Controlling Disease Due to Helminth Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Full Text in Pdf Format
DISEASES OF AQUATIC ORGANISMS Published July 30 Dis Aquat Org Oral pharmacological treatments for parasitic diseases of rainbow trout Oncorhynchus mykiss. 11: Gyrodactylus sp. J. L. Tojo*, M. T. Santamarina Department of Microbiology and Parasitology, Laboratory of Parasitology, Faculty of Pharmacy, Universidad de Santiago de Compostela, E-15706 Santiago de Compostela, Spain ABSTRACT: A total of 24 drugs were evaluated as regards their efficacy for oral treatment of gyro- dactylosis in rainbow trout Oncorhj~nchusmykiss. In preliminary trials, all drugs were supplied to infected fish at 40 g per kg of feed for 10 d. Twenty-two of the drugs tested (aminosidine, amprolium, benznidazole, b~thionol,chloroquine, diethylcarbamazine, flubendazole, levamisole, mebendazole, n~etronidazole,mclosamide, nitroxynil, oxibendazole, parbendazole, piperazine, praziquantel, roni- dazole, secnidazole, tetramisole, thiophanate, toltrazuril and trichlorfon) were ineffective Triclabenda- zole and nitroscanate completely eliminated the infection. Triclabendazole was effective only at the screening dosage (40 g per kg of feed for 10 d), while nitroscanate was effective at dosages as low as 0.6 g per kg of feed for 1 d. KEY WORDS: Gyrodactylosis . Rainbow trout Treatment. Drugs INTRODUCTION to the hooks of the opisthohaptor or to ulceration as a result of feeding by the parasite. The latter is the most The monogenean genus Gyrodactylus is widespread, serious. though some individual species have a restricted distri- Transmission takes place largely as a result of direct bution. Gyrodactyloses affect numerous freshwater contact between live fishes, though other pathways species including salmonids, cyprinids and ornamen- (contact between a live fish and a dead fish, or with tal fishes, as well as marine fishes including gadids, free-living parasites present in the substrate, or with pleuronectids and gobiids. -

The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca Volvulus Excretory Secretory Products
pathogens Review The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca volvulus Excretory Secretory Products Luc Vanhamme 1,*, Jacob Souopgui 1 , Stephen Ghogomu 2 and Ferdinand Ngale Njume 1,2 1 Department of Molecular Biology, Institute of Biology and Molecular Medicine, IBMM, Université Libre de Bruxelles, Rue des Professeurs Jeener et Brachet 12, 6041 Gosselies, Belgium; [email protected] (J.S.); [email protected] (F.N.N.) 2 Molecular and Cell Biology Laboratory, Biotechnology Unit, University of Buea, Buea P.O Box 63, Cameroon; [email protected] * Correspondence: [email protected] Received: 28 October 2020; Accepted: 18 November 2020; Published: 23 November 2020 Abstract: Nematodes constitute a very successful phylum, especially in terms of parasitism. Inside their mammalian hosts, parasitic nematodes mainly dwell in the digestive tract (geohelminths) or in the vascular system (filariae). One of their main characteristics is their long sojourn inside the body where they are accessible to the immune system. Several strategies are used by parasites in order to counteract the immune attacks. One of them is the expression of molecules interfering with the function of the immune system. Excretory-secretory products (ESPs) pertain to this category. This is, however, not their only biological function, as they seem also involved in other mechanisms such as pathogenicity or parasitic cycle (molting, for example). Wewill mainly focus on filariae ESPs with an emphasis on data available regarding Onchocerca volvulus, but we will also refer to a few relevant/illustrative examples related to other worm categories when necessary (geohelminth nematodes, trematodes or cestodes). -
Comparative Efficacies of Commercially Available Benzimidazoles Against Pseudodactylogyrus Infestations in Eels
