An Autochthonous Human Case of Fasciolopsiasis in Nepal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Waterborne Zoonotic Helminthiases Suwannee Nithiuthaia,*, Malinee T
Veterinary Parasitology 126 (2004) 167–193 www.elsevier.com/locate/vetpar Review Waterborne zoonotic helminthiases Suwannee Nithiuthaia,*, Malinee T. Anantaphrutib, Jitra Waikagulb, Alvin Gajadharc aDepartment of Pathology, Faculty of Veterinary Science, Chulalongkorn University, Henri Dunant Road, Patumwan, Bangkok 10330, Thailand bDepartment of Helminthology, Faculty of Tropical Medicine, Mahidol University, Ratchawithi Road, Bangkok 10400, Thailand cCentre for Animal Parasitology, Canadian Food Inspection Agency, Saskatoon Laboratory, Saskatoon, Sask., Canada S7N 2R3 Abstract This review deals with waterborne zoonotic helminths, many of which are opportunistic parasites spreading directly from animals to man or man to animals through water that is either ingested or that contains forms capable of skin penetration. Disease severity ranges from being rapidly fatal to low- grade chronic infections that may be asymptomatic for many years. The most significant zoonotic waterborne helminthic diseases are either snail-mediated, copepod-mediated or transmitted by faecal-contaminated water. Snail-mediated helminthiases described here are caused by digenetic trematodes that undergo complex life cycles involving various species of aquatic snails. These diseases include schistosomiasis, cercarial dermatitis, fascioliasis and fasciolopsiasis. The primary copepod-mediated helminthiases are sparganosis, gnathostomiasis and dracunculiasis, and the major faecal-contaminated water helminthiases are cysticercosis, hydatid disease and larva migrans. Generally, only parasites whose infective stages can be transmitted directly by water are discussed in this article. Although many do not require a water environment in which to complete their life cycle, their infective stages can certainly be distributed and acquired directly through water. Transmission via the external environment is necessary for many helminth parasites, with water and faecal contamination being important considerations. -

Public Health Significance of Intestinal Parasitic Infections*
Articles in the Update series Les articles de la rubrique give a concise, authoritative, Le pointfournissent un bilan and up-to-date survey of concis et fiable de la situa- the present position in the tion actuelle dans les do- Update selectedfields, coveringmany maines consideres, couvrant different aspects of the de nombreux aspects des biomedical sciences and sciences biomedicales et de la , po n t , , public health. Most of santepublique. Laplupartde the articles are written by ces articles auront donc ete acknowledged experts on the redigeis par les specialistes subject. les plus autorises. Bulletin of the World Health Organization, 65 (5): 575-588 (1987) © World Health Organization 1987 Public health significance of intestinal parasitic infections* WHO EXPERT COMMITTEE' Intestinal parasitic infections are distributed virtually throughout the world, with high prevalence rates in many regions. Amoebiasis, ascariasis, hookworm infection and trichuriasis are among the ten most common infections in the world. Other parasitic infections such as abdominal angiostrongyliasis, intestinal capil- lariasis, and strongyloidiasis are of local or regional public health concern. The prevention and control of these infections are now more feasible than ever before owing to the discovery of safe and efficacious drugs, the improvement and sim- plification of some diagnostic procedures, and advances in parasite population biology. METHODS OF ASSESSMENT The amount of harm caused by intestinal parasitic infections to the health and welfare of individuals and communities depends on: (a) the parasite species; (b) the intensity and course of the infection; (c) the nature of the interactions between the parasite species and concurrent infections; (d) the nutritional and immunological status of the population; and (e) numerous socioeconomic factors. -

