Praziquantel Treatment in Trematode and Cestode Infections: an Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Dicrocoelium Dendriticum
Links For more information, please contact your Regional Veterinarian or the Animal Ontario Ministry of Agriculture, Food, and Health Division. Rural Affairs www.omafra.gov.on.ca under Sheep Health and Diseases Dicrocoelium dendriticum: Other information pamphlets are The Lancet Fluke of available online from the Department of Natural Resources at: Sheep www.nr.gov.nl.ca/agric/ Publication: VS 02-001 Last Revised: March 2010 Department of Natural Resources Animal Health Division P.O. Box 7400 St. John's, NL A1E 3Y5 t 709.729.6879 f 709.729.0055 [email protected] Introduction Snails eat the eggs which hatch and eventually form cercaria. The cercaria live in the Dicrocoelium can also be snail’s respiratory chamber and are released to the environment in slime balls. It normally diagnosed by finding eggs by fecal Infection by parasites is a major takes three to four months for the parasite to complete the snail portion of its life cycle. flotation. Routine flotation techniques concern of anyone who raises sheep. A may not show Dicrocoelium, and group of parasites that are often The slime balls are a favoured food of ants; and once ingested, the cercaria move to techniques intended specifically for fluke overlooked are the flukes (also called the abdomen of the ant. One or two of these cercaria move to the ant’s head and establish diagnosis may be required. flatworms or trematodes). The lancet themselves in the brain. When cercaria are present in the brain, ants which normally move fluke (or small liver fluke), Dicrocoelium into their nests with cold temperatures will move up to the tops of vegetation. -
A Literature Survey of Common Parasitic Zoonoses Encountered at Post-Mortem Examination in Slaughter Stocks in Tanzania: Economic and Public Health Implications
Volume 1- Issue 5 : 2017 DOI: 10.26717/BJSTR.2017.01.000419 Erick VG Komba. Biomed J Sci & Tech Res ISSN: 2574-1241 Research Article Open Access A Literature Survey of Common Parasitic Zoonoses Encountered at Post-Mortem Examination in Slaughter Stocks in Tanzania: Economic and Public Health Implications Erick VG Komba* Department of Veterinary Medicine and Public Health, Sokoine University of Agriculture, Tanzania Received: September 21, 2017; Published: October 06, 2017 *Corresponding author: Erick VG Komba, Senior lecturer, Department of Veterinary Medicine and Public Health, College of Veterinary Medicine and Biomedical Sciences, Sokoine University of Agriculture, P.O. Box 3021, Morogoro, Tanzania Abstract Zoonoses caused by parasites constitute a large group of infectious diseases with varying host ranges and patterns of transmission. Their public health impact of such zoonoses warrants appropriate surveillance to obtain enough information that will provide inputs in the design anddistribution, implementation prevalence of control and transmission strategies. Apatterns need therefore are affected arises by to the regularly influence re-evaluate of both human the current and environmental status of zoonotic factors. diseases, The economic particularly and in view of new data available as a result of surveillance activities and the application of new technologies. Consequently this paper summarizes available information in Tanzania on parasitic zoonoses encountered in slaughter stocks during post-mortem examination at slaughter facilities. The occurrence, in slaughter stocks, of fasciola spp, Echinococcus granulosus (hydatid) cysts, Taenia saginata Cysts, Taenia solium Cysts and ascaris spp. have been reported by various researchers. Information on these parasitic diseases is presented in this paper as they are the most important ones encountered in slaughter stocks in the country. -

