Burundi Country Operational Plan (COP) 2019 Strategic Direction Summary 29 April 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Business Ethics As Field of Training, Teaching and Research in Francophone Africa
Faculty of Arts and Humanities, Original Business Ethics as field of training, teaching and Article research in Francophone Africa Liboire Kagabo Department of African Languages and Literature, University of Burundi, Burundi ABSTRACT This article has been written within the framework of the Global Survey of Business Ethics 2010. It is seemingly the first attempt to investigate Business Ethics as academic field in Francophone Africa. After a discussion of methodological considerations, the article provides an overview of how Business Ethics is distributed in Francophone Africa. Even though, it is not well established in that part of Africa, some interesting data have been found in some countries like Burundi, Democratic Republic of Congo, Ivory Coast, Rwanda and Senegal. Business Ethics has been investigated in three areas: teaching, training and research. In Francophone Africa, teaching Business Ethics does not seem to be a reality in traditional faculties of Economics, Management or Commerce. Training in Business Ethics, however, is a reality in Francophone Africa, notably with the non-governmental organizations that deal with political and economic governance, development, and women and gender issues. Research on Business Ethics can be found in journals, bulletins, consultancy reports, university term papers, seminars and colloquia as well as in books. Key words: Business Ethics, Teaching, Training, Research, Francophone Africa INTRODUCTION Madagascar. For the purpose of the survey some French speaking countries in West For the purpose of the Global Survey of Africa, namely Cameroun, Tchad, Niger, Business Ethics 2010, the world was divided Benin and Togo was however included in into nine world regions, one of which was the the West African region. -

Burundi-SCD-Final-06212018.Pdf
Document of The World Bank Report No. 122549-BI Public Disclosure Authorized REPUBLIC OF BURUNDI ADDRESSING FRAGILITY AND DEMOGRAPHIC CHALLENGES TO REDUCE POVERTY AND BOOST SUSTAINABLE GROWTH Public Disclosure Authorized SYSTEMATIC COUNTRY DIAGNOSTIC June 15, 2018 Public Disclosure Authorized International Development Association Country Department AFCW3 Africa Region International Finance Corporation (IFC) Sub-Saharan Africa Department Multilateral Investment Guarantee Agency (MIGA) Sub-Saharan Africa Department Public Disclosure Authorized BURUNDI - GOVERNMENT FISCAL YEAR January 1 – December 31 CURRENCY EQUIVALENTS (Exchange Rate Effective as of December 2016) Currency Unit = Burundi Franc (BIF) US$1.00 = BIF 1,677 ABBREVIATIONS AND ACRONYMS ACLED Armed Conflict Location and Event Data Project AfDB African Development Bank BMM Burundi Musangati Mining CE Cereal Equivalent CFSVA Comprehensive Food Security and Vulnerability Assessment CNDD-FDD Conseil National Pour la Défense de la Démocratie-Forces pour la Défense de la Démocratie (National Council for the Defense of Democracy-Forces for the Defense of Democracy) CPI Consumer Price Index CPIA Country Policy and Institutional Assessment DHS Demographic and Health Survey EAC East African Community ECVMB Enquête sur les Conditions de Vie des Menages au Burundi (Survey on Household Living Conditions in Burundi) ENAB Enquête Nationale Agricole du Burundi (National Agricultural Survey of Burundi) FCS Fragile and conflict-affected situations FDI Foreign Direct Investment FNL Forces Nationales -