Public Health Significance of Foodborne
imental er Fo p o x d E C Journal of Experimental Food f h o e l m a n i Pal et al., J Exp Food Chem 2018, 4:1 s r t u r y o J Chemistry DOI: 10.4172/2472-0542.1000135 ISSN: 2472-0542 Review Article Open Access Public Health Significance of Foodborne Helminthiasis: A Systematic Review Mahendra Pal1*, Yodit Ayele2, Angesom Hadush3, Pooja Kundu4 and Vijay J Jadhav4 1Narayan Consultancy on Veterinary Public Health, 4 Aangan, Jagnath Ganesh Dairy Road, Anand-38001, India 2Department of Animal Science, College of Agriculture and Natural Resources, Bonga University, Post Box No.334, Bonga, Ethiopia 3Department of Animal Production and Technology, College of Agriculture and Environmental Sciences, Adigrat University, P.O. Box 50, Adigrat, Ethiopia 4Department of Veterinary Public Health and Epidemiology, College of Veterinary Sciences, LUVAS, Hisar-125004, India *Corresponding author: Mahendra Pal, Narayan Consultancy on Veterinary Public Health and Microbiology, 4 Aangan, Jagnath Ganesh Dairy Road, Anand-388001, Gujarat, India, E-mail: [email protected] Received date: December 18, 2017; Accepted date: January 19, 2018; Published date: January 25, 2018 Copyright: ©2017 Pal M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Foodborne diseases, caused by biological as well as chemical agents, have an impact in both developing and developed nations. The foodborne diseases of microbial origin are acute where as those caused by chemical toxicants are resulted due to chronic exposure. -

TCM Diagnostics Applied to Parasite-Related Disease
TCM Diagnostics Applied to Parasite-Related Disease by Laraine Crampton, M.A.T.C.M., L. Ac. Capstone Advisor: Lawrence J. Ryan, Ph.D. Presented in partial fulfillment of the requirements for the degree Doctor of Acupuncture and Oriental Medicine Yo San University of Traditional Chinese Medicine Los Angeles, California April 2014 TCM and Parasites/Crampton 2 Approval Signatures Page This Capstone Project has been reviewed and approved by: April 30th, 2014 ____________________________________________________________________________ Lawrence J. Ryan, Ph. D. Capstone Project Advisor Date April 30th, 2014 ________________________________________________________________________ Don Lee, L. Ac. Specialty Chair Date April 30th, 2014 ________________________________________________________________________ Andrea Murchison, D.A.O.M., L.Ac. Program Director Date TCM and Parasites/Crampton 3 Abstract Complex, chronic disease affects millions in the United States, imposing a significant cost to the affected individuals and the productivity and economic realities those individuals and their families, workplaces and communities face. There is increasing evidence leading towards the probability that overlooked and undiagnosed parasitic disease is a causal, contributing, or co- existent factor for many of those afflicted by chronic disease. Yet, frustratingly, inadequate diagnostic methods and clever adaptive mechanisms in parasitic organisms mean that even when physicians are looking for parasites, they may not find what is there to be found. Examining the practice of medicine in the United States just over a century ago reveals that fully a third of diagnostic and treatment concerns for leading doctors of the time revolved around parasitic organisms and related disease, and that the population they served was largely located in rural areas. By the year 2000, more than four-fifths of the population had migrated to cities, enjoying the benefits of municipal services, water treatment systems, grocery stores and restaurants. -

Praziquantel Treatment in Trematode and Cestode Infections: an Update
Review Article Infection & http://dx.doi.org/10.3947/ic.2013.45.1.32 Infect Chemother 2013;45(1):32-43 Chemotherapy pISSN 2093-2340 · eISSN 2092-6448 Praziquantel Treatment in Trematode and Cestode Infections: An Update Jong-Yil Chai Department of Parasitology and Tropical Medicine, Seoul National University College of Medicine, Seoul, Korea Status and emerging issues in the use of praziquantel for treatment of human trematode and cestode infections are briefly reviewed. Since praziquantel was first introduced as a broadspectrum anthelmintic in 1975, innumerable articles describ- ing its successful use in the treatment of the majority of human-infecting trematodes and cestodes have been published. The target trematode and cestode diseases include schistosomiasis, clonorchiasis and opisthorchiasis, paragonimiasis, het- erophyidiasis, echinostomiasis, fasciolopsiasis, neodiplostomiasis, gymnophalloidiasis, taeniases, diphyllobothriasis, hyme- nolepiasis, and cysticercosis. However, Fasciola hepatica and Fasciola gigantica infections are refractory to praziquantel, for which triclabendazole, an alternative drug, is necessary. In addition, larval cestode infections, particularly hydatid disease and sparganosis, are not successfully treated by praziquantel. The precise mechanism of action of praziquantel is still poorly understood. There are also emerging problems with praziquantel treatment, which include the appearance of drug resis- tance in the treatment of Schistosoma mansoni and possibly Schistosoma japonicum, along with allergic or hypersensitivity -

