Abuse Treatment and Rehabilitation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Addiction Stigma Language- the Words We Use Matter
naabt.org The National Alliance of Advocates for Buprenorphine Treatment The Words We Use Matter. Reducing Stigma through Language. Why does language matter? Stigma remains the biggest barrier to addiction treatment faced by patients. Changing the stigma will benefit everyone. It will allow patients to The terminology used to describe addiction has contributed to the stigma. more easily regain their self esteem, allow lawmakers to appropriate Many derogatory, stigmatizing terms were championed throughout the “War funding, allow doctors to treat without disapproval of their peers, allow on Drugs” in an effort to dissuade people from misusing substances. Education insurers to cover treatment, and help the public understand this is a took a backseat, mainly because little was known about the science of medical condition as real as any other. addiction. That has changed, and the language of addiction medicine should be changed to reflect today’s greater understanding. By choosing language Choosing the words we use more carefully is one way we can all make that is not stigmatizing, we can begin to dismantle the negative stereotype a difference and help decrease the stigma. associated with addiction. “…In discussing substance use disorders, words can be powerful when used to inform, clarify, encourage, support, enlighten, and unify. On the other hand, stigmatizing words often discourage, isolate, misinform, shame, and embarrass…” Excerpt from “Substance Use Disorders: A Guide to the Use of Language” published by CSAT and SAMHSA Words to avoid and alternatives. Following are stigmatizing words and phrases which could be replaced Habit or Drug Habit with the suggested “preferred terminology” as a start in reducing the Problem with the terms: Calling addictive disorders a habit denies stigma associated with addiction. -
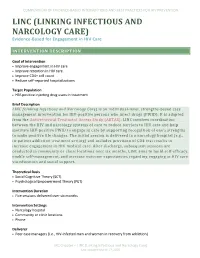
LINKING INFECTIOUS and NARCOLOGY CARE) Evidence-Based for Engagement in HIV Care
COMPENDIUM OF EVIDENCE-BASED INTERVENTIONS AND BEST PRACTICES FOR HIV PREVENTION LINC (LINKING INFECTIOUS AND NARCOLOGY CARE) Evidence-Based for Engagement in HIV Care INTERVENTION DESCRIPTION Goal of Intervention • Improve engagement in HIV care • Improve retention in HIV care • Improve CD4+ cell count • Reduce self-reported hospitalizations Target Population • HIV-positive injecting drug users in treatment Brief Description LINC (Linking Infectious and Narcology Care) is an individual-level, strengths-based case management intervention for HIV-positive persons who inject drugs (PWID). It is adapted from the Antiretroviral Treatment Access Study (ARTAS). LINC involves coordination between the HIV and narcology systems of care to reduce barriers to HIV care and help motivate HIV-positive PWID to engage in care by supporting recognition of one’s strengths to make positive life changes. The initial session is delivered in a narcology hospital (e.g., in-patient addiction treatment setting) and includes provision of CD4 test results to increase engagement in HIV medical care. After discharge, subsequent sessions are conducted in community or clinic locations over six months. LINC aims to build self-efficacy, enable self-management, and increase outcome expectancies regarding engaging in HIV care via education and social support. Theoretical Basis • Social Cognitive Theory (SCT) • Psychological Empowerment Theory (PET) Intervention Duration • Five sessions delivered over six months Intervention Settings • Narcology hospital • Community or clinic locations • Phone Deliverer • Peer case managers (i.e., HIV-infected men and women in recovery from addiction) LRC Chapter – LINC (Linking Infectious and Narcology Care) Last updated March 17, 2020 COMPENDIUM OF EVIDENCE-BASED INTERVENTIONS AND BEST PRACTICES FOR HIV PREVENTION Delivery Methods • Case management • Printed materials • Discussion • Video • Goal setting Structural Components There are no reported structural components reported for this study. -

Addiction and Substance Abuse in Anesthesiology Ethan O
Ⅵ REVIEW ARTICLES David S. Warner, M.D., and Mark A. Warner, M.D., Editors Anesthesiology 2008; 109:905–17 Copyright © 2008, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Addiction and Substance Abuse in Anesthesiology Ethan O. Bryson, M.D.,* Jeffrey H. Silverstein, M.D.† Despite substantial advances in our understanding of addic- idents, and 19% reported at least one pretreatment tion and the technology and therapeutic approaches used to fatality.2 Substantial advances have occurred in our fight this disease, addiction still remains a major issue in the understanding of addiction as well as both the tech- anesthesia workplace, and outcomes have not appreciably changed. Although alcoholism and other forms of impair- nology and therapeutic approaches used to fight this ment, such as addiction to other substances and mental ill- disease, although outcomes have not appreciably ness, impact anesthesiologists at rates similar to those in changed. Starting with a brief review of the basic other professions, as recently as 2005, the drug of choice for concepts of addiction, this article highlights the cur- anesthesiologists entering treatment was still an opioid. rent thoughts regarding the pathophysiologic basis of There exists a considerable association between chemical dependence and other psychopathology, and successful addiction, as well as clinical manifestations, legal is- treatment for addiction is less likely when comorbid psycho- sues, and treatment strategies. pathology is not treated. Individuals under evaluation or Anesthesiologists (as well as any physician) may suffer treatment for substance abuse should have an evaluation from addiction to any number of substances, though with subsequent management of comorbid psychiatric con- addiction to opioids remains the most common. -

