Defining Lipid Mediators of Insulin Resistance: Controversies and Challenges
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
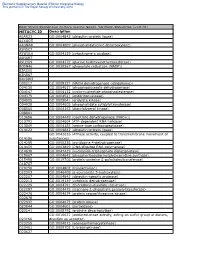
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

I HIGH MASS ACCURACY COUPLED to SPATIALLY-DIRECTED
HIGH MASS ACCURACY COUPLED TO SPATIALLY-DIRECTED PROTEOMICS FOR IMPROVED PROTEIN IDENTIFICATIONS IN IMAGING MASS SPECTROMETRY EXPERIMENTS By David Geoffrey Rizzo Dissertation Submitted to the Faculty of the Graduate School of Vanderbilt University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in Chemistry August, 2016 Nashville, Tennessee Approved: Richard M. Caprioli, Ph.D. Kevin L. Schey, Ph.D. John A. McLean, Ph.D. Michael P. Stone, Ph.D. i Copyright © 2016 by David Geoffrey Rizzo All Rights Reserved ii This work is dedicated to my family and friends, who have shown nothing but support for me in all of life’s endeavors. iii ACKNOWLEDGEMENTS “As we express our gratitude, we must never forget that the highest appreciation is not to utter words, but to live by them.” - John F. Kennedy – There are many people I must thank for showing kindness, encouragement, and support for me during my tenure as a graduate student. First and foremost, I would like to thank my research advisor, Richard Caprioli, for providing both ample resources and guidance that allowed me to grow as a scientist. Our discussions about my research and science in general have helped me become a much more focused and discerning analytical chemist. I must also thank my Ph.D. committee members, Drs. Kevin Schey, John McLean, and Michael Stone, who have brought valuable insight into my research and provided direction along the way. My undergraduate advisor, Dr. Facundo Fernández, encouraged me to begin research in his lab and introduced me to the world of mass spectrometry. -

Negative Regulation of Diacylglycerol Kinase &Theta
Cell Death and Differentiation (2010) 17, 1059–1068 & 2010 Macmillan Publishers Limited All rights reserved 1350-9047/10 $32.00 www.nature.com/cdd Negative regulation of diacylglycerol kinase h mediates adenosine-dependent hepatocyte preconditioning G Baldanzi1,5, E Alchera2,5, C Imarisio2, M Gaggianesi1, C Dal Ponte2, M Nitti3, C Domenicotti3, WJ van Blitterswijk4, E Albano2, A Graziani1,5 and R Carini*,2,5 In liver ischemic preconditioning (IP), stimulation of adenosine A2a receptors (A2aR) prevents ischemia/reperfusion injury by promoting diacylglycerol-mediated activation of protein kinase C (PKC). By concerting diacylglycerol to phosphatidic acid, diacylglycerol kinases (DGKs) act as terminator of diacylglycerol signalling. This study investigates the role of DGK in the development of hepatocyte IP. DGK activity and cell viability were evaluated in isolated rat hepatocytes preconditioned by 10 min hypoxia followed by 10 min re-oxygenation or by the treatment with the A2aR agonist, CGS21680, and subsequently exposed to prolonged hypoxia. We observed that after IP or A2aR activation, a decrease in DGK activity was associated with the onset of hepatocyte tolerance to hypoxia. CGS21680-induced stimulation of A2aR specifically inhibited DGK isoform h by activating RhoA–GTPase. Consistently, both siRNA-mediated downregulation of DGK h and hepatocyte pretreatment with the DGK inhibitor R59949 induced cell tolerance to hypoxia. The pharmacological inhibition of DGK was associated with the diacylglycerol- dependent activation of PKC d and e and of their downstream target p38 MAPK. In conclusion, we unveil a novel signalling pathway contributing to the onset of hepatocyte preconditioning, which through RhoA–GTPase, couples A2aR to the downregulation of DGK. -

TITLE PAGE Oxidative Stress and Response to Thymidylate Synthase
Downloaded from molpharm.aspetjournals.org at ASPET Journals on October 2, 2021 -Targeted -Targeted 1 , University of of , University SC K.W.B., South Columbia, (U.O., Carolina, This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. -

