Background Paper
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CBX Case Study
C A SE S TUDY | CROSS BORDER XPRESS (CBX) Maximizing Airport Operational Efficiency The Challenge The international border between the United States and Mexico is the most frequently crossed border in the world. In total, there are 48 U.S.-Mexico border crossings with 330 ports of entry. Cross Border Xpress (CBX) is a terminal located in San Diego, California, with a 390-foot pedestrian bridge connecting it to the Tijuana International Airport in Tijuana, Mexico. It provides easy and direct access for ticketed passengers from the U.S. side to clear Mexican immigration and catch their flight at the Tijuana airport, and for passengers arriving in Tijuana to cross into U.S. Cross Border Express at a Glance customs and exit on the U.S. side. SAFR anonymous video analytics helps improve airport operational efficiency. CBX is open 24 hours a day, and with more than a million passengers crossing each year, it is important to ensure Location: Tijuana, Mexico – both a safe and efficient passenger experience, and a San Diego, CA, USA secure border crossing. CBX needed a real-time automated solution that could count the number of Deployment Type: Anonymous video analytics people crossing, track the time it takes to cross from one Features: People counting, traversal time end of the bridge to the next, and identify any irregularity analysis, mask detection in passenger flow in order to alert security and operations personnel to potential safety problems, Use Cases: Real-time anonymous video unauthorized movement, or inefficiencies. analytics The SAFR Solution on live video feeds, in motion, under poor lighting condi- To address CBX’s need for actionable, real-time analytics, tions, and even partially obscured. -

Air Quality Planning and Transportation Conformity
Appendix C: Air Quality Planning and Transportation Conformity Draft for Public Review May 2021 Appendix C: Air Quality Planning and Transportation Conformity Executive Summary The San Diego Association of Governments (SANDAG), as the region’s Metropolitan Planning Organization (MPO), must make a transportation air quality conformity determination for regional transportation plans (RTPs) and regional transportation improvement programs (RTIPs). The purpose of transportation conformity is to ensure that federally funded or approved activities are consistent with the State Implementation Plan (SIP). This ensures that no transportation activities will cause or contribute to new air quality violations, worsen existing violations, or delay the attainment of any relevant National Ambient Air Quality Standards (NAAQS). This report documents a demonstration of conformity for the 2008 and 2015 Ozone NAAQS for San Diego Forward: The 2021 Regional Plan (2021 Regional Plan) and the 2021 Regional Transportation Improvement Program (2021 RTIP), as amended. The 2021 Regional Plan serves as the region’s Regional Transportation Plan (RTP). Background The federal Clean Air Act (CAA), which was last amended in 1990, requires the United States Environmental Protection Agency (U.S. EPA) to set NAAQS for pollutants considered harmful to public health and the environment. California has adopted state air quality standards that are more stringent than the NAAQS.1 Areas with levels that violate the standard for specified pollutants are designated as nonattainment areas. The U.S. EPA requires that each state containing nonattainment areas develop and adopt plans to attain the NAAQS by a specified attainment deadline. These attainment plans are called SIPs. The San Diego County Air Pollution Control District (SDAPCD), in collaboration with California Air Resources Board (CARB), prepares the San Diego portion of the California SIP. -
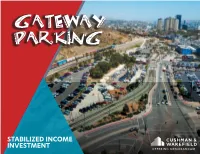
Gateway Parking