HIV DR in CENTRAL AFRICA
WHO HIVRESNET STEERING COMMITTEE MEETING, November 10–12, 2009, Geneva, Switzerland HIV DR in CENTRAL AFRICA Pr Belabbes Intercountry Support Team Central Africa COUNTRIES COVERED BY THE INTERCOUNTRY SUPPORT TEAM / CENTRAL AFRICA Angola Burundi Cameroon Central African Republic Chad Congo Democratic Republic of Congo Equatorial Guinea Gabon Rwanda Sao Tome & Principe HIV PREVALENCE AMONG THE POPULATION Legend Generalized epidemic in 10 <1% countries /11 1-5% >5% Excepted Sao Tome& Principe nd HIV PREVALENCE AMONG PREGNANT WOMEN Legend <1% 1-5% >5% nd PATIENTS UNDER ART 2005-2008 70000 2005 2006 2007 2008 60000 50000 40000 30000 20000 10000 0 Angola Burundi Cameroon Congo Equatorial Gabon CAR DRC Rwanda Sao Tome Guinea Source of data Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. WHO, UNAIDS,UNICEF;September 2009. Training on HIVDR Protocols ANGOLA BURUNDI CAMEROON CENTRAL AFRICA REPUBLIC CHAD CONGO DEMOCRATIC REPUBLIC CONGO EQUATORIAL GUINEA GABON RWANDA SAO TOME&PRINCIPE Training on HIVDR Protocols Douala, Cameroon 27-29 April 2009 The opening ceremony Participants to the Training on HIVDR Protocols, Douala Cameroon 27-29 April 2009 ON SITE STRENGTHENING CAPACITIES OF THE TECHNICAL WORKING GROUPS ANGOLA BURUNDI CAMEROON CENTRAL AFRICA REPUBLIC CHAD EQUATORIAL GUINEA RWANDA TECHNICAL ASSISTANCE PROVIDED TO DEVELOP HIVDR PROTOCOLS ANGOLA BURUNDI CAMEROON CENTRAL AFRICA REPUBLIC CHAD EQUATORIAL GUINEA RWANDA EARLY WARNING INDICATORS BURUNDI : EWI abstraction in 19 sites (October) using paper-based. -

Researching Education Outcomes in Burundi, Malawi, Senegal and Uganda: Using Participatory Tools and Collaborative Approaches
Researching education outcomes in Burundi, Malawi, Senegal and Uganda: using participatory tools and collaborative approaches Dr. Karen Edge Akanksha A. Marphatia Elise Legault David Archer The Improving Learning Outcomes in Primary Schools (ILOPS) Project | Project methodology Funding: The William and Flora Hewlett Foundation in partnership with the Bill & Melinda Gates Foundation May 2010 © Institute of Education and ActionAid Table of Contents Section Page Executive summary 6 Context 8 Section 1 Current knowledge 11 Current knowledge on participatory approaches involving stakeholders to address children's learning 11 Implications of literature review on the ILOPS collaborative approach 11 Section 2 Building ILOPS partnerships 12 Recruiting the international, national and local researchers 12 The constituencies involved in multi-stakeholder research teams 13 Strategies for coordinating national-level team involvement 15 Section 3 Designing the ILOPS research framework 17 Pre-workshop activities and agenda setting 17 Workshop 1 – the Sesse cross-country research design workshop 18 Mapping expertise: what makes a good research team? 20 Developing the ILOPS conceptual framework 22 Focusing the ILOPS research 23 Generating and testing interview instruments 24 Next steps 25 Section 4 In-country data collection, analysis and validation process 26 Research process 26 In-country data analysis and validation workshops 27 Section 5 Cross-country findings 28 Workshop 2: Discussing cross-country findings 28 Section 6 Lessons learned on collaborative -
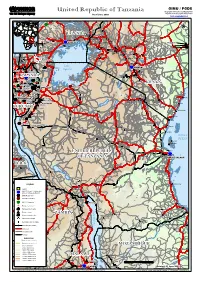
United Republic of Tanzania Geographic Information and Mapping Unit Population and Geographic Data Section As of June 2003 Email : [email protected]
GIMU / PGDS United Republic of Tanzania Geographic Information and Mapping Unit Population and Geographic Data Section As of June 2003 Email : [email protected] Soroti Masindi ))) ))) Bunia ))) HoimaHoima CCCCC CCOpiOpi !!! !! !!! !! !!! !! Mbale 55 !! 5555 55 Kitale !! 5555 Fort Portal UGANDAUGANDA !! CC !! Tororo !! ))) ))) !! ))) Bungoma !! !! Jinja CCCCCSwesweSweswe ))) Isiolo Tanzania_Atlas_A3PC.WOR CC ))) CC ))) KAMPALAKAMPALA ))) Kakamega DagahaleyDagahaley ))) Butembo !! ))) !! Entebbe Kisumu ))) Thomsons Falls!! Nanyuki IfoIfoIfo KakoniKakoni ))) !! ))) ))) ))) HagaderaHagadera ))) Lubero Londiani ))) DadaabDadaab Kabatoro ))) Molo ))) !! Nakuru ))) Bingi Elburgon !! Nyeri Gilgil ))) !! Embu CC))) MbararaMbarara Kinyasano CCMbararaMbarara !! Kisii ))) Naivasha ))) Fort Hall ))) )))) Nyakibale CCSettlementSettlement ))) CCCKifunzoKifunzo Makiro ))) Rutshuru ))) Thika ))) Kabale ))) ))) Lake ))) ))) Bukoba NAIROBINAIROBI Kikungiri Victoria ))) ))) ))) ))) MwisaMwisa Athi River !! GisenyiGisenyi ))) MwisaMwisa !! ))) ByumbaByumba Machakos yy!!))) Goma ))) Kajiado RWANDARWANDA ))) RWANDARWANDA ))) RWANDARWANDA ))) RWANDARWANDA ))) RWANDARWANDA ))) RWANDARWANDA ))) RWANDARWANDA Magadi ))) KIGALIKIGALI KibuyeKibuye ))) KibungoKibungo ))) KibungoKibungo KENYAKENYA ))) KENYAKENYA ))) KENYAKENYA ))) KENYAKENYA ))) KENYAKENYA ))) GikongoroGikongoro NgaraNgara))) ))) NgaraNgara ))) !! ))) LukoleLukole A&BA&B MwanzaMwanza !! )))LukoleLukole A&BA&B MuganoMugano ))) )))MbubaMbuba SongoreSongore ))) ))) Ngozi ))) MuyingaMuyinga ))) Nyaruonga -