Domains, Amino Acid Residues, and New Isoforms of Caenorhabditis Elegans Diacylglycerol Kinase 1 (DGK-1) Important for Terminating Diacylglycerol Signaling in Vivo*□S
Supplemental Material can be found at: http://www.jbc.org/content/suppl/2004/12/06/M409460200.DC1.html THE JOURNAL OF BIOLOGICAL CHEMISTRY Vol. 280, No. 4, Issue of January 28, pp. 2730–2736, 2005 © 2005 by The American Society for Biochemistry and Molecular Biology, Inc. Printed in U.S.A. Domains, Amino Acid Residues, and New Isoforms of Caenorhabditis elegans Diacylglycerol Kinase 1 (DGK-1) Important for Terminating Diacylglycerol Signaling in Vivo*□S Received for publication, August 17, 2004, and in revised form, November 22, 2004 Published, JBC Papers in Press, November 24, 2004, DOI 10.1074/jbc.M409460200 Antony M. Jose‡ and Michael R. Koelle§¶ From the ‡Departments of Molecular, Cellular, and Developmental Biology and §Molecular Biophysics and Biochemistry, Yale University School of Medicine, New Haven, Connecticut 06520 Diacylglycerol kinases (DGKs) inhibit diacylglycerol numerous cellular processes mediated by neurotransmitters, (DAG) signaling by phosphorylating DAG. DGK-1, the growth factors, and hormones (3). DAG also activates the syn- Caenorhabditis elegans ortholog of human neuronal aptic vesicle priming protein UNC-13 (4, 5) to control neuro- DGK, inhibits neurotransmission to control behavior. transmission and certain transient receptor potential cation Downloaded from DGK-1, like DGK, has three cysteine-rich domains channels (6). In humans, nine DGK isozymes have been iden- (CRDs), a pleckstrin homology domain, and a kinase tified (DGK␣, , ␥, ␦, , ⑀, , , and ), but their physiological domain. To identify DGK domains and amino acid resi- functions remain largely unknown (1, 2). dues critical for terminating DAG signaling in vivo,we C. elegans DGK-1 provides a genetically tractable model for analyzed 20 dgk-1 mutants defective in DGK-1-con- elucidating the physiological functions of diacylglycerol ki- trolled behaviors. -

Lipid Rafts Activation of a Neutral Sphingomyelinase in T Cells by + and Proliferation of Human CD4 Cholera Toxin B-Subunit Prev
Cholera Toxin B-Subunit Prevents Activation and Proliferation of Human CD4 + T Cells by Activation of a Neutral Sphingomyelinase in Lipid Rafts This information is current as of October 1, 2021. Alexandre K. Rouquette-Jazdanian, Arnaud Foussat, Laurence Lamy, Claudette Pelassy, Patricia Lagadec, Jean-Philippe Breittmayer and Claude Aussel J Immunol 2005; 175:5637-5648; ; doi: 10.4049/jimmunol.175.9.5637 Downloaded from http://www.jimmunol.org/content/175/9/5637 References This article cites 55 articles, 31 of which you can access for free at: http://www.jimmunol.org/content/175/9/5637.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on October 1, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2005 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Cholera Toxin B-Subunit Prevents Activation and Proliferation of Human CD4؉ T Cells by Activation of a Neutral Sphingomyelinase in Lipid Rafts1 Alexandre K. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Thesis Template
An In Vivo Screen for Genes Involved in Central Nervous System Control of Obesity Identifies Diacylglycerol Kinase as a Regulator of Insulin Secretion by Irene Trinh A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Department of Molecular Genetics University of Toronto © Copyright by Irene Trinh, 2017. An In Vivo Screen for Genes Involved in Central Nervous System Control of Obesity Identifies Diacylglycerol Kinase as a Regulator of Insulin Secretion Irene Trinh Doctor of Philosophy Department of Molecular Genetics University of Toronto 2017 Abstract The increasing prevalence of obesity as well as its association with many chronic diseases has turned obesity into a major health concern worldwide. Obesity has many underlying environmental and genetic factors that disturb the balance between energy intake and energy expenditure, which is controlled by the central nervous system. The goal of my project is to help further our understanding of these CNS mechanisms by using the powerful tools available in Drosophila melanogaster to identify neuronal genes involved in energy homeostasis. Using the neuronal fru-Gal4 driver we performed an RNAi screen with 1748 genes and assayed for obese or lean phenotypes defined as increases or decreases in triacylglycerol (TAG) levels. After 3 rounds of screening I identified 25 hits that were reproducible and confirmed these phenotypes with independent RNAi lines. ii One of these hits was Diacylglycerol kinase (Dgk) whose mammalian homologues have been implicated in genome-wide association studies for metabolic defects. Manipulation of neuronal Dgk levels affects TAG and carbohydrate levels but these effects don’t seem to be mediated through Dgk’s regulation of DAG, PA levels or PKC activity. -
Building a Metabolic Bridge Between Glycolysis and Sphingolipid Biosynthesis : Implications in Cancer
University of Louisville ThinkIR: The University of Louisville's Institutional Repository Electronic Theses and Dissertations 8-2014 Building a metabolic bridge between glycolysis and sphingolipid biosynthesis : implications in cancer. Morgan L. Stathem University of Louisville Follow this and additional works at: https://ir.library.louisville.edu/etd Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Stathem, Morgan L., "Building a metabolic bridge between glycolysis and sphingolipid biosynthesis : implications in cancer." (2014). Electronic Theses and Dissertations. Paper 1374. https://doi.org/10.18297/etd/1374 This Master's Thesis is brought to you for free and open access by ThinkIR: The nivU ersity of Louisville's Institutional Repository. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of ThinkIR: The nivU ersity of Louisville's Institutional Repository. This title appears here courtesy of the author, who has retained all other copyrights. For more information, please contact [email protected]. BUILDING A METABOLIC BRIDGE BETWEEN GLYCOLYSIS AND SPHINGOLIPID BIOSYNTHESIS: IMPLICATIONS IN CANCER By Morgan L. Stathem B.S., University of Georgia, 2010 A Thesis Submitted to the Faculty of the School of Medicine of the University of Louisville In Partial Fulfillment of the Requirements for the Degree of Master of Science Department of Pharmacology and Toxicology University of Louisville Louisville, KY August 2014 BUILDING A METABOLIC BRIDGE BETWEEN GLYCOLYSIS AND SPHINGOLIPID BIOSYNTHESIS: IMPLICATIONS IN CANCER By Morgan L. Stathem B.S., University of Georgia, 2010 Thesis Approved on 08/07/2014 by the following Thesis Committee: __________________________________ Leah Siskind, Ph.D. __________________________________ Levi Beverly, Ph.D. -

