ≤5 ≤5 0 0 The Esk Centre 0 0 ≤5 0 Mental health incidents - July 2018 Cambridge Street House ≤5 0 ≤5 ≤5 Craigroyston Health Clinic 0 0 ≤5 0 Ellen's Glen House 21 22 67 33 Ferryfield House ≤5 15 17 34 Findlay House 9 57 208 113 Total 1,235 1,390 1,410 1,249 Question: 2.