Situation Report on Cholera in Zimbabwe Issue Number 10 21 January 2009
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Ports of Entry and Routes) (Amendment) Order, 2020
Statutory Instrument 55 ofS.I. 2020. 55 of 2020 Customs and Excise (Ports of Entry and Routes) (Amendment) [CAP. 23:02 Order, 2020 (No. 20) Customs and Excise (Ports of Entry and Routes) (Amendment) “THIRTEENTH SCHEDULE Order, 2020 (No. 20) CUSTOMS DRY PORTS IT is hereby notifi ed that the Minister of Finance and Economic (a) Masvingo; Development has, in terms of sections 14 and 236 of the Customs (b) Bulawayo; and Excise Act [Chapter 23:02], made the following notice:— (c) Makuti; and 1. This notice may be cited as the Customs and Excise (Ports (d) Mutare. of Entry and Routes) (Amendment) Order, 2020 (No. 20). 2. Part I (Ports of Entry) of the Customs and Excise (Ports of Entry and Routes) Order, 2002, published in Statutory Instrument 14 of 2002, hereinafter called the Order, is amended as follows— (a) by the insertion of a new section 9A after section 9 to read as follows: “Customs dry ports 9A. (1) Customs dry ports are appointed at the places indicated in the Thirteenth Schedule for the collection of revenue, the report and clearance of goods imported or exported and matters incidental thereto and the general administration of the provisions of the Act. (2) The customs dry ports set up in terms of subsection (1) are also appointed as places where the Commissioner may establish bonded warehouses for the housing of uncleared goods. The bonded warehouses may be operated by persons authorised by the Commissioner in terms of the Act, and may store and also sell the bonded goods to the general public subject to the purchasers of the said goods paying the duty due and payable on the goods. -

Status of Telecommunications Sector in Zimbabwe
TELECOMMUNICATIONS STATUS IN ZIMBABWE Sirewu Baxton [email protected] Background • Postal and Telecommunications Regulatory Authority of Zimbabwe (POTRAZ) o Established by the Postal and Telecommunications Act of 2000. o Started its operations in March 2001 o POTRAZ situated at Emerald Business Park, No. 30 The Chase Harare • Legislation brought about a new institutional framework for telecommunications: o Liberalized the sector o Introduced distinct roles of government, regulator, operators, and consumers. POTRAZ MANDATE • Ensuring provision of sufficient domestic and international telecommunication services • Ensuring provision of services at rates consistent with the provision of an efficient and continuous service • Promote the development of the sector services in accordance with: o Practicable recognised international standards o Public demand POTRAZ MANDATE cont’d • Furthers the advancement of technology • Represents Zimbabwe internationally in matters relating to the sector • Establishes, approves or controls the National Numbering plan • Manages the Radio Frequency Resource • Advises the Government on all matters relating to the telecommunication services General Country Background Location Southern Africa Area 390 590 square Km Population 12.6 Million Population Distribution 38% Urban: 62% Rural • Telecommunication service usage is mainly in urban areas. MARKET STRUCTURE FIXED • One fixed public operator (TelOne.) • Offers local, regional and international voice telephone services. • Has 337 881 subscribers (Lines) • The fixed teledensity is 2.68%. • Of these, 61 % are in the capital Harare. • 53% are residential lines. • 84 % of the lines are connected to the digital exchange. • 17 % of the lines are in rural areas. MARKET STRUCTURE MOBILE • There are three mobile operators: Econet, Net One and Telecel • The current subscriber base as at 30 June 2011 for the operators: Econet 5,521,000 Telecel 1,297,000 Net One 1,349,000 • Mobile teledensity stands at 64.85 %. -