Parasitic Organisms Chart
Parasitic organisms: Pathogen (P), Potential pathogen (PP), Non-pathogen (NP) Parasitic Organisms NEMATODESNematodes – roundworms – ROUNDWORMS Organism Description Epidemiology/Transmission Pathogenicity Symptoms Ancylostoma -Necator Hookworms Found in tropical and subtropical Necator can only be transmitted through penetration of the Some are asymptomatic, though a heavy burden is climates, as well as in areas where skin, whereas Ancylostoma can be transmitted through the associated with anemia, fever, diarrhea, nausea, Ancylostoma duodenale Soil-transmitted sanitation and hygiene are poor.1 skin and orally. vomiting, rash, and abdominal pain.2 nematodes Necator americanus Infection occurs when individuals come Necator attaches to the intestinal mucosa and feeds on host During the invasion stages, local skin irritation, elevated into contact with soil containing fecal mucosa and blood.2 ridges due to tunneling, and rash lesions are seen.3 matter of infected hosts.2 (P) Ancylostoma eggs pass from the host’s stool to soil. Larvae Ancylostoma and Necator are associated with iron can penetrate the skin, enter the lymphatics, and migrate to deficiency anemia.1,2 heart and lungs.3 Ascaris lumbricoides Soil-transmitted Common in Sub-Saharan Africa, South Ascaris eggs attach to the small intestinal mucosa. Larvae Most patients are asymptomatic or have only mild nematode America, Asia, and the Western Pacific. In migrate via the portal circulation into the pulmonary circuit, abdominal discomfort, nausea, dyspepsia, or loss of non-endemic areas, infection occurs in to the alveoli, causing a pneumonitis-like illness. They are appetite. Most common human immigrants and travelers. coughed up and enter back into the GI tract, causing worm infection obstructive symptoms.5 Complications include obstruction, appendicitis, right It is associated with poor personal upper quadrant pain, and biliary colic.4 (P) hygiene, crowding, poor sanitation, and places where human feces are used as Intestinal ascariasis can mimic intestinal obstruction, fertilizer. -

Proteomic Insights Into the Biology of the Most Important Foodborne Parasites in Europe
foods Review Proteomic Insights into the Biology of the Most Important Foodborne Parasites in Europe Robert Stryi ´nski 1,* , El˙zbietaŁopie ´nska-Biernat 1 and Mónica Carrera 2,* 1 Department of Biochemistry, Faculty of Biology and Biotechnology, University of Warmia and Mazury in Olsztyn, 10-719 Olsztyn, Poland; [email protected] 2 Department of Food Technology, Marine Research Institute (IIM), Spanish National Research Council (CSIC), 36-208 Vigo, Spain * Correspondence: [email protected] (R.S.); [email protected] (M.C.) Received: 18 August 2020; Accepted: 27 September 2020; Published: 3 October 2020 Abstract: Foodborne parasitoses compared with bacterial and viral-caused diseases seem to be neglected, and their unrecognition is a serious issue. Parasitic diseases transmitted by food are currently becoming more common. Constantly changing eating habits, new culinary trends, and easier access to food make foodborne parasites’ transmission effortless, and the increase in the diagnosis of foodborne parasitic diseases in noted worldwide. This work presents the applications of numerous proteomic methods into the studies on foodborne parasites and their possible use in targeted diagnostics. Potential directions for the future are also provided. Keywords: foodborne parasite; food; proteomics; biomarker; liquid chromatography-tandem mass spectrometry (LC-MS/MS) 1. Introduction Foodborne parasites (FBPs) are becoming recognized as serious pathogens that are considered neglect in relation to bacteria and viruses that can be transmitted by food [1]. The mode of infection is usually by eating the host of the parasite as human food. Many of these organisms are spread through food products like uncooked fish and mollusks; raw meat; raw vegetables or fresh water plants contaminated with human or animal excrement. -

Controlling Disease Due to Helminth Infections
During the past decade there have been major efforts to plan, Controlling disease due to helminth infections implement, and sustain measures for reducing the burden of human ControllingControlling diseasedisease disease that accompanies helminth infections. Further impetus was provided at the Fifty-fourth World Health Assembly, when WHO duedue toto Member States were urged to ensure access to essential anthelminthic drugs in health services located where the parasites – schistosomes, roundworms, hookworms, and whipworms – are endemic. The helminthhelminth infectionsinfections Assembly stressed that provision should be made for the regular anthelminthic treatment of school-age children living wherever schistosomes and soil-transmitted nematodes are entrenched. This book emerged from a conference held in Bali under the auspices of the Government of Indonesia and WHO. It reviews the science that underpins the practical approach to helminth control based on deworming. There are articles dealing with the public health significance of helminth infections, with strategies for disease control, and with aspects of anthelminthic chemotherapy using high-quality recommended drugs. Other articles summarize the experience gained in national and local control programmes in countries around the world. Deworming is an affordable, cost-effective public health measure that can be readily integrated with existing health care programmes; as such, it deserves high priority. Sustaining the benefits of deworming depends on having dedicated health professionals, combined with political commitment, community involvement, health education, and investment in sanitation. "Let it be remembered how many lives and what edited by a fearful amount of suffering have been saved by D.W.T. Crompton the knowledge gained of parasitic worms through A. -