Examination of Some Endoparasites Prevalence in Romanov Sheep Imported from Ukraine
Harran Üniv Vet Fak Derg, 2019; 8 (1): 99-103 Research Article Examination of Some Endoparasites Prevalence in Romanov Sheep Imported from Ukraine Adnan AYAN1*, Turan YAMAN2, Ömer Faruk KELEŞ2, Hidayet TUTUN3 1Department of Genetics, Faculty of Veterinary Medicine, Van Yuzuncu Yil University, Van, Turkey. 2Department of Pathology, Faculty of Veterinary Medicine, Van Yuzuncu Yil University, Van, Turkey. 3Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Burdur Mehmet Akif Ersoy University, Burdur, Turkey. Geliş Tarihi: 11.09.2018 Kabul Tarihi: 27.05.2019 Abstract: The purpose of this study was to investigate some endoparasites spread in the Romanov sheep imported from Ukraine. The flotation, sedimentation and Baerman-Wetzel techniques were used to analyze the fecal samples collected from the sheep (n=156) and the samples were examined under the light microscope. Furthermore, from this herd, the internal organs of the sheep that had died were pathologically examined on macroscopic and microscopic level. Among fecal samples examined 69 (44.23%) were found parasitically positive, 66 of these (42.3%) were found positive for Dicrocoelium dentriticum, 3 samples (1.92%) were positive for Nematodirus spp. and Eimeria spp, while Giardia spp. was not detected. The pathological examination of the internal organs of eight of these sheep revealed adult forms of D. dendriticum only in the liver. The parasitological and pathological findings of this study indicated a high incidence of D. dendriticum that causes economic losses due to cases of death, in the Romanov sheep, which has been imported to country in large numbers in recent years. Keywords: Dicrocoelium dendriticum, Helminth, Protozoan, Romanov sheep. -

Pulmonary Edema Associated with Ascaris Lumbricoides in a Patient with Mild Mitral Stenosis: a Case Report
Eur J Gen Med 2004; 1(2): 43-45 CASE REPORT PULMONARY EDEMA ASSOCIATED WITH ASCARIS LUMBRICOIDES IN A PATIENT WITH MILD MITRAL STENOSIS: A CASE REPORT Talantbek Batyraliev1, Beyhan Eryonucu2, Zarema Karben1, Hakan Sengul1, Niyazi Güler2, Orhan Dogru1, Alper Sercelik1 Sani Konukoglu Medical Center , Department of Cardiology1 Yüzüncü Yıl University, Department of Cardiology2 Ascaris lumbricoides remains the most common intestinal nematode in the world. Clinical manifestations of ascaris lumbricoides are different in each stage of the infection. We presented an unusual presentation of ascaris lumbricoides. Key words: Pulmonary oedema, mild mitral stenosis, Ascaris lumbricoides INTRODUCTION oedema due to mitral stenosis. Treatment of Ascaris lumbricoides (AL) remain the most diuretics was initiated. She was placed on common intestinal nematode in the world. oxygen by nasal cannula. Tachycardia was not Clinical manifestations of AL are different taken under control by treatment with digoxin in each stage of the infection. Infection with and verapamil. A reason for excessive nausea ascaris appears to be asymptomatic in the vast and vomiting was not determined and these majority of cases, but may produce serious semptoms were not responsive to antiemetic pulmonary disease or obstruction of biliary drugs. Despite intensive treatment, clinical or intestinal tract in a small proportion of improvement was not occured. Fortunately, at infected people. We presented an unusual the 3rd day, the patient was expelled ascaris presentation of AL and pulmonary edema lumbricoides (AL) (Figure). Once the AL was (1,2). removed the patient’s respiratory condition dramatically improved. The patient was CASE started on a 3-day course of mebendazole A 27-year-old woman was admitted to and discharged 4 days later in good general our hospital because of an episode of acute condition. -

Genetic Characterization, Species Differentiation and Detection of Fasciola Spp
Ai et al. Parasites & Vectors 2011, 4:101 http://www.parasitesandvectors.com/content/4/1/101 REVIEW Open Access Genetic characterization, species differentiation and detection of Fasciola spp. by molecular approaches Lin Ai1,2,3†, Mu-Xin Chen1,2†, Samer Alasaad4, Hany M Elsheikha5, Juan Li3, Hai-Long Li3, Rui-Qing Lin3, Feng-Cai Zou6, Xing-Quan Zhu1,6,7* and Jia-Xu Chen2* Abstract Liver flukes belonging to the genus Fasciola are among the causes of foodborne diseases of parasitic etiology. These parasites cause significant public health problems and substantial economic losses to the livestock industry. Therefore, it is important to definitively characterize the Fasciola species. Current phenotypic techniques fail to reflect the full extent of the diversity of Fasciola spp. In this respect, the use of molecular techniques to identify and differentiate Fasciola spp. offer considerable advantages. The advent of a variety of molecular genetic techniques also provides a powerful method to elucidate many aspects of Fasciola biology, epidemiology, and genetics. However, the discriminatory power of these molecular methods varies, as does the speed and ease of performance and cost. There is a need for the development of new methods to identify the mechanisms underpinning the origin and maintenance of genetic variation within and among Fasciola populations. The increasing application of the current and new methods will yield a much improved understanding of Fasciola epidemiology and evolution as well as more effective means of parasite control. Herein, we provide an overview of the molecular techniques that are being used for the genetic characterization, detection and genotyping of Fasciola spp. -