Regulation of Whole-Body Glucose and Lipid Metabolism by Skeletal Muscle
From the DEPARTMENT OF MOLECULAR MEDICINE AND SURGERY Karolinska Institutet, Stockholm, Sweden REGULATION OF WHOLE-BODY GLUCOSE AND LIPID METABOLISM BY SKELETAL MUSCLE Milena Schönke Stockholm 2018 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by E-Print AB Cover art “Tribute”: Jeffrey B. Bolstad © Milena Schönke, 2018 ISBN 978-91-7676-971-3 Department of Molecular Medicine and Surgery Regulation of whole-body glucose and lipid metabolism by skeletal muscle Thesis for doctoral degree (Ph.D.) By Milena Schönke Defended on Friday the 9th of March 2018, 1:00 pm Hillarpsalen, Retzius väg 8, Solna Principal Supervisor: Opponent: Professor Juleen R. Zierath Professor Antonio Vidal-Puig Karolinska Institutet University of Cambridge Department of Molecular Medicine and Surgery Wellcome Trust-MRC Institute of Metabolic Section of Integrative Physiology Science Metabolic Research Laboratories Co-Supervisor: Dr. Marie Björnholm Examination Board: Karolinska Institutet Docent Jurga Laurencikiene Department of Molecular Medicine and Surgery Karolinska Institutet Section of Integrative Physiology Department of Medicine, Huddinge Unit of Endocrinology and Diabetes Professor Elisabet Stener-Victorin Karolinska Institutet Department of Physiology and Pharmacology Division of Reproductive Endocrinology and Metabolism Professor Jan Nedergaard Stockholm University Department of Molecular Biosciences Division of Integrative Biology To my family „Am Ende des Tages muss man den Ball flach halten.” Thomas Romeiser ABSTRACT Obesity and associated diseases like type 2 diabetes are rapidly growing health concerns across the globe. The uptake and expenditure of energy in the body are tightly regulated by a plethora of enzymes and hormones in central and peripheral tissues. Skeletal muscle is an important organ in this regulatory network and exhibits remarkable flexibility with regard to fuel utilization and modulates whole-body glucose and lipid metabolism as underlined by the work presented in this thesis. -