Case Report Fasciolopsiasis
SOUTHEAST ASIAN J TROP MED PUBLIC HEALTH CASE REPORT FASCIOLOPSIASIS: A FIRST CASE REPORT FROM MALAYSIA M Rohela1, I Jamaiah1, J Menon2 and J Rachel2 1Department of Parasitology, Faculty of Medicine, University of Malaya, Kuala Lumpur; 2Hospital Queen Elizabeth, Kota Kinabalu, Sabah, Malaysia Abstract. Fasciolopsiasis is a disease caused by the largest intestinal fluke, Fasciolopsis buski. The disease is endemic in the Far East and Southeast Asia. Human acquires the infection after eating raw freshwater plants contaminated with the infective metacercariae. There has been no report of fasciolopsiasis either in man or in animal in Malaysia. We are reporting the first case of fasciolopsia- sis in Malaysia in a 39-year-old female farmer, a native of Sabah (East Malaysia). This patient com- plained of cough and fever for a duration of two weeks, associated with loss of appetite and loss of weight. She had no history of traveling overseas. Physical examination showed pallor, multiple cer- vical and inguinal lymph nodes and hepatosplenomegaly. Laboratory investigations showed that she had iron deficiency anemia. There was leukocytosis and a raised ESR. Lymph node biopsy revealed a caseating granuloma. Stool examination was positive for the eggs of Fasciolopsis buski. The eggs measure 140 x 72.5 µm and are operculated. In this case, the patient did not present with symp- toms suggestive of any intestinal parasitic infections. Detection of Fasciolopsis buski eggs in the stool was an incidental finding. She was diagnosed as a case of disseminated tuberculosis with fasciolopsiasis and was treated with antituberculosis drugs and praziquantel, respectively. INTRODUCTION ate other fresh water plants including water cal- trop, watercress and morning glory (Bunnag et Fasciolopsiasis is a disease caused by the al, 1983). -

Fasciolopsis Buski • Liver Fluke Clonorchis Sinensis • Lung Fluke Paragonimus Westermani
TREMATODES PM2 Pathophysiology Trematodes • multicellular eukaryotic helminths • unsegmented leaf- shaped worms • MONECIOUS except for schistosomes (DIECIOUS) TREMATODES • blood flukes Schistosoma mansoni S. japonicum S. hematobium. • intestinal fluke Fasciolopsis buski • liver fluke Clonorchis sinensis • lung fluke Paragonimus westermani. Trematodes • MOT: 1. cercariae - FREE SWIMMING LARVAE - given off by infected snail - penetrate the skin of the human definitive host 2. metacercariae - encysted form of the cercariae - edible plants or animals water plants fishs crustaceans • Praziquantel -paralysis of musculature -attachment of phagocytes to parasite and death. Schistosomiasis (Bilharziasis) • S. hematobium: Africa • S. mansoni : Africa and America • S. japonicum: Far East. • 250 million people are infected Morphology • Adult worms are 10 to 20 mm long • Male: lamelliform shape with marginal folds “The sweetest parasites on earth” SCHISTOSOMES MOT: skin penetration by cercariae FAVORITE SITES • S. japonicum :VEINS OF GIT • S. mansoni : VEINS OF GIT • S. haematobium : VEINS OF BLADDER Schistosomiasis • type I and type IV hypersensitivity • collagenase: damage to the vascular endothelium. Three major disease syndromes occur in schistosomiasis • 1. schistosome dermatitis • 2. acute schistosomias (Katayama fever) • 3. chronic schistosomiasis. dermatitis (swimmers' itch): penetration of cercariae Acute schistosomiasis (Katayama fever) -4 to 8 weeks after primary exposure -cough, hepatosplenomegaly -lymphadenopathy,and eosinophilia Chronic disease • may appear many years later • japonica and mansoni hepatomegaly splenomegaly portal hypertension esophageal varices • schistosomiasis haematobium inflammation and fibrosis obstruction hydronephrosis uremia Schistosoma eggs in the intestinal mucosa S. Haematobium and bladder cancer Schistosomiasis Characteristic eggs: diagnosis Apical spine: S. haematobium Lateral spine: S. mansoni Vestigial spine: S. japonicum Treatment and control • Praziquantel is effective against all species. • Contaminated water should be avoided. -