Toxocariasis: a Rare Cause of Multiple Cerebral Infarction Hyun Hee Kwon Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea
Case Report Infection & http://dx.doi.org/10.3947/ic.2015.47.2.137 Infect Chemother 2015;47(2):137-141 Chemotherapy ISSN 2093-2340 (Print) · ISSN 2092-6448 (Online) Toxocariasis: A Rare Cause of Multiple Cerebral Infarction Hyun Hee Kwon Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu, Korea Toxocariasis is a parasitic infection caused by the roundworms Toxocara canis or Toxocara cati, mostly due to accidental in- gestion of embryonated eggs. Clinical manifestations vary and are classified as visceral larva migrans or ocular larva migrans according to the organs affected. Central nervous system involvement is an unusual complication. Here, we report a case of multiple cerebral infarction and concurrent multi-organ involvement due to T. canis infestation of a previous healthy 39-year- old male who was admitted for right leg weakness. After treatment with albendazole, the patient’s clinical and laboratory results improved markedly. Key Words: Toxocara canis; Cerebral infarction; Larva migrans, visceral Introduction commonly involved organs [4]. Central nervous system (CNS) involvement is relatively rare in toxocariasis, especially CNS Toxocariasis is a parasitic infection caused by infection with presenting as multiple cerebral infarction. We report a case of the roundworm species Toxocara canis or less frequently multiple cerebral infarction with lung and liver involvement Toxocara cati whose hosts are dogs and cats, respectively [1]. due to T. canis infection in a previously healthy patient who Humans become infected accidentally by ingestion of embry- was admitted for right leg weakness. onated eggs from contaminated soil or dirty hands, or by in- gestion of raw organs containing encapsulated larvae [2]. -

Globalization and Infectious Diseases: a Review of the Linkages
TDR/STR/SEB/ST/04.2 SPECIAL TOPICS NO.3 Globalization and infectious diseases: A review of the linkages Social, Economic and Behavioural (SEB) Research UNICEF/UNDP/World Bank/WHO Special Programme for Research & Training in Tropical Diseases (TDR) The "Special Topics in Social, Economic and Behavioural (SEB) Research" series are peer-reviewed publications commissioned by the TDR Steering Committee for Social, Economic and Behavioural Research. For further information please contact: Dr Johannes Sommerfeld Manager Steering Committee for Social, Economic and Behavioural Research (SEB) UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR) World Health Organization 20, Avenue Appia CH-1211 Geneva 27 Switzerland E-mail: [email protected] TDR/STR/SEB/ST/04.2 Globalization and infectious diseases: A review of the linkages Lance Saker,1 MSc MRCP Kelley Lee,1 MPA, MA, D.Phil. Barbara Cannito,1 MSc Anna Gilmore,2 MBBS, DTM&H, MSc, MFPHM Diarmid Campbell-Lendrum,1 D.Phil. 1 Centre on Global Change and Health London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK 2 European Centre on Health of Societies in Transition (ECOHOST) London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK TDR/STR/SEB/ST/04.2 Copyright © World Health Organization on behalf of the Special Programme for Research and Training in Tropical Diseases 2004 All rights reserved. The use of content from this health information product for all non-commercial education, training and information purposes is encouraged, including translation, quotation and reproduction, in any medium, but the content must not be changed and full acknowledgement of the source must be clearly stated. -