GATEWAY PARKING STABILIZED INCOME INVESTMENT OFFERING MEMORANDUM INVESTMENT ADVISORS CONFIDENTIALITY AGREEMENT JOSEPH LISING The information contained in the following offering memorandum is proprietary Managing Director and strictly confidential. It is intended to be reviewed only by the party receiving it Irvine Office from Cushman & Wakefield and it should not be made available to any other person +1 949 372 4896 Direct or entity without the written consent of Cushman & Wakefield. By taking possession +1 949 474 0405 Fax [email protected] of and reviewing the information contained herein the recipient agrees to hold and Lic. 01248258 treat all such information in the strictest confidence. The recipient further agrees that recipient will not photocopy or duplicate any part of the offering memorandum. If you have no interest in the subject property now, please return this offering memorandum to Cushman & Wakefield. This offering memorandum has been prepared to provide summary, unverified financial and physical information to prospective purchasers, and to establish only a preliminary level of interest in the subject property. The information contained herein is not a substitute for a thorough due diligence investigation. Cushman & Wakefield has not made any investigation, and makes no warranty or representation with respect to the income or expenses for the subject property, the future projected financial performance of the property, the size and square footage of the property and improvements, the presence or absence of contaminating substances, PCBs or asbestos, the compliance with local, state and federal regulations, the physical condition of the improvements thereon, or the financial condition or business prospects of any tenant, or any tenant’s plans or intentions to continue its occupancy of the subject property. -
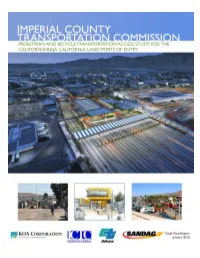
2.1 Description of Border Function
TABLE OF CONTENTS 1.0 EXECUTIVE SUMMARY 1 1.1 INTRODUCTION ..................................................................................................................................................2 1.2 COMMUNITY AND PUBLIC INVOLVEMENT .........................................................................................................4 1.3 EXISTING CONDITIONS ANALYSIS AND ASSESSMENT ......................................................................................4 1.4 PROGRAMMED IMPROVEMENTS AND FUTURE CONDITIONS .............................................................................5 1.5 ORIGIN AND DESTINATION SURVEY RESULTS ..................................................................................................5 1.6 RECOMMENDED PROJECTS .................................................................................................................................5 1.7 FUNDING STRATEGY AND VISION .....................................................................................................................7 2.0 INTRODUCTION 8 2.1 DESCRIPTION OF BORDER FUNCTION ...............................................................................................................9 2.2 DEMOGRAPHIC DATA ...................................................................................................................................... 12 2.3 CROSSING AND WAIT TIME SUMMARIES ......................................................................................................... 14 2.4 ENVIRONMENTAL, HEALTH, -

Gateway Parking
GATEWAY PARKING STABILIZED INCOME INVESTMENT OFFERING MEMORANDUM INVESTMENT ADVISORS CONFIDENTIALITY AGREEMENT JOSEPH LISING The information contained in the following offering memorandum is proprietary Managing Director and strictly confidential. It is intended to be reviewed only by the party receiving it Irvine Office from Cushman & Wakefield and it should not be made available to any other person +1 949 372 4896 Direct or entity without the written consent of Cushman & Wakefield. By taking possession +1 949 474 0405 Fax [email protected] of and reviewing the information contained herein the recipient agrees to hold and Lic. 01248258 treat all such information in the strictest confidence. The recipient further agrees that recipient will not photocopy or duplicate any part of the offering memorandum. If you have no interest in the subject property now, please return this offering memorandum to Cushman & Wakefield. This offering memorandum has been prepared to provide summary, unverified financial and physical information to prospective purchasers, and to establish only a preliminary level of interest in the subject property. The information contained herein is not a substitute for a thorough due diligence investigation. Cushman & Wakefield has not made any investigation, and makes no warranty or representation with respect to the income or expenses for the subject property, the future projected financial performance of the property, the size and square footage of the property and improvements, the presence or absence of contaminating substances, PCBs or asbestos, the compliance with local, state and federal regulations, the physical condition of the improvements thereon, or the financial condition or business prospects of any tenant, or any tenant’s plans or intentions to continue its occupancy of the subject property. -