Transaction Costs and Smallholder Farmers' Participation in Banana
Center of Evaluation for Global Action Working Paper Series Agriculture for Development Paper No. AfD-0909 Issued in July 2009 Transaction Costs and Smallholder Farmers’ Participation in Banana Markets in the Great Lakes Region John Jagwe Emily Ouma Charles Machethe University of Pretoria International Institute of Tropical Agriculture This paper is posted at the eScholarship Repository, University of California. http://repositories.cdlib.org/cega/afd Copyright © 2009 by the author(s). Series Description: The CEGA AfD Working Paper series contains papers presented at the May 2009 Conference on “Agriculture for Development in Sub-Saharan Africa,” sponsored jointly by the African Economic Research Consortium (AERC) and CEGA. Recommended Citation: Jagwe, John; Ouma, Emily; Machethe, Charles. (2009) Transaction Costs and Smallholder Farmers’ Participation in Banana Markets in the Great Lakes Region. CEGA Working Paper Series No. AfD-0909. Center of Evaluation for Global Action. University of California, Berkeley. Transaction Costs and Smallholder Farmers’ Participation in Banana Markets in the Great Lakes Region John Jagwe1, 2, Emily Ouma2, Charles Machethe1 1Department of Agricultural Economics, Extension and Rural Development, University of Pretoria (LEVLO, 002, Pretoria, South Africa); 2International Institute of Tropical Agriculture, Burundi, c/o IRAZ, B.P. 91 Gitega Keywords: smallholder farmers, market participation, transaction costs, bananas Abstract. This article analyses the determinants of the discrete decision of a household on whether to participate in banana markets using the FIML bivariate probit method. The continuous decision on how much to sell or buy is analyzed by establishing the supply and demand functions while accounting for the selectivity bias. Results indicate that buying and selling decisions are not statistically independent and the random disturbances in the buying and selling decisions are affected in opposite directions by random shocks. -

The Burundi Peace Process
ISS MONOGRAPH 171 ISS Head Offi ce Block D, Brooklyn Court 361 Veale Street New Muckleneuk, Pretoria, South Africa Tel: +27 12 346-9500 Fax: +27 12 346-9570 E-mail: [email protected] Th e Burundi ISS Addis Ababa Offi ce 1st Floor, Ki-Ab Building Alexander Pushkin Street PEACE CONDITIONAL TO CIVIL WAR FROM PROCESS: THE BURUNDI PEACE Peace Process Pushkin Square, Addis Ababa, Ethiopia Th is monograph focuses on the role peacekeeping Tel: +251 11 372-1154/5/6 Fax: +251 11 372-5954 missions played in the Burundi peace process and E-mail: [email protected] From civil war to conditional peace in ensuring that agreements signed by parties to ISS Cape Town Offi ce the confl ict were adhered to and implemented. 2nd Floor, Armoury Building, Buchanan Square An AU peace mission followed by a UN 160 Sir Lowry Road, Woodstock, South Africa Tel: +27 21 461-7211 Fax: +27 21 461-7213 mission replaced the initial SA Protection Force. E-mail: [email protected] Because of the non-completion of the peace ISS Nairobi Offi ce process and the return of the PALIPEHUTU- Braeside Gardens, Off Muthangari Road FNL to Burundi, the UN Security Council Lavington, Nairobi, Kenya Tel: +254 20 386-1625 Fax: +254 20 386-1639 approved the redeployment of an AU mission to E-mail: [email protected] oversee the completion of the demobilisation of ISS Pretoria Offi ce these rebel forces by December 2008. Block C, Brooklyn Court C On 18 April 2009, at a ceremony to mark the 361 Veale Street ON beginning of the demobilisation of thousands New Muckleneuk, Pretoria, South Africa DI Tel: +27 12 346-9500 Fax: +27 12 460-0998 TI of PALIPEHUTU-FNL combatants, Agathon E-mail: [email protected] ON Rwasa, leader of PALIPEHUTU-FNL, gave up AL www.issafrica.org P his AK-47 and military uniform. -