Fishery Bulletin/U S Dept of Commerce National Oceanic
Abstract.-Seventeen species of parasites representing the Cestoda, Parasite Fauna of Three Species Nematoda, Acanthocephala, and Crus tacea are reported from three spe of Antarctic Whales with cies of Antarctic whales. Thirty-five sei whales Balaenoptera borealis, Reference to Their Use 106 minke whales B. acutorostrata, and 35 sperm whales Pkyseter cato as Potentia' Stock Indicators don were examined from latitudes 30° to 64°S, and between longitudes 106°E to 108°W, during the months Murray D. Dailey ofNovember to March 1976-77. Col Ocean Studies Institute. California State University lection localities and regional hel Long Beach, California 90840 minth fauna diversity are plotted on distribution maps. Antarctic host-parasite records from Wolfgang K. Vogelbein B. borealis, B. acutorostrata, and P. Virginia Institute of Marine Science catodon are updated and tabulated Gloucester Point. Virginia 23062 by commercial whaling sectors. The use of acanthocephalan para sites of the genus Corynosoma as potential Antarctic sperm whale stock indicators is discussed. The great whales of the southern hemi easiest to find (Gaskin 1976). A direct sphere migrate annually between result of this has been the successive temperate breeding and Antarctic overexploitation of several major feeding grounds. However, results of whale species. To manage Antarctic Antarctic whale tagging programs whaling more effectively, identifica (Brown 1971, 1974, 1978; Ivashin tion and determination of whale 1988) indicate that on the feeding stocks is of high priority (Schevill grounds circumpolar movement by 1971, International Whaling Com sperm and baleen whales is minimal. mission 1990). These whales apparently do not com The Antarctic whaling grounds prise homogeneous populations were partitioned by the International whose members mix freely through Whaling Commission into commer out the entire Antarctic. -

Opisthorchiasis: an Emerging Foodborne Helminthic Zoonosis of Public Health Significance
IJMPES International Journal of http://ijmpes.com doi 10.34172/ijmpes.2020.27 Medical Parasitology & Vol. 1, No. 4, 2020, 101-104 eISSN 2766-6492 Epidemiology Sciences Review Article Opisthorchiasis: An Emerging Foodborne Helminthic Zoonosis of Public Health Significance Mahendra Pal1* ID , Dimitri Ketchakmadze2 ID , Nino Durglishvili3 ID , Yagoob Garedaghi4 ID 1Narayan Consultancy on Veterinary Public Health and Microbiology, Gujarat, India 2Faculty of Chemical Technologies and Metallurgy, Georgian Technical University, Tbilisi, Georgia 3Department of Sociology and Social Work, Ivane Javakhishvili Tbilisi State University, Tbilisi, Georgia 4Department of Parasitology, Tabriz Branch, Islamic Azad University, Tabriz, Iran Abstract Opisthorchiasis is an emerging foodborne parasitic zoonosis that has been reported from developing as well as developed nations of the world. Globally, around 80 million people are at risk of acquiring Opisthorchis infection. The source of infection is exogenous, and ingestion is considered as the primary mode of transmission. Humans get the infection by consuming raw or undercooked fish. In most cases, the infection remains asymptomatic. However, in affected individuals, the clinical manifestations are manifold. Occasionally, complications including cholangitis, cholecystitis, and cholangiocarcinoma are observed. The people who have the dietary habit of eating raw fish usually get the infection. Certain occupational groups, such as fishermen, agricultural workers, river fleet employees, and forest industry personnel are mainly infected with Opisthorchis. The travelers to the endemic regions who consume raw fish are exposed to the infection. Parasitological, immunological, and molecular techniques are employed to confirm the diagnosis of disease. Treatment regimens include oral administration of praziquantel and albendazole. In the absence of therapy, the acute phase transforms into a chronic one that may persist for two decades. -