Zoonotic Infections – an Overview
14.1 CHAPTER 14 Zoonotic infections – an overview John M. Goldsmid 14.1 INTRODUCTION Zoonotic infections can be defined as infections of animals that are naturally transmissible to humans. As such they are worldwide and often spread with humans through their companion and domestic animals. However, when humans move to new areas or come into contact with different animal species (eg moving into newly cleared natural forest areas), then new zoonoses may emerge or are recognised, and it is significant that many of the new or newly recognised emerging infections of humans are zoonotic in origin1. The probable reasons for the emergence of new zoonotic diseases are many and include, as described by McCarthy and Moore2 for the Helminth zoonoses: “changes in social, dietary or cultural mores, environmental changes, and the improved recognition of heretofore neglected infections often coupled with an improved ability to diagnose infection”. Zoonotic infections may be very localised in their distribution and often reflect particular associations between the natural reservoir hosts and humans – they are thus often influenced by human dietary habits, behaviour and relationships with different animal species. For the practising physician, the knowledge that a disease is zoonotic, is of particular significance in the differential diagnosis (hence the need in all history taking, of asking the question of contact with animals), and in the prevention and control of such diseases. A list of the more important/significant zoonotic infections is given in Table 1 which also outlines the aetiological agent of the disease; its usual animal reservoir host and rough geographical distribution. In some cases, where the vector may serve as a reservoir, it is included under reservoir hosts. -
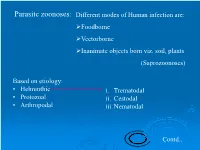
Parasitc Zoonoses: Different Modes of Human Infection Are: Foodborne Vectorborne Inanimate Objects Born Viz
Parasitc zoonoses: Different modes of Human infection are: Foodborne Vectorborne Inanimate objects born viz. soil, plants (Saprozoonoses) Based on etiology: • Helminthic i. Trematodal • Protozoal ii. Cestodal • Arthropodal iii. Nematodal Contd.. Snail borne diseases Contd.. Trematode Final host Intermediate host Transmission to humans Fasciolopsiasis: Man, dog and buffalo; Snail Ingestion of Fasciolopsis buski Pig (reservoir) metacercaria on water chestnut Schistosomiasis: Man and other Snail Skin penetration S. hematobium, mammals by cercaria S. mansoni, S. Japonicum Clonorchiasis: Man, dog, cat, pig, rat 1st snail Ingestion of cyst Clonorchis sinensis 2nd freshwater in fish (Chinese liver fluke) fishes esp. cyprinid Opisthorchiasis: Man and fish eating 1st snail Ingestion of cyst Opisthorchis felineus mammals; Dog and 2nd cyprinid fish in fish O. viverrini cat-(reservoir) Paragonimiasis: Man, dog, cat and 1st snail Ingestion of cyst Paragonimus other mammals 2nd fresh water in crab meat westermanni crabs and fishes Fasciolopsiasis: •Fasciolopsis buski •Intestinal-ulcerous disease in humans •Humans and pigs are final hosts; pigs are reservoirs. Infective stage (metcercaria) via ingestion of contaminated water chest nuts and walnuts which are eaten raw. Contd.. Occurrence: Areas of endemicity are large parts of the People’s Republic of China and Taiwan, India, Bangladesh, Indonesia, Thailand, and Vietnam. Disease occurs focally and is most prevalent in school-age children. The prevalence of infection in children ranges: 60% in India 57% in China 50% in Bangladesh 25% in Taiwan, and 10% in Thailand [Nithiuthai et al. 2004] Schistosomiasis (Bilharziosis) Common in tropical and subtropical areas Schistosome Type of infection Occurrence Reservoir Hosts species caused (highly (zoonotic) prevalent) S. hematobium Schistosomiasis of North America, Not important, but urinary tract Africa monkey, pig and rodents may play role S.