DISEASES OF AQUATIC ORGANISMS Published October 4 Dis. aquat. Org. l Comparative efficacies of commercially available benzimidazoles against Pseudodactylogyrus infestations in eels ' Department of Fish Diseases, Royal Veterinary and Agricultural University, 13 Biilowsvej, DK-1870 Frederiksberg C, Denmark Department of Pharmacy, Royal Veterinary and Agricultural University, 13 Biilowsvej. DK-1870 Frederiksberg C,Denmark ABSTRACT: The antiparasitic efficacies of 9 benzimidazoles in commercially avalable formulations were tested (water bath treatments) on small pigmented eels Anguilla anguilla, expenmentally infected by 30 to 140 specimens of Pseudodactylogyrus spp. (Monogenea).Exposure time was 24 h and eels were examined 4 to 5 d post treatment. Mebendazole (Vermox; 1 mg 1-') eradicated all parasites, whereas luxabendazole (pure substance) and albendazole (Valbazen) were 100 % effective only at a concen- tration of 10 mg I-'. Flubendazole (Flubenol), fenbendazole (Panacur) and oxibendazole (Lodltac) (10 mg l-') caused a reduction of the infection level to a larger extent than did triclabendazole (Fasinex) and parbendazole (Helmatac).Thiabendazole (Equizole), even at a concentration as high as 100 mg l-', was without effect on Pseudodactylogyrus spp. INTRODUCTION range of commercially available benzimidazole com- pounds. If drug resistance will develop under practical The broad spectrum anthelmintic drug mebendazoIe eel-farm conditions in the future, it is likely to be was reported as an efficacious compound against infes- recognized during treatments with commercially avail- tations of the European eel Anguilla anguilla with gill able drug formulations. Therefore this type of drug parasitic monogeneans of the genus Pseudodactylo- preparations were used in the present study. gyms (Szekely & Molnar 1987, Buchmann & Bjerre- gaard 1989, 1990, Mellergaard 1989). -

84364615004.Pdf
Biomédica ISSN: 0120-4157 ISSN: 2590-7379 Instituto Nacional de Salud Bolaños, Fernando; Jurado, Leonardo F.; Luna-Tavera, Rina L.; Jiménez, Jaime M. Abdominal angiostrongyliasis, report of two cases and analysis of published reports from Colombia Biomédica, vol. 40, no. 2, 2020, pp. 233-242 Instituto Nacional de Salud DOI: 10.7705/biomedica.5043 Available in: http://www.redalyc.org/articulo.oa?id=84364615004 How to cite Complete issue Scientific Information System Redalyc More information about this article Network of Scientific Journals from Latin America and the Caribbean, Spain and Journal's webpage in redalyc.org Portugal Project academic non-profit, developed under the open access initiative Biomédica 2020;40:233-42 Abdominal angiostrongyliasis in Colombia doi: https://doi.org/10.7705/biomedica.5043 Case report Abdominal angiostrongyliasis, report of two cases and analysis of published reports from Colombia Fernando Bolaños1,2, Leonardo F. Jurado3,4,5, Rina L. Luna-Tavera1, Jaime M. Jiménez1 1 Departamento de Patología, Hospital Universitario Hernando Moncaleano Perdomo, Neiva, Colombia 2 Departamento de Patología, Hospital Universitario Departamental de Nariño, Pasto, Colombia 3 Departamento de Patología y Laboratorios, Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá, D.C., Colombia 4 Departamento de Microbiología, Facultad de Medicina, Universidad Nacional de Colombia, Bogotá, D.C., Colombia 5 Facultad de Medicina, Fundación Universitaria Sanitas, Bogotá, D.C., Colombia Abdominal angiostrongyliasis is a parasitic zoonosis, endemic in the American continent. Its etiological agent is Angiostrongylus costaricensis, a nematode whose definitive hosts are rats and other rodents and the intermediate hosts, slugs. Mammals acquire the infection by consuming vegetables contaminated with L3 larvae. -

Comparison Laboratory Methods for Detection of Hookworms Infection
Advances in Health Sciences Research, volume 1 1st Public Health International Conference (PHICo 2016) Comparison Laboratory Methods for Detection of Hookworms Infection Merina Panggabean1, Lambok Siahaan2, Yoan Carolina Panggabean3 1.2.3Department of Parasitology, Faculty of Medicine, University Sumatera Utara, Indonesia [email protected] [email protected] [email protected] Abstract— Intestinal parasitic infections are globally endemic in transmitted Helminths (STH) or worms are the world. In Indonesia, intestinal parasitic infections transmitted through by the soil. They are particularly helminthes is one of the public health problems. It can cause malnutrition and anemia so can be disturbing growth transmitted by eggs present in human faeces which and development children. Intestinal