Budiriro Mumapurazi.Pmd
FCTZ A Better Life upenyu hwakanaka Impilo Enhle Mumapurazi Budiriro Mumapurazi Quarterly Newsletter March - May 2007 Celebrating 10 years of facilitating the empowerment of vulnerable groups in farm communities WHATS INSIDE Editorial…………………………………….....................…........................Pg - 1 Your letters……………………………………….............….....................….…Pg - 2 New hope for orphans in Chihwiti…………………….…………................….Pg - 3 More food despite poor rains-case study on conservation agriculture…Pg - 4 Old but going strong- story on goat pass on scheme……….….....………..Pg - 5 Widower gives away chickens to vulnerable groups……………….......…..Pg - 6 A man who has a passion for beekeeping………………..…… …….……….…..Pg - 7 Chawasarira nutrition garden bears fruit………….……………………………....Pg - 8 Smallholder farmer dedicated to community development…………...…pg - 9 Nyanzou garden source of livelihoods for many households………………Pg - 10 Chicken pass on project helpful- says beneficiary…………….…….....…..Pg - 11 Promoting household food security, Being HIV not disability- woman………………………………………...........….Pg - 12 income and sustainable livelihoods Children's Section……………………………….…..……………….……….............Pg - 14 Anniversary theme winner……………………………………………........………….Pg - 15 WELCOME MESSAGE EDITORIAL Welcome to the March-May 2007 issue of Budiriro Mumapurazi, Farm Community The Protracted Relief Programme (PRP) Trust of Zimbabwe (FCTZ’s) Quarterly with funding from the Department for Newsletter. This edition focuses on food security, sustainable livelihoods and HIV International Development (DFID) aims and AIDS. The newsletter will publish case to assist the poorest and most vulnerable studies on the impact of the FCTZ Sustainable Livelihoods Programme. households in Zimbabwe suffering from Testimonies on HIV and AIDS, which will the effects of rainfall failures, economic also feature in the newsletter, will inform readers on how farming communities are decline and the HIV and AIDS epidemic. copying with HIV and AIDS. -

MASHONALAND EAST PROVINCE - Basemap
MASHONALAND EAST PROVINCE - Basemap Mashonaland Central Karanda Chimandau Guruve MukosaMukosa Guruve Kamusasa Karanda Marymount Matsvitsi Marymount Mary Mount Locations ShinjeShinje Horseshoe Nyamahobobo Ruyamuro RUSHINGA CentenaryDavid Nelson Nyamatikiti Nyamatikiti Province Capital Nyakapupu M a z o w e CENTENARY Mazowe St. Pius MOUNT DARWIN 2 Chipuriro Mount DarwinZRP NyanzouNyanzou Mt Darwin Chidikamwedzi Town 17 GoromonziNyahuku Tsakare GURUVE Jingamvura MAKONDE Kafura Nyamhondoro Place of Local Importance Bepura 40 Kafura Mugarakamwe Mudindo Nyamanyora Chingamuka Bure Katanya Nyamanyora Bare Chihuri Dindi ARDA Sisi Manga Dindi Goora Mission M u s e n g e z i Nyakasoro KondoKondo Zvomanyanga Goora Wa l t o n Chinehasha Madziwa Chitsungo Mine Silverside Donje Madombwe Mutepatepa Nyamaruro C o w l e y Chistungo Chisvo DenderaDendera Nyamapanda Birkdale Chimukoko Nyamapanda Chindunduma 13 Mukodzongi UMFURUDZI SAFARI AREA Madziwa Chiunye KotwaKotwa 16 Chiunye Shinga Health Facility Nyakudya UZUMBA MARAMBA PFUNGWE Shinga Kotwa Nyakudya Bradley Institute Borera Kapotesa Shopo ChakondaTakawira MvurwiMvurwi Makope Raffingora Jester H y d e Maramba Ayrshire Madziwa Raffingora Mvurwi Farm Health Scheme Nyamaropa MUDZI Kasimbwi Masarakufa Boundaries Rusununguko Madziva Mine Madziwa Vanad R u y a Madziwa Masarakufa Shutu Nyamukoho P e m b i Nzvimbo M u f u r u d z i Madziva Teacher's College Vanad Nzvimbo Chidembo SHAMVA Masenda National Boundary Feock MutawatawaMutawatawa Mudzi Rosa Muswewenhede Chakonda Suswe Mutorashanga Madimutsa Chiwarira -