Downloaded from NCBI (Table1)
insects Article Lipidomic Profiling Reveals Distinct Differences in Sphingolipids Metabolic Pathway between Healthy Apis cerana cerana larvae and Chinese Sacbrood Disease Xiaoqun Dang 1, Yan Li 1, Xiaoqing Li 1, Chengcheng Wang 1, Zhengang Ma 1, Linling Wang 1, Xiaodong Fan 1, Zhi Li 1, Dunyuan Huang 1, Jinshan Xu 1,* and Zeyang Zhou 1,2,3,* 1 Chongqing Key Laboratory of Vector Insect, College of Life Science, Chongqing Normal University, Chongqing 401331, China; [email protected] (X.D.); [email protected] (Y.L.); [email protected] (X.L.); [email protected] (C.W.); [email protected] (Z.M.); [email protected] (L.W.); [email protected] (X.F.); [email protected] (Z.L.); [email protected] (D.H.) 2 State Key Laboratory of Silkworm Genome Biology, College of Biotechnology, Southwest University, Chongqing 400715, China 3 Chongqing Key Laboratory of Microsporidia Infection and Control, Southwest University, Chongqing 400715, China * Correspondence: [email protected] (J.X.); [email protected] (Z.Z.) Simple Summary: Chinese Sacbrood Virus (CSBV) is one of the most destructive viruses; it causes Chinese sacbrood disease (CSD) in Apis cerana cerana, resulting in heavy economic loss. In this study, the first comprehensive analysis of the lipidome of A. c. cerana larvae-infected CSBV was performed. Viruses rely on host metabolites to infect, replicate and disseminate from several tissues. Citation: Dang, X.; Li, Y.; Li, X.; Wang, C.; Ma, Z.; Wang, L.; Fan, X.; Li, The metabolic environments play crucial roles in these processes amplification and reproduction Z.; Huang, D.; Xu, J.; et al. -

Supplementary Material Computational Prediction of SARS
Supplementary_Material Computational prediction of SARS-CoV-2 encoded miRNAs and their putative host targets Sheet_1 List of potential stem-loop structures in SARS-CoV-2 genome as predicted by VMir. Rank Name Start Apex Size Score Window Count (Absolute) Direct Orientation 1 MD13 2801 2864 125 243.8 61 2 MD62 11234 11286 101 211.4 49 4 MD136 27666 27721 104 205.6 119 5 MD108 21131 21184 110 204.7 210 9 MD132 26743 26801 119 188.9 252 19 MD56 9797 9858 128 179.1 59 26 MD139 28196 28233 72 170.4 133 28 MD16 2934 2974 76 169.9 71 43 MD103 20002 20042 80 159.3 403 46 MD6 1489 1531 86 156.7 171 51 MD17 2981 3047 131 152.8 38 87 MD4 651 692 75 140.3 46 95 MD7 1810 1872 121 137.4 58 116 MD140 28217 28252 72 133.8 62 122 MD55 9712 9758 96 132.5 49 135 MD70 13171 13219 93 130.2 131 164 MD95 18782 18820 79 124.7 184 173 MD121 24086 24135 99 123.1 45 176 MD96 19046 19086 75 123.1 179 196 MD19 3197 3236 76 120.4 49 200 MD86 17048 17083 73 119.8 428 223 MD75 14534 14600 137 117 51 228 MD50 8824 8870 94 115.8 79 234 MD129 25598 25642 89 115.6 354 Reverse Orientation 6 MR61 19088 19132 88 197.8 271 10 MR72 23563 23636 148 188.8 286 11 MR11 3775 3844 136 185.1 116 12 MR94 29532 29582 94 184.6 271 15 MR43 14973 15028 109 183.9 226 27 MR14 4160 4206 89 170 241 34 MR35 11734 11792 111 164.2 37 52 MR5 1603 1652 89 152.7 118 53 MR57 18089 18132 101 152.7 139 94 MR8 2804 2864 122 137.4 38 107 MR58 18474 18508 72 134.9 237 117 MR16 4506 4540 72 133.8 311 120 MR34 10010 10048 82 132.7 245 133 MR7 2534 2578 90 130.4 75 146 MR79 24766 24808 75 127.9 59 150 MR65 21528 21576 99 127.4 83 180 MR60 19016 19049 70 122.5 72 187 MR51 16450 16482 75 121 363 190 MR80 25687 25734 96 120.6 75 198 MR64 21507 21544 70 120.3 35 206 MR41 14500 14542 84 119.2 94 218 MR84 26840 26894 108 117.6 94 Sheet_2 List of stable stem-loop structures based on MFE.