Joint Meeting of the SANDAG Borders Committee and the Committee on Binational Regional Opportunities with the Municipalities and State Government of Baja California
Joint Meeting of the SANDAG Borders Committee and the Committee on Binational Regional Opportunities with the Municipalities and State Government of Baja California Friday, February 28, 2020 Joint Meeting from 12:30 to 2:30 p.m. SANDAG Board Room 401 B Street, 7th Floor San Diego, CA 92101 Hospitality Room open from 11:30 a.m. to 12:30 p.m. in Conference Room 8A on the 8th floor Agenda Highlights • Innovation Analysis Study for the Otay Mesa East–Mesa de Otay II Port of Entry Project • Cross Border Xpress (CBX) 2020 Update • Business Improvement Districts in Baja California Please silence all electronic devices during the meeting You can listen to the Borders Committee meeting by visiting our website at sandag.org Welcome to SANDAG. Members of the public may speak to the Borders Committee (Committee) on any item at the time the Committee is considering the item. Please complete a Request to Comment form located in the lobby. Members of the public may address the Committee on any issue under the agenda item entitled Public Comments/Communications/Member Comments. Public speakers are limited to three minutes or less per person. The Committee may take action on any item appearing on the agenda. Both agenda and non-agenda comments should be sent to the Clerk of the Committee via [email protected]. Please include the meeting date, agenda item, your name, and your organization. Any comments, handouts, presentations, or other materials from the public intended for distribution at the meeting should be received by the Clerk no later than 5 p.m. -

Final Rule; Technical and Land Transportation Are Listed in 8 Amendment
75631 Rules and Regulations Federal Register Vol. 80, No. 232 Thursday, December 3, 2015 This section of the FEDERAL REGISTER Department of Homeland Security facility, CBP will provide a variety of contains regulatory documents having general where CBP officers or employees are inspection services, including applicability and legal effect, most of which assigned to accept entries of immigration services. are keyed to and codified in the Code of merchandise, clear passengers, collect The CBX facility was designed in Federal Regulations, which is published under duties, and enforce the various accordance with U.S. and international 50 titles pursuant to 44 U.S.C. 1510. provisions of the customs and security standards. It includes an The Code of Federal Regulations is sold by immigration laws, as well as other laws enclosed pedestrian walkway the Superintendent of Documents. Prices of applicable at the border. The term ‘‘port connecting the Tijuana Airport in new books are listed in the first FEDERAL of entry’’ is used in the Code of Federal Mexico to San Diego, California and a REGISTER issue of each week. Regulations (CFR) in title 19 for customs passenger terminal located in San Diego purposes and in title 8 for immigration that will be used exclusively to process purposes. Subject to certain exceptions, ticketed Tijuana Airport passengers DEPARTMENT OF HOMELAND all individuals entering the United traveling to and from the United States SECURITY States must present themselves to an via the walkway. The pedestrian immigration officer for inspection at a walkway will be accessible only for U.S. Customs and Border Protection U.S. -

Download PDF Arrow Forward