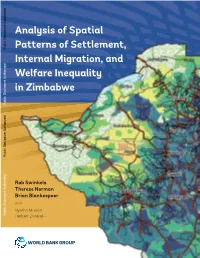
ANALYSIS of SPATIAL PATTERNS of SETTLEMENT, INTERNAL MIGRATION, and WELFARE INEQUALITY in ZIMBABWE 1 Analysis of Spatial
ANALYSIS OF SPATIAL PATTERNS OF SETTLEMENT, INTERNAL MIGRATION, AND WELFARE INEQUALITY IN ZIMBABWE 1 Analysis of Spatial Public Disclosure Authorized Patterns of Settlement, Internal Migration, and Welfare Inequality in Zimbabwe Public Disclosure Authorized Public Disclosure Authorized Rob Swinkels Therese Norman Brian Blankespoor WITH Nyasha Munditi Public Disclosure Authorized Herbert Zvirereh World Bank Group April 18, 2019 Based on ZIMSTAT data Zimbabwe District Map, 2012 Zimbabwe Altitude Map ii ANALYSIS OF SPATIAL PATTERNS OF SETTLEMENT, INTERNAL MIGRATION, AND WELFARE INEQUALITY IN ZIMBABWE TABLE OF CONTENTS ACKNOWLEDGMENTS iii ABSTRACT v EXECUTIVE SUMMARY ix ABBREVIATIONS xv 1. INTRODUCTION AND OBJECTIVES 1 2. SPATIAL ELEMENTS OF SETTLEMENT: WHERE DID PEOPLE LIVE IN 2012? 9 3. RECENT POPULATION MOVEMENTS 27 4. REASONS BEHIND THE SPATIAL SETTLEMENT PATTERN AND POPULATION MOVEMENTS 39 5. CONSEQUENCES OF THE POPULATION’S SPATIAL DISTRIBUTION 53 6. POLICY DISCUSSION 71 AREAS FOR FURTHER RESEARCH 81 REFERENCES 83 APPENDIX A. SUPPLEMENTAL MAPS AND CHARTS 87 APPENDIX B. RESULTS OF REGRESSION ANALYSIS 99 APPENDIX C. EXAMPLE OF LOCAL DEVELOPMENT INDEX 111 ACKNOWLEDGMENTS This report was prepared by a team led by Rob Swinkels, comprising Therese Norman and Brian Blankespoor. Important background work was conducted by Nyasha Munditi and Herbert Zvirereh. Wishy Chipiro provided valuable technical support. Overall guidance was provided by Andrew Dabalen, Ruth Hill, and Mukami Kariuki. Peer reviewers were Luc Christiaensen, Nagaraja Rao Harshadeep, Hans Hoogeveen, Kirsten Hommann, and Marko Kwaramba. Tawanda Chingozha commented on an earlier draft and shared the shapefiles of the Zimbabwe farmland use types. Yondela Silimela, Carli Bunding-Venter, Leslie Nii Odartey Mills, and Aiga Stokenberga provided inputs to the policy section. -

Original Research Article the Spatial Dimension of Health Service
Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2016; 4(1C):201-204 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Original Research Article The Spatial Dimension of Health Service Provision in Mashonaland West Province, Zimbabwe Takudzwa Mhandu, Dr Evans Chazireni Great Zimbabwe University, P O Box 1235, Masvingo, Zimbabwe *Corresponding author Dr Evans Chazireni Email: Abstract: Zimbabwe like many other developing countries has serious problems in its healthcare system. The quality of health service provision in Zimbabwe is generally poor Chazireni. Different parts of the country have serious healthcare problems. Mashonaland West, like other provinces in Zimbabwe, experiences numerous healthcare challenges. The research examines health service provision in Mashonaland West province in Zimbabwe. Data for this study was collected from ZIMSTAT published census reports and Ministry of health and Child Welfare published national health profiles. The analysis of the data was done through the composite index method. The calculated composite indices were used to rank the districts according to the level of health service provision. The researcher found out that there overall, the conditions of health service provision in Mashonaland West province is poor and that there are health service disparities among administrative districts in Mashonaland West province of Zimbabwe. There are many reasons which contribute to disparities in health care services at different levels (global, continental, regional, national and district level). It emerged from the research that the disparities are due to social, economic, physical and political factors. -