Boletin De Documentación Nº 37, Marzo De 2009
Su elaboración en formato electrónico, iniciada en julio de 2002, ha supuesto importantes ventajas de cara a ampliar y agilizar su difusión entre los profesionales del sector, permitiendo asimismo la localización de documentación relevante por parte de cualquier ciudadano interesado en el campo de las drogodependencias. Como en los números anteriores, en el boletín de marzo se recogen las principales novedades bibliográficas que, sobre los distintos aspectos relacionados con las adicciones, han tenido entrada en el Centro de Documentación e Información de la Delegación del Gobierno para el Plan Nacional sobre Drogas en los tres últimos meses. El contenido del Boletín está estructurado en tres grandes epígrafes: Novedades bibliográficas (clasificadas por su temática y con indicación de su ruta en el caso de que estén disponibles a texto completo en Internet), Legislación y Sumarios de revistas. Esperamos que el Boletín, cuya difusión se realiza a través de listas de distribución de correo electrónico y de su presencia permanente en la página web de la Delegación del Gobierno para el Plan Nacional sobre Drogas, sea de interés y quedamos a la espera de cualquier sugerencia y/o consulta que sobre el mismo queráis formular. Ministerio de Sanidad y Consumo. Delegación del Gobierno para el Plan Nacional sobre Drogas José del Val – E-correo: [email protected] Jefe de Servicio del Centro de Documentación e Información 1 Aspectos Generales ........................................................................ 4 Aspectos Sociales ............................................................................ -

Addiction Medicine
Supplemental Guide for Addiction Medicine Supplemental Guide: Addiction Medicine January 2019 Supplemental Guide for Addiction Medicine Milestones Supplemental Guide This document provides additional guidance and examples for the Addiction Medicine Milestones. This is not designed to indicate any specific requirements for each level, but to provide insight into the thinking of the Milestone Work Group. Included in this document is the intent of each Milestone and examples of what a Clinical Competency Committee (CCC) might expect to be observed/assessed at each level. Also included are suggested assessment models and tools for each subcompetency, references, and other useful information. Review this guide with the CCC and faculty members. As the program develops a shared mental model of the Milestones, consider creating an individualized guide (Supplemental Guide Template available) with institution/program-specific examples, assessment tools used by the program, and curricular components. 2 Supplemental Guide for Addiction Medicine Patient Care 1: Screening, Evaluation, Differential Diagnosis, and Case Formulation of the Patient with or at Risk for Substance Use, Addictive Disorders, and Comorbidities Overall Intent: To correctly identify patient on continuum from low risk to substance use disorder (meeting DSM-5 criteria) while recognizing other medical and psychiatric conditions and contributing social factors Milestones Examples Level 1 Uses validated screening and • Correctly administers a National Institute on Alcohol Abuse and Alcoholism -

Use of the Communication Checklist
Psychiatria Danubina, 2020; Vol. 32, Suppl. 1, pp 88-92 Conference paper © Medicinska naklada - Zagreb, Croatia USE OF THE COMMUNICATION CHECKLIST - SELF REPORT (CC-SR) IN SCHIZOPHRENIA: LANGUAGE IMPAIRMENTS CORRELATE WITH POOR PREMORBID SOCIAL ADJUSTMENT Daria Smirnova1,2, Svetlana Zhukova3, Olga Izmailova4, Ilya Fedotov5, Yurii Osadshiy6, Alexander Shustov7, Anna Spikina8, Dmitriy Ubeikon9, Anna Yashikhina2, Natalia Petrova10, Johanna Badcock1, Vera Morgan1 & Assen Jablensky1 1Centre for Clinical Research in Neuropsychiatry, University of Western Australia, Perth, Australia 2Department of Psychiatry, Narcology, Psychotherapy and Clinical Psychology, Samara State Medical University, Samara, Russia 3Department of Psychiatry, Narcology and Psychology, Ivanovo State Medical Academy, Ivanovo, Russia 4Samara District Clinical Psychiatric Hospital, Samara, Russia 5Department of Psychiatry, Ryazan State Medical University n.a. academician I.P. Pavlov, Ryazan, Russia 6Department of Psychiatry, Narcology and Medical Psychology, Rostov State Medical University, Rostov-on-Don, Russia 7National Medical Research Centre of Psychiatry and Narcology n.a. V.P. Serbsky, Moscow, Russia 8Psychoneurological dispensary ʋ2, Saint Petersburg, Russia 9Department of Psychiatry, Narcology and Psychotherapy with the course of General and Medical psychology, S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, Simferopol, Republic of Crimea, Russia 10Department of Psychiatry and Narcology, Saint Petersburg State University, Saint Petersburg, -