CDC Overseas Parasite Guidelines
Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil-Transmitted Helminth Infections for Refugees Resettling to the United States U.S. Department of Health and Human Services Centers for Disease Control and Prevention National Center for Emerging and Zoonotic Infectious Diseases Division of Global Migration and Quarantine February 6, 2019 Accessible version: https://www.cdc.gov/immigrantrefugeehealth/guidelines/overseas/intestinal- parasites-overseas.html 1 Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil-Transmitted Helminth Infections for Refugees Resettling to the United States UPDATES--the following are content updates from the previous version of the overseas guidance, which was posted in 2008 • Latin American and Caribbean refugees are now included, in addition to Asian, Middle Eastern, and African refugees. • Recommendations for management of Strongyloides in refugees from Loa loa endemic areas emphasize a screen-and-treat approach and de-emphasize a presumptive high-dose albendazole approach. • Presumptive use of albendazole during any trimester of pregnancy is no longer recommended. • Links to a new table for the Treatment Schedules for Presumptive Parasitic Infections for U.S.-Bound Refugees, administered by IOM. Contents • Summary of Recommendations • Background • Recommendations for overseas presumptive treatment of intestinal parasites o Refugees originating from the Middle East, Asia, North Africa, Latin America, and the Caribbean o Refugees -
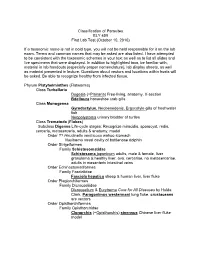
Classification of Parasites BLY 459 First Lab Test (October 10, 2010)
Classification of Parasites BLY 459 First Lab Test (October 10, 2010) If a taxonomic name is not in bold type, you will not be held responsible for it on the lab exam. Terms and common names that may be asked are also listed. I have attempted to be consistent with the taxonomic schemes in your text as well as to list all slides and live specimens that were displayed. In addition to highlighted taxa, be familiar with, material in lab handouts (especially proper nomenclature), lab display sheets, as well as material presented in lecture. Questions about vectors and locations within hosts will be asked. Be able to recognize healthy from infected tissue. Phylum Platyhelminthes (Flatworms) Class Turbellaria Dugesia (=Planaria ) Free-living, anatomy, X-section Bdelloura horseshoe crab gills Class Monogenea Gyrodactylus , Neobenedenis, Ergocotyle gills of freshwater fish Neopolystoma urinary bladder of turtles Class Trematoda ( Flukes ) Subclass Digenea Life-cycle stages: Recognize miracidia, sporocyst, redia, cercaria , metacercaria, adults & anatomy, model Order ?? Hirudinella ventricosa wahoo stomach Nasitrema nasal cavity of bottlenose dolphin Order Strigeiformes Family Schistosomatidae Schistosoma japonicum adults, male & female, liver granuloma & healthy liver, ova, cercariae, no metacercariae, adults in mesenteric intestinal veins Order Echinostomatiformes Family Fasciolidae Fasciola hepatica sheep & human liver, liver fluke Order Plagiorchiformes Family Dicrocoeliidae Dicrocoelium & Eurytrema Cure for All Diseases by Hulda Clark, Paragonimus -

Angiostrongylus Cantonensis: a Review of Its Distribution, Molecular Biology and Clinical Significance As a Human
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/303551798 Angiostrongylus cantonensis: A review of its distribution, molecular biology and clinical significance as a human... Article in Parasitology · May 2016 DOI: 10.1017/S0031182016000652 CITATIONS READS 4 360 10 authors, including: Indy Sandaradura Richard Malik Centre for Infectious Diseases and Microbiolo… University of Sydney 10 PUBLICATIONS 27 CITATIONS 522 PUBLICATIONS 6,546 CITATIONS SEE PROFILE SEE PROFILE Derek Spielman Rogan Lee University of Sydney The New South Wales Department of Health 34 PUBLICATIONS 892 CITATIONS 60 PUBLICATIONS 669 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Create new project "The protective rate of the feline immunodeficiency virus vaccine: An Australian field study" View project Comparison of three feline leukaemia virus (FeLV) point-of-care antigen test kits using blood and saliva View project All content following this page was uploaded by Indy Sandaradura on 30 May 2016. The user has requested enhancement of the downloaded file. All in-text references underlined in blue are added to the original document and are linked to publications on ResearchGate, letting you access and read them immediately. 1 Angiostrongylus cantonensis: a review of its distribution, molecular biology and clinical significance as a human pathogen JOEL BARRATT1,2*†, DOUGLAS CHAN1,2,3†, INDY SANDARADURA3,4, RICHARD MALIK5, DEREK SPIELMAN6,ROGANLEE7, DEBORAH MARRIOTT3, JOHN HARKNESS3, JOHN ELLIS2 and DAMIEN STARK3 1 i3 Institute, University of Technology Sydney, Ultimo, NSW, Australia 2 School of Life Sciences, University of Technology Sydney, Ultimo, NSW, Australia 3 Department of Microbiology, SydPath, St.