Land Reform in Burundi: Waiting for Change After Twenty Years of Fruitless Debate
Dominik Kohlhagen [email protected] Land reform in Burundi: Waiting for change after twenty years of fruitless debate INTRODUCTION Burundi is a landlocked country in East Africa, neighboring Rwanda, Tanzania and the Democratic Republic of Congo. With its 8,5 million inhabitants living on 28,000 square kilometres, it is comparable in size and inhabitants to Belgium or Catalonia. In Africa, it is the second most densely populated country after Rwanda. Its economy heavily depends on the agricultural sector and relies to a large extent on subsistence farming. Since independence from Belgium in 1962, Burundi has experienced several outbreaks of violence. Important interethnic massacres occurred in 1965, 1969, 1972, 1988 and 1991. Between 1993 and 2005, a civil war has caused hundreds of thousands of deaths. At all these occasions, people were displaced or had to seek refuge in neighboring countries, leaving behind their land and livestock. Following a relative political and military stabilization, many refugees have recently returned to Burundi and are now trying to recover their land. Demands for land or compensation by returning refugees are currently adding to many other problems caused by land scarcity and inappropriate land laws. The current land code of Burundi, which was promulgated only in 1986, is mainly a compilation of former colonial laws and retained most of the shortcomings of preceding texts. Under the 1986 code, the country saw a significant increase in land conflicts and many illegal land allocations. A reform of the land code has been discussed by government officials and international donors since the 1990s. But up to now, all these discussions proved fruitless. -

An Estimated Dynamic Model of African Agricultural Storage and Trade
High Trade Costs and Their Consequences: An Estimated Dynamic Model of African Agricultural Storage and Trade Obie Porteous Online Appendix A1 Data: Market Selection Table A1, which begins on the next page, includes two lists of markets by country and town population (in thousands). Population data is from the most recent available national censuses as reported in various online databases (e.g. citypopulation.de) and should be taken as approximate as census years vary by country. The \ideal" list starts with the 178 towns with a population of at least 100,000 that are at least 200 kilometers apart1 (plain font). When two towns of over 100,000 population are closer than 200 kilometers the larger is chosen. An additional 85 towns (italics) on this list are either located at important transport hubs (road junctions or ports) or are additional major towns in countries with high initial population-to-market ratios. The \actual" list is my final network of 230 markets. This includes 218 of the 263 markets on my ideal list for which I was able to obtain price data (plain font) as well as an additional 12 markets with price data which are located close to 12 of the missing markets and which I therefore use as substitutes (italics). Table A2, which follows table A1, shows the population-to-market ratios by country for the two sets of markets. In the ideal list of markets, only Nigeria and Ethiopia | the two most populous countries | have population-to-market ratios above 4 million. In the final network, the three countries with more than two missing markets (Angola, Cameroon, and Uganda) are the only ones besides Nigeria and Ethiopia that are significantly above this threshold. -