Overview of Substance Use Disorder (SUD) Care Clinical Guidelines
Overview of Substance Use Disorder (SUD) Care Clinical Guidelines: A Resource for States Developing SUD Delivery System Reforms April 2017 For the past two years, the Medicaid Innovation Accelerator Program (IAP) has been providing a broad group of state Medicaid and behavioral health agencies with a variety of technical support resources to support the development of robust approaches for addressing substance use disorders (SUD). In addition, IAP has also been working directly with a small group of leader states on issues related to reducing substance use disorders, as well as with a number of states to assist with their planning and development of section 1115 demonstration proposals focusing on SUD.1 Through our close work with states under various IAP SUD activities, we have developed tools and resources such as this one designed to support state efforts to introduce policy, program and payment reforms appropriate for a robust SUD delivery system. The purpose of this resource is to support states in their ongoing efforts to introduce SUD service coverage and delivery system reforms by providing information about the preventive, treatment and recovery services and the levels of care comprising the continuum of SUD care. This document also provides an overview of nationally developed guidelines for SUD treatment criteria, including provider and service standards for each level of care. In addition, it provides useful tools and examples of state-based initiatives that can assist states in their efforts to ensure that care is delivered consistent with industry standard SUD treatment guidelines and that Medicaid beneficiaries receive the most appropriate services given their treatment and recovery needs. -

Workbook Psychiatry and Narcology
Kharkiv National Medical University Department of Psychiatry, Narcology and Medical Psychology WORKBOOK MANUAL FOR INDIVIDUAL WORK FOR MEDICAL STUDENTS PSYCHIATRY AND NARCOLOGY (Part 2) Student ___________________________________________________________ Faculty _________________________________________________________ Course _________________ Group _____________________________________ Kharkiv 2019 Затверджено вченою радою ХНМУ Протокол №5 від 23.05.2019 р. Psychiatry (Part 2) : workbook manual for individual work of students / I. Strelnikova, G. Samardacova, К. Zelenska – Kharkiv, 2019. – 103 p. Копіювання для розповсюдження в будь-якому вигляді частин або повністю можливо тільки з дозволу авторів навчального посібника. CLASS 7. NEUROTIC DISORDERS. CLINICAL FORMS. TREATMENT AND REHABILITATION. POSTTRAUMATIC STRESS DISORDER. TREATMENT AND REHABILITATION. Psychogenic diseases are a large and clinically varied group of diseases resulting from an effect of acute or long-term psychic traumas, which manifest themselves by both mental and somatoneurological disorders and, as a rule, are reversible. Psychogenic diseases are caused by a psychic trauma, i.e. some events which affect significant aspects of existence of the human being and result in deep psychological feelings. These may be subjectively significant events, i.e. those which are pathogenic for the majority of people. Besides, the psyche may be traumatized by conventionally pathogenic events, which cause feelings in an individual because of his peculiar hierarchy of values. Unfavorable psychogenic effects on the human being cause stress in him, i.e. a nonspecific reaction at the physiological, psychological and behavioural levels. Stress may exert some positive, mobilizing influence, but may result in disorganization of the organism activity. The stress, which exerts a negative influence and causes various disturbances and even diseases, is termed distress. Classification of neurotic disorders I. -