parasitic infections with in turn contaminate soil [1]. STH infections belong soil-transmitted helminths (STH) such as Ascaris lumbricoides, to the neglected tropical diseases (NTDs) that affect Trichuris trichiura and hookworms (Necator americanus and Ancylostoma duodenale) diagnosed by detection of helminth eggs human populations in poorer regions of the world in stool samples. Stool samples commonly examine by using [4]. Their presence is a typical marker of poverty microscopic with conventional techniques as direct wet smear where access to sanitation and clean water is limited stain like Lugol stain, sedimentation methods like formol ether concentration (FEC). Stool examination for hookworm with and, concomitantly, standards of hygiene are low conventional techniques often miss opportunity in laboratory. [5]–[7]. There are four main species of STH; Therefore we used modified Harada Mori culture to detect namely, Ascaris lumbricoides (roundworm), hookworms infection. The objective of this study was to compare modified Harada Mori culture method and others laboratory Trichuris trichiura (whipworm) and the methods like direct wet smear Lugol stain and FEC to detect hookworms (Ancylostoma duodenale and Necator hookworm infections. -

Hookworm (Ancylostomiasis)
Hookworm (ancylostomiasis) Hookworm (ancylostomiasis) rev Jan 2018 BASIC EPIDEMIOLOGY Infectious Agent Hookworm is a soil transmitted helminth. Human infections are caused by the nematode parasites Necator americanus and Ancylostoma duodenale. Transmission Transmission primarily occurs via direct contact with fecal contaminated soil. Soil becomes contaminated with eggs shed in the feces of an individual infected with hookworm. The eggs must incubate in the soil for several days before they become infectious and are able to be transmitted to another person. Oral transmission can sometimes occur from consuming improperly washed food grown or exposed to fecal contaminated soil. Transmission can also occur (rarely) between a mother and her fetus/infant via infected placental or mammary tissue. Incubation Period Eggs must incubate in the soil for 5-10 days before they mature into infectious filariform larvae that can penetrate the skin. Within the first 10 days following penetration of the skin filariform larvae will migrate to the lungs and occasionally cause respiratory symptoms. Three to five weeks after skin penetration the larvae will migrate to the intestinal tract where they will mature into an adult worm. Adult worms may live in the intestine for 1-5 years depending on the species. Communicability Human to human transmission of hookworm does NOT occur because part of the worm’s life cycle must be completed in soil before becoming infectious. However, vertical transmission of dormant filariform larvae can occur between a mother and neonate via contaminated breast milk. These dormant filariform larvae can remain within in a host for months to years. Soil contamination is perpetuated by fecal contamination from infected individuals who can shed eggs in feces for several years after infection. -

Taenia Solium Transmission in a Rural Community in ·Honduras: an Examination of Risk Factors and Knowledge
Taenia solium Transmission in a Rural Community in ·Honduras: An Examination of Risk Factors and Knowledge by Haiyan Pang Faculty of Applied Health Sciences Brock University A thesis submitted for completion of the Master of Science Degree Haiyan Pang © 2004 lAMES A GIBSON LIBRARY . BROCK UNIVERSITY sr. CAtHARINES· ON Abstract Taenia soliurn taeniasis and cysticercosis are recognized as a major public health problem in Latin America. T. soliurn transmission not only affects the health of the individual, but also social and economic development, perpetuating the cycle of poverty. To determine prevalence rates, population knowledge and risk factors associated with transmission, anepidemiological study was undertaken in the rural community of Jalaca. Two standardized questionnaires were used to collect epidemiological and T. soli urn general knowledge data. Kato-Katz technique and an immunoblot assay (EITB) were used to determine taeniasis and seroprevalence, respectively. In total, 139 individuals belonging to 56 households participated in