Annual Report 2016
ZIMBABWE NETWORK FOR HEALTH – EUROPE (ZimHealth) (RÉSEAU ZIMBABWÉEN POUR L’ACCÈS À LA SANTÉ) ANNUAL REPORT 2016 MARCH 2017 Chairperson’s Foreword This is the 9th year in the work of Zimbabwe Network for Health in its mission to support rehabilitation of public health facilities and sustain universal access and coverage with public health services based on our vision for better health for all Zimbabweans. This is my second year as chairman. I continue to provide institutional continuity required with changing ZimHealth executive. There has been need to proactively reach out to all Zimbabwean and friends of Zimbabwe who have very busy work and personal life but continue to participate in the work of the Executive, ZimHealth activities and events. In 2016, ZimHealth major project activities continued to focus on the US$1.2 million Mabvuku Polyclinic expansion in Harare City with the new construction occupation certificate provided in October 2016. This is being followed up with procurement and supply of medical equipment and recruitment and training of health staff to start theatre operations ZimHealth partnered with Ark Zimbabwe to support the rehabilitation of the floors and sluice rooms for the Mpilo Central Hospital maternity theatre and training of staff in infection control. The ZimHealth team continued to follow-up on the 24 ongoing projects with monitoring and evaluation visits to Zvamabande District Hospital-Shurugwi, Chinengundu Clinic-Chegutu, Nyamhunga Clinic - Kariba and Chikangwe Clinic- Karoi. New projects were jointly identified with Zimbabwe Association of Church Hospitals (ZACH) and some local authorities and government hospitals in 14 sites. Proposals have been developed and resource mobilization is underway. -

MAKONDE DISTRICT- Natural Farming Regions 14 February 2012
MAKONDE DISTRICT- Natural Farming Regions 14 February 2012 12 Locations Small Town Place of local Importance Mission 5 Mine Primary School ANGWA Angwa BRIDGE Clinic 3 Secondary School Health Facility 2 RUKOMECHI MANA POOLS NATIONAL Boundaries MASOKA PARK 4 Masoka MUSHUMBI Province Boundary Clinic POOLS CHEWORE MBIRE District Boundary & SAPI SAFARI AREA Ward Boundary 9 7 Transport Network 11 Major Road Secondary Road Feeder Road Connector Road ST. HURUNGWE CECELIA Track SAFARI AREA 16 Railway Line 10 Natural Farming Regions 8 1 - Specialized and diversified farming 2A - Intensive farming 2B - Intensive farming 3 - Semi-intensive farming Chundu Council 20 4 - Semi-extensive farming Clinic 8 DOMA Nyamakaze CHITINDIWA Nyama SAFARI 5 - Extensive farming Gvt Clinic Council AREA Protected Conservation Area Mashongwe SHAMROCKE 24 Council Clinic 3 Karuru 17 Council CHARARA (Construction) SAFARI VUTI AREA Dete Council Clinic RELATED FARMING SYSTEMS 9 KACHUTA 18 Region I - Specialized and Diversified Farming: Rainfall in this region is high (more than 1000mm per annum in areas lying below 1700m altitude, and more than 900mm 2 per annum at greater altitudes), normally with some precipitation in all months of the year. Kazangarare 4 Hewiyai Gvt Council Temperatures are normally comparatively low and the rainfall is consequently highly Council affective enabling afforestation, fruit and intensive livestock production to be practiced. Clinic 16 In frost-free areas plantation crops such as tea, coffee and macadamia nuts can be Lynx 1 grown, where the mean annual rainfall below 1400mm, supplementary irrigation of Clinic Private these plantation crops is required for top yields. LYNX Clinic HURUNGWE 1 23 GURUVE Region IIA - Intesive Farming : Rainfall is confined to summer and is moderately Kemutamba high (750-1000mm). -