African Elections in 2015: a Snapshot for Côte D'ivoire, Tanzania, Burkina
AFRICAN ELECTIONS IN 2015: A SNAPSHOT FOR CÔTE D’IVOIRE, TANZANIA, BURKINA FASO AND SUDAN John Mukum Mbaku, Nonresident Senior Fellow, Africa Growth Initiative INTRODUCTION democratic constitution making to provide each country with institutional arrangements In 2015, many countries in Africa—including that guarantee the rule of law—where the the Burkina Faso, Burundi, Chad, Egypt, latter exists, the law is supreme; a majority of Ethiopia, Guinea, Libya, Mauritius, Niger, the citizens voluntarily accept and respect the South Sudan, Sudan, Tanzania, Togo and law; there is judicial independence; the law is Zambia—will conduct presidential and/or not administered arbitrarily or capriciously but legislative elections. Most of these countries citizens are able to expect predictable results; have struggled with transition to democracy at there is protection of human rights, including least since the mid-1980s, and some of them those of minority ethnic and religious groups; much more recently. The 2015 elections, then, and governments operate in an open and for some, could be turning points for embrac- transparent manner. ing democracy more closely, and, for others, for significantly deepening and institutional- Openness and transparency are very important izing democracy and emerging as democratic for governance in Africa. Making certain that strongholds on the continent. public policies are designed and implemented in an open and transparent manner not only re- The failure to manage ethnic and religious di- duces corruption but also improves the chanc- versity and provide institutional structures that es that these policies will reflect the values, enhance peaceful coexistence, national inte- interests and aspirations of the country’s rele- gration and nation-building, remains one of vant stakeholders. -

Burundi's Constitution of 2005
PDF generated: 26 Aug 2021, 16:21 constituteproject.org Burundi's Constitution of 2005 Historical This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:21 Table of contents Preamble . 4 TITLE I: Of THE STATE AND THE SOVEREIGNTY OF THE PEOPLE . 5 1. Of the General Principles . 5 2. OF THE FUNDAMENTAL VALUES . 6 TITLE II: OF THE CHARTER OF THE FUNDAMENTAL RIGHTS AND DUTIES OF THE INDIVIDUAL AND CITIZEN . 7 1. OF THE FUNDAMENTAL RIGHTS OF THE INDIVIDUAL AND THE CITIZEN . 7 2. Of the Fundamental Responsibilities of the Individual and the Citizen . 12 TITLE III: OF THE SYSTEM OF THE POLITICAL PARTIES . 14 TITLE IV: OF ELECTIONS . 16 TITLE V: OF THE EXECUTIVE POWER . 17 1. Of the President of the Republic . 17 2. Of the Vice Presidents of the Republic . 22 3. Of Government . 23 Title VI: Of the Legislative Power . 26 1. The Provisions Common to the National Assembly and Senate . 26 2. Of the National Assembly . 30 3. Of the Senate . 33 4. Of the Procedure of Adopting New Law . 36 TITLE VII: OF THE RELATIONS BETWEEN THE EXECUTIVE AND THE LEGISLATIVE . 37 TITLE VIII: OF THE JUDICIAL POWER . 40 1. Of the Superior Council of the Magistracy . 40 2. Of the Supreme Court . 42 3. Of the Constitutional Court . 42 4. OF THE HIGH COURT OF JUSTICE . 44 TITLE IX: OF THE OMBUDSMAN . 45 TITLE X: OF DEFENSE AND OF SECURITY . 45 TITLE XI: OF THE LOCAL COLLECTIVITIES . -

Burundi Situation
BURUNDI SITUATION The Burundi situation remains one of the least-funded refugee situations in the world. As of June 2020, 333,703 Burundian refugees were in the Democratic Republic of the Congo, Rwanda, the United Republic of Tanzania and Uganda. COVID-19 has exacerbated the already precarious UNHCR’s overall requirements for the Burundi condition of Burundian refugees in the region, situation in 2020 stand at $189.9 million. As of 25 including pressure on the health and sanitation August 2020, $19 million has been received. systems in remote areas of countries of asylum. Flexible and country-level funds received by Some Burundian refugees have opted for UNHCR have allowed the organization to allocate voluntary repatriation, which is ongoing from the an additional $48.5 million to the Burundi United Republic of Tanzania and was initiated situation, raising the current funding level to 36%. BURUNDI recently from Rwanda. UNHCR is not promoting These low funding levels have forced UNHCR’s return but is assisting those refugees who indicate operations in Burundi and in neighbouring they have made an informed choice to repatriate. countries to cut programmes and activities across SITUATION a range of sectors, including voluntary repatriation, water, sanitation and hygiene, education and cash assistance, with cuts A child draws on a blackboard in an outdoor classroom at anticipated to other programmes should further Jugudi primary school school in Nyarugusu refugee camp, funding not be received. Kigoma province, western United Republic of Tanzania.