the study. Household characteristics were consistent with conditions of poverty of rural Honduras: 21.4% had no toilet or latrines, 19.6% had earthen floor, and 51.8% lacked indoor tap water. Pigs were raised in 46.4% of households, of which 70% allowed their pigs roaming freely. A human seroprevalence rate of 18.7% and a taeniasis prevalence rate of 2.4% were found. Only four persons answered correctly 2: 6 out of ten T. soliurn knowledge questions, for an average passing score of 2.9%. In general, a serious gap exists in knowledge regarding how humans acquire the infections, especially neurocysticercosis was identified. After regression analysis, the ability to recognize adult tapeworms and awareness of the clinical importance of taeniasis, were found to be significant risk factors for T. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -
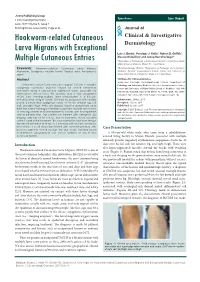
Hookworm-Related Cutaneous Larva Migrans with Exceptional Multiple Cutaneous Entries
Open Access Case Report J Clin Investigat Dermatol June 2017 Volume 5, Issue 1 © All rights are reserved by Vega et al. Journal of Hookworm-related Cutaneous Clinical & Investigative Larva Migrans with Exceptional Dermatology Luis J. Borda1, Penelope J. Kallis1, Robert D. Griffith1, Alessio Giubellino1 and Jeong Hee Cho-Vega2* Multiple Cutaneous Entries 1Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL, United States Keywords: Hookworm-related Cutaneous Larva Migrans; 2Dermatopathology Division, Department of Pathology and Laboratory Hookworm; Serpiginous multiple tracks; Tropical area; Anti-parasite Medicine, Sylvester Comprehensive Cancer Center and University of agent Miami Miller School of Medicine, Miami, FL, United States Abstract *Address for Correspondence Jeong Hee Cho-Vega, Dermatopathology Division, Department of Hookworm-related Cutaneous Larva Migrans (HrCLM) is a pruritic Pathology and Laboratory Medicine Sylvester Comprehensive Cancer serpiginous cutaneous eruption caused by animal hookworms Center and University of Miami Miller School of Medicine 1120 NW commonly found in tropical and subtropical areas, especially the 14th Street, Holtz ET, Suite 2146 Miami, FL 33136, USA, Tel: (305)- Southeastern United States. We describe here a very exceptional 243-6433; Fax: (305)-243-1624; E-mail: [email protected] HrCLM case showing multiple larva entries/lesions in a 63-year- old white male living in Miami. Clinically he presented with multiple Submission: 25 May, 2017 pruritic erythematous serpiginous tracks on his left anterior leg, left Accepted: 15 June, 2017 calf, and right thigh. While skin biopsies failed to demonstrate larva Published: 22 June, 2017 itself, the overall histological features supported multiple larva tracks Copyright: © 2017 Borda LJ, et al. -

Visceral and Cutaneous Larva Migrans PAUL C
Visceral and Cutaneous Larva Migrans PAUL C. BEAVER, Ph.D. AMONG ANIMALS in general there is a In the development of our concepts of larva II. wide variety of parasitic infections in migrans there have been four major steps. The which larval stages migrate through and some¬ first, of course, was the discovery by Kirby- times later reside in the tissues of the host with¬ Smith and his associates some 30 years ago of out developing into fully mature adults. When nematode larvae in the skin of patients with such parasites are found in human hosts, the creeping eruption in Jacksonville, Fla. (6). infection may be referred to as larva migrans This was followed immediately by experi¬ although definition of this term is becoming mental proof by numerous workers that the increasingly difficult. The organisms impli¬ larvae of A. braziliense readily penetrate the cated in infections of this type include certain human skin and produce severe, typical creep¬ species of arthropods, flatworms, and nema¬ ing eruption. todes, but more especially the nematodes. From a practical point of view these demon¬ As generally used, the term larva migrans strations were perhaps too conclusive in that refers particularly to the migration of dog and they encouraged the impression that A. brazil¬ cat hookworm larvae in the human skin (cu¬ iense was the only cause of creeping eruption, taneous larva migrans or creeping eruption) and detracted from equally conclusive demon¬ and the migration of dog and cat ascarids in strations that other species of nematode larvae the viscera (visceral larva migrans). In a still have the ability to produce similarly the pro¬ more restricted sense, the terms cutaneous larva gressive linear lesions characteristic of creep¬ migrans and visceral larva migrans are some¬ ing eruption. -