ZIMBABWE Situation Report Last Updated: 26 Jun 2020
ZIMBABWE Situation Report Last updated: 26 Jun 2020 HIGHLIGHTS (26 Jun 2020) From 20 March to 24 June, 530 COVID-19 cases and 6 deaths were confirmed. Out of 207 cases reported in the last two weeks, 175 were among recent returnees. From 1 April to 22 June, 9,546 Zimbabwean migrants returned from neighbouring countries. As of 22 June, 2,136 returnees were quarantined in 44 centres . A decrease of admission of children for acute malnutrition treatment was recorded in April and May, with 50 per cent less children receiving vitamin A supplementation. Lawrance Njanje gives her 19-month-old son a supplement A diarrhoea outbreak was declared in Bulawayo City plumpy nut at the Tanganda Rural Health Centre, near with 1,739 cases and 9 deaths, as of 22 June. Mutare. Photo: UNICEF KEY FIGURES FUNDING (2020) CONTACTS Wouter De Cuyper 7M 5.6M $800.7M $103.1M Humanitarian Affairs Officer, Zimbabwe people in need people targeted Required Received [email protected] A S o r Guiomar Pau Sole 47 13% Communications & Information partners operational Progress Management, Regional Office for Southern & Eastern Africa [email protected] FTS: https://fts.unocha.org/appeals/9 21/summary BACKGROUND (26 Jun 2020) Situation Overview The United Nations and humanitarian partners have revised the Humanitarian Response Plan (HRP) to include response to the COVID-19 outbreak. The COVID-19 Addendum requires US$84.9 million to respond to the immediate public health crisis and the secondary impacts of the pandemic on vulnerable people, in addition to the $715 million required in the HRP. -
Covid-19 Addendum
ZIMBABWE COVID-19 ADDENDUM Part 6 COVID-19 Addendum SHAMVA DISTRICT, MASHONALAND CENTRAL PROVINCE A beneficiary washes her hands before entering a food distribution in Shamva district. Photo:WFP/Claire Nevill 46 ZIMBABWE COVID-19 ADDENDUM COVID-19 Response at a Glance PEOPLE IN NEED PEOPLE TARGETED REQUIREMENTS (US$) OPERATIONAL PARTNERS 7.5M 5.9M $84.9M 37 People in Need and Targeted Requirements by Cluster H M Me Hurungwe Cy/ Mabani M F S M U Dwin Rushinga MASHONALAND CENTRAL Karoi M Guruve Mwi M Shamva M AIBA Kariba Zvimba B Pfungwe Cyi U M Mowe MASHONALAND EAST Education Ba Moko Nth MASHONALAND WEST Nton Goromonzi HARARE Mehwa B South Sanyati C Water S U Nanga V Monder M Kadoma M Town Seke U U C H WASH U MIDLANDS Mondera MANICALAND M-N Hdweza Rusape M Lupane Kwekwe MATEBELELAND NORTH K Nyi C N U M Hwange Redcliff M U C Ba urban Gutu Me Tsholotsho B Gweru U U P BV Byo C M MASVINGO I B C M Zvishavane U B Zvishavane U Z U U M C Potection Plumtree Mengwa MATEBELELAND SOUTH 2M C C Potection U U M Mobo M Gwanda Cedzi B SM M Propor IN Targeted B P geted U R 02M People in Need and Targeted by Cluster Operational Partners by Type Water S M H WASH 2M F S 0M M NNO Education M 9 M INO H M 18 0M PBV 2M 845K PP 22M UN 22 0 MS 20M 20 0M N 353K 2 S 91K In addition to the humanitarian response requirements, R 14K $4.5 million is needed to support Governance interventions 14K dination and $22.5 million for social protection, which will be 953 M 953 carried out by development actors. -

African Traditional Cultural Values and Beliefs: a Driving Force to Natural Resource Management: a Study of Makonde District, Mashonaland West Province, Zimbabwe