SMART BORDER COALITION™ San Diego-Tijuana MID-YEAR PROGRESS REPORT-2016 www.smartbordercoalition.com A Wall That Divides Us. A Goal to Unite Us. SMART BORDER COALITION Members of the Board 2016 Malin Burnham/Jose Larroque, Co-Chairs Jose Galicot Gaston Luken Eduardo Acosta Ted Gildred III Matt Newsome Raymundo Arnaiz Dave Hester JC Thomas Lorenzo Berho Russ Jones Mary Walshok Malin Burnham Mohammad Karbasi Steve Williams Frank Carrillo Pradeep Khosla Honorary Rafael Carrillo Pablo Koziner Jorge Astiazaran James Clark Jorge Kuri Marcela Celorio Salomon Cohen Elias Laniado Greg Cox Alberto Coppel Jose Larroque Kevin Faulconer Jose Fimbres Jeff Light William Ostick “OPPORTUNITY COMES FROM A SEAMLESS INTERNATIONAL REGION WHERE ALL CITIZENS WORK TOGETHER FOR MUTUAL ECONOMIC AND SOCIAL PROGRESS” MID-YEAR PROGRESS REPORT 2016 Secure and efficient border crossings are the primary goal of the Coalition. The Coalition works with existing stakeholders in both the public and private sectors to coordinate regional border efficiency efforts not duplicate them. Aquí Empiezan Las Patrias/The Countries Begin Here—Where the Border Meets the Pacific WHY THE BORDER MATTERS The United States is both Mexico’s largest export and largest import market. Hundreds of thousands or people cross the shared 2000-mile border daily During the time we spend on an SBC Board of Directors luncheon, the United States and Mexico will have traded more than $60 million worth of goods and services. The daily United States trade total with is Mexico is more than $1.5 billion supporting jobs in both countries. –courtesy of Consul General Will Ostick SAN DIEGO/TIJUANA BORDER ACCOMPLISHMENTS 1. -
Presentación De Powerpoint
BAJA CALIFORNIA Strategic Location Top Industrial Competitiveness International Diplomatic Support Our People World Class Infrastructure Industrial Sectors STRATEGIC LOCATION MEXICO has free trade agreements with 46 countries. BAJA CALIFORNIA is the closest Mexican State to ASIA. STRATEGIC LOCATION • Excellent access to NAFTA Market • BC shares border with California 265 Km. and Arizona, USA. Border with USA • BC is the only Mexican state bordering with California (6th economy in the world) • Los Angeles is 3 hours driving distance • Baja California is one of the MOST COMPETITIVE Mexican States 1,550 Km. Coastline Source: Center for the Continuing Study of the California Economy. DIPLOMATIC NETWORK WORLDWIDE BAJA CALIFORNIA has a broad network of international diplomatic support in more than 15 countries TOP INDUSTRIAL COMPETITIVENESS • 1st Place in Mexico with 928 foreign manufacturing companies (IMMEX). • This represent 329,840 industrial jobs. Percentage of IMMEX Companies Creation by State Baja California 23.2 What is an IMMEX Company? Nuevo León 16.1 Chihuahua 12.8 The IMMEX program (formerly Coahuila 9.9 Tamaulipas 8.7 known as “maquiladora” is an Estado de México 6.9 incentive provided by Mexico for Jalisco 6.8 Guanajuato 7.0 companies that export goods. It Sonora 5.7 Querétaro 5.4 consists of allowing a Mexican Puebla 4.7 San Luis Potosí 3.8 company to carry out “temporary” Distrito Federal 2.4 imports of production inputs and Aguascalientes 2.1 Yucatán 1.4 assets, without having to pay the Durango 1.9 Last updated: May, 2016 Veracruz 1.3 otherwise assessed V.A.T. Otras entidades 6.7 Last updated: 2018 SOURCE: INEGI TOP INDUSTRIAL COMPETITIVENESS Baja California by the numbers Last updated: Jan 2018 Economic Indicators 2016 2017 Diff. -
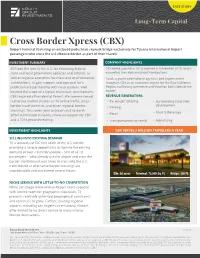
Cross Border Xpress (CBX)
CASE STUDY Long-Term Capital Cross Border Xpress (CBX) Airport terminal featuring an enclosed pedestrian skywalk bridge exclusively for Tijuana International Airport passengers who cross the U.S./Mexico border as part of their travels INVESTMENT SUMMARY COMPANY HIGHLIGHTS EGI took the lead in the U.S. for educating federal, CBX broke ground in 2014, opened in December 2015, and is state and local government agencies and officials, as exceeding user demand growth projections. well as regional economic, business and environmental Local, regional and national agencies and organizations stakeholders, to gain support and approval for a recognize CBX as an economic engine for the Baja California public/private partnership with no precedent. Well Region, facilitating commerce and travel on both sides of the beyond the scope of a typical real estate development, border. CBX required a Presidential Permit. We commissioned REVENUE GENERATORS: numerous market studies on TIJ airline traffic, cross- • Passenger