Pathophysiology and Gastrointestinal Impacts of Parasitic Helminths in Human Being
Research and Reviews on Healthcare: Open Access Journal DOI: 10.32474/RRHOAJ.2020.06.000226 ISSN: 2637-6679 Research Article Pathophysiology and Gastrointestinal Impacts of Parasitic Helminths in Human Being Firew Admasu Hailu1*, Geremew Tafesse1 and Tsion Admasu Hailu2 1Dilla University, College of Natural and Computational Sciences, Department of Biology, Dilla, Ethiopia 2Addis Ababa Medical and Business College, Addis Ababa, Ethiopia *Corresponding author: Firew Admasu Hailu, Dilla University, College of Natural and Computational Sciences, Department of Biology, Dilla, Ethiopia Received: November 05, 2020 Published: November 20, 2020 Abstract Introduction: This study mainly focus on the major pathologic manifestations of human gastrointestinal impacts of parasitic worms. Background: Helminthes and protozoan are human parasites that can infect gastrointestinal tract of humans beings and reside in intestinal wall. Protozoans are one celled microscopic, able to multiply in humans, contributes to their survival, permits serious infections, use one of the four main modes of transmission (direct, fecal-oral, vector-borne, and predator-prey) and also helminthes are necked multicellular organisms, referred as intestinal worms even though not all helminthes reside in intestines. However, in their adult form, helminthes cannot multiply in humans and able to survive in mammalian host for many years due to their ability to manipulate immune response. Objectives: The objectives of this study is to assess the main pathophysiology and gastrointestinal impacts of parasitic worms in human being. Methods: Both primary and secondary data were collected using direct observation, books and articles, and also analyzed quantitativelyResults and and conclusion: qualitatively Parasites following are standard organisms scientific living temporarily methods. in or on other organisms called host like human and other animals. -

Infestation in a Central Nigerian Rural Community * ANOSIKE, JC
J. Appl. Sci. Environ. Mgt. June, 2006 JASEM ISSN 1119-8362 Full-text Available Online at All rights reserved www.bioline.org.br/ja Vol. 10 (2) 61 - 66 Studies on the Intestinal Worm (Helminthiasis) infestation in a Central Nigerian Rural Community *1ANOSIKE, JC; 1ZACCHEAUS, VO; 1ADEIYONGO, CM; 2ABANOBI, OC; 1DADA, EO; 3OKU, EE; 1KEKE, IR; 4UWAEZUOKE, JC; 4AMAJUOYI, OU; 5OBIUKWU, CE; 4NWOSU, DC; 4OGBUSU, FI 1Department of Zoology, University of Jos P.M.B. 2084, Jos, Plateau State, Nigeria 2Department of Community Medicine, College of Medicine and Health Sciences, Abia State, University, Uturu, Nigeria 3Department of Biological Sciences, University of Calabar, Nigeria 4Department of Animal & Environmental Biology, Imo State University, Owerri, Nigeria. 5Department of Industrial Microbiology, Imo State University, Owerri, Nigeria. E-mail: [email protected] ABSTRACT: The prevalence of intestinal helminth of residents of Naraguta rural community in Central Nigeria is presented. Out of 700 stool specimens examined between January and July 1999, 261 (37.3%) were positive for helminthic infections. Helminths encountered include Hookworm, Schistosoma mansoni, Trichuris trichiura, Strongyloides stercoralis, Ascaris lumbricoides, and Hymenolepis nana. Hookworm was the most predominant, followed by S. stercoralis, S. mansoni and A. lumbricoides with T. trichiura as the least. Intestinal helminthiasis was equally prevalent for males and females. However, infection rates were high among persons below ten years of age, in toddlers, housewives and farmers than others. Persons defecating in the bush harbored more worms (56.7%) than pit latrine users (43.3%). Free medical diagnosis in most rural communities in Nigeria are probably justifiable and should be promoted and/or sustained by government.