Journal of Culture, Society and Development www.iiste.org ISSN 2422-8400 An International Peer-reviewed Journal Vol.9, 2015 African Traditional Cultural Values and Beliefs: A Driving Force to Natural Resource Management: A Study of Makonde District, Mashonaland West Province, Zimbabwe Sigauke,E.I; Katsaruware,D. 2; Chiridza, P. 3; Saidi,T. 4 1. Department of Geography and Environmental Studies, Zimbabwe Open University, Mashonaland West Region, Chinhoyi. 2. Department of Agricultural Management; Zimbabwe Open University; Mashonaland West Region, Chinhoyi, Zimbabwe. 3. Department of Journalism and Media Studies; Zimbabwe Open University, Mashonaland West Region, Chinhoyi, Zimbabwe. 4. Department of Technology and Society Studies, Maastricht University, Maastricht, The Netherlands. Abstract Natural resources in Africa are in jeopardy of depletion as a result of increasing demographic pressure and climate change. Sustainability of the natural resource base can be achieved through adoption of traditional cultural values and beliefs. This research was conducted in Makonde District, Mashonaland West Province of Zimbabwe. The research is qualitative in nature and employs the empirical case study research design through adopting the descriptive approach to data. The research involved description of knowledge, behaviors, perceptions and attitudes of the people in the Makonde District on cultural values and beliefs for the sustainable management of natural resources. The results of the study indicate that cultural norms and values such as totems, taboos, traditional ceremonies, and the formation of the old age group committees as well as the role of the spirit mediums have an impact of the conservation of natural resources namely tree species, water resources, forests, minerals and some sacred groves in Makonde district. -

A Survey of Communication Media Preferred by Smallholder Farmers in the Gweru District of Zimbabwe T
Journal of Rural Studies 66 (2019) 112–118 Contents lists available at ScienceDirect Journal of Rural Studies journal homepage: www.elsevier.com/locate/jrurstud A survey of communication media preferred by smallholder farmers in the Gweru District of Zimbabwe T ∗ Rachel Moyo , Abiodun Salawu Department of Communication, North West University, Private Bag X2046, Mafikeng, 2735, South Africa ARTICLE INFO ABSTRACT Keywords: This study is a quantitative survey of communication media preferred by smallholder farmers resettled under the Communication media Fast Track Land Reform Programme (FTLRP) in the Gweru district of Zimbabwe. Data were gathered using a Gweru questionnaire and simple random sampling. Communication is integral to agricultural development, particularly Productivity so in the context of the FTLRP characterised by a dearth of information, education and training, ensued by the Preference discriminatory command agriculture (Murisa and Chikweche, 2015). Farmers' preferences of communication Smallholder farming media in receiving agricultural innovations should be prioritised to improve agricultural communication and Development subsequently, productivity, which is dire in Zimbabwe in the light of the continuing food insecurity. The findings indicated that farmers prefer media that are stimulating and engaging such as television and demonstrations; convenient such as mobile phones and detailed such as books probably because the majority of them do not have training in agriculture. Demographic variables of age-group and education were found to be associated with communication preferences of some media. The study has implications for agricultural communication media policy. Beyond prioritisation of farmers’ preferences, a model of a multi-media approach to agricultural com- munication has been developed, that could widen communication reach if implemented.