ticketing • Surrounding land sale/ development border travel patterns, and other regional border • Parking crossings. This seven-year outreach and research • Food & Beverage effort culminated in nearly universal support for CBX • Retail and a 2014 groundbreaking. • Transportation/car rental • Advertising INVESTMENT HIGHLIGHTS CBX SERVES 3 MILLION TRAVELERS A YEAR SELLING INTO EXISTING DEMAND TIJ is located just 500 feet south of the U.S. border, providing a unique opportunity to tap into the existing demand of over 7.8 million people – 58% of all TIJ passengers -- who already use the airport and cross the border. Northbound wait times to cross into the U.S. from Mexico at alternative border crossings are unpredictable and can extend several hours. -

AGENDA (Representing North County Coastal)
Members John Minto, Chair Vice Mayor, City of Santee (Representing East County) Greg Cox, Vice Chair Supervisor, County of San Diego David Alvarez Councilmember, City of San Diego BORDERS John Renison Supervisor (Representing Imperial County) COMMITTEE Lorraine Wood Councilmember, City of Carlsbad AGENDA (Representing North County Coastal) Ed Gallo Councilmember, City of Escondido (Representing North County Inland) Friday, April 22, 2016 Serge Dedina 12:30 to 2:30 p.m. Mayor, City of Imperial Beach (Representing South County) SANDAG Board Room 401 B Street, 7th Floor Alternates San Diego Ruth Sterling Councilmember, City of La Mesa (Representing East County) Dianne Jacob Supervisor, County of San Diego Mark Kersey Councilmember, City of San Diego VACANT AGENDA HIGHLIGHTS (Representing Imperial County) Al Corti • SOUTH BAY RAPID UPDATE Councilmember, City of Del Mar (Representing North County Coastal) • CROSS BORDER XPRESS FACILITY Jim Cunningham Deputy Mayor, City of Poway (Representing North County Inland) • UPDATE ON IMPERIAL COUNTY BORDER Bill Sandke TRANSPORTATION PROJECTS Councilmember, City of Coronado (Representing South County) Advisory Members PLEASE SILENCE ALL ELECTRONIC DEVICES DURING THE MEETING Laurie Berman District 11 Director, Caltrans YOU CAN LISTEN TO THE BORDERS COMMITTEE Remedios Gómez-Arnau Consul General MEETING BY VISITING OUR WEBSITE AT SANDAG.ORG Consulate General of Mexico Jim Ferryman (Representing Orange County) MISSION STATEMENT Marsha Swanson The Borders Committee provides oversight for planning activities that impact the borders of the City of Wildomar San Diego region (Orange, Riverside and Imperial Counties, and the Republic of Mexico) as well as (Representing Riverside County) government-to-government relations with tribal nations in San Diego County. -

Tijuana REGIONAL PROFILE Produced by SAN DIEGO REGIONAL EDC
TIJUANA REGIONAL PROFILE ProdUced BY SAN DIEGO REGIONAL EDC TIJUANA: The largest city in the state of Baja California sits at one of busiest land border crossings in the world. Together with San Diego, Tijuana is part of LA a dynamic cross-border metropolis where deep economic and cultural linkages SD TIJUANA result in the creation of value, jobs and exports. The unique dynamics of the Ensenada region provide local companies with an important comparative advantage in the global economy. In Tijuana, employment in global companies has grown steadily, with many workers engaged in STEM and R&D-intensive industries. The city has become a powerhouse in industries such as semiconductors, medical devices, aerospace, MX electrical equipment, and audiovisual and communications equipment. Quality universities and an attractive cost of doing business have supported the development of these high-growth industries, attracting more than $5.6 billion TABle of CONteNTS of foreign direct investment to the region since 2012.1 Economic drivers 2 Talent pool 3 On average, 135,000 people cross the border each day between San Diego Tourism and quality of life 4 and Tijuana.2 Like the economy, people’s lives exist on both sides of the Global connectivity 5 border. Tijuana’s vibrant cultural scene – with trendy coffee shops, world-class Operating costs 6 restaurants, museums, art galleries and a top-ranked soccer team – provides an Regional resources and incentives 7 enriching quality of life to residents. Nearby beaches in Rosarito and Ensenada, as well as the bourgeoning Valle de Guadalupe wine region, attract tourists year- round.