Young Psychiatrists' Network Meeting “Stigma from the Yps' Perspective: Hopes and Challenges”, September 27-29 2012, Minsk, Belarus
International conference 3rd Young Psychiatrists’ Network Meeting “Stigma From The YPs' perspective: Hopes and Challenges” September 27-29, 2012 Programme and abstract booklet Ministry of Health of the Republic Of Belarus State Educational Establishment “Belarusian Medical Academy of Post-Graduate Education” Supported by Rotary club “Minsk” International conference 3rd Young Psychiatrists’ Network Meeting “Stigma From The YPs' perspective: Hopes and Challenges” September 27-29, 2012 Programme and abstract booklet Ltd “Magic” Minsk 2012 UDC (УДК) 61 LCN (ББК) 56.14 Scientific edition 3rd Young Psychiatrists' Network Meeting “Stigma From The YPs' perspective: Hopes and Challenges”, September 27-29 2012, Minsk, Belarus. International conference: Programme and abstract booklet. – Minsk: Publishing house “Magic“, 2012. - 84 p. ISBN 978 – 985-6473-81-7 Supported by European Federation of Psychiatrists’ Trainees (EFPT) Supported by Belarusian Medical Academy of Post-Graduate Education (BelMAPGE) Supported by Belarusian Psychiatric Association (BPA) Supported by Rotary club “Minsk” Editorial Board: J. Hanson, MD, PhD, Assoc. Prof., Sweden; D. Krupchanka, MD, PhD student, Belarusian Medical Academy of Postgraduate Education, Minsk, Belarus; N. Bezborodovs, MD, Riga Stradins University, Riga Centre of Psychiatry and Addiction Disorders, Latvia; M. Bendix, MD, Dr. Med., Karolinska University Hospital Huddinge, Sweden; S. Jauhar, MD, MBChB, BSc (Hons), MRCPsych, Department of Psychosis Studies, Institute of Psychiatry, United Kingdom; D. Smirnova, MD, PhD, Samara State Medical University, Russian Federation. ISBN 978 – 985-6473-81-7 © State Educational Establishment “Belarusian Medical Academy of Post- Graduate Education” Anyone who keeps learning stays young. The greatest thing in life is to keep your mind young. (c) There is a story of our meetings. -

Drug Testing: a White Paper of the American Society of Addiction Medicine (ASAM)
Drug Testing: A White Paper of the American Society of Addiction Medicine (ASAM) October 26, 2013 DRUG TESTING: A WHITE PAPER OF THE AMERICAN SOCIETY OF ADDICTION MEDICINE Adopted by the Board of Directors 10/26/2013 © Copyright 2013. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the first page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specific written permission or license from the Society. ASAM Public Policy Statements normally may be referenced in their entirety only, without editing or paraphrasing, and with proper attribution to the Society. Excerpting any statement for any purpose requires specific written permission from the Society. Public Policy statements of ASAM are revised on a regular basis; therefore, those wishing to utilize this document must ensure that it is the most current position of ASAM on the topic addressed. American Society of Addiction Medicine 4601 North Park Avenue, Upper Arcade Suite 101, Chevy Chase, MD 20815-4520 TREAT ADDICTION • SAVE LIVES PHONE: (301) 656-3920 • FACSIMILE: (301) 656-3815 E-MAIL: [email protected] • WEBSITE: HTTP://WWW.ASAM.ORG Writing Committee Members Robert L. DuPont, M.D., Committee Chair President, Institute for Behavior and Health, Inc. Corinne L. Shea, MA, Editor Director of Communications, Institute for Behavior and Health, Inc. -

Bioethical Differences Between Drug Addiction Treatment Professionals Inside and Outside the Russian Federation Mendelevich
Bioethical differences between drug addiction treatment professionals inside and outside the Russian Federation Mendelevich Mendelevich Harm Reduction Journal 2011, 8:15 http://www.harmreductionjournal.com/content/8/1/15 (10 June 2011) Mendelevich Harm Reduction Journal 2011, 8:15 http://www.harmreductionjournal.com/content/8/1/15 RESEARCH Open Access Bioethical differences between drug addiction treatment professionals inside and outside the Russian Federation Vladimir D Mendelevich Abstract This article provides an overview of a sociological study of the views of 338 drug addiction treatment professionals. A comparison is drawn between the bioethical approaches of Russian and foreign experts from 18 countries. It is concluded that the bioethical priorities of Russian and foreign experts differ significantly. Differences involve attitudes toward confidentiality, informed consent, compulsory treatment, opioid agonist therapy, mandatory testing of students for psychoactive substances, the prevention of mental patients from having children, harm reduction programs (needle and syringe exchange), euthanasia, and abortion. It is proposed that the cardinal dissimilarity between models for providing drug treatment in the Russian Federation versus the majority of the countries of the world stems from differing bioethical attitudes among drug addiction treatment experts. Introduction deontological norms [6,10]. Although there have been Russian and international narcology (addiction medi- calls for adherence to the principles of medical ethics, cine) began to develop along divergent paths during the the procedures put into practicecontinuetobeincom- second half of the twentieth century. Indeed, Russian patible with these principles. Drug addicts still have narcology has ceased to be a part of international nar- even fewer patient rights than the mentally ill. -

Pain and Addiction Case Vignette: James J
Pain and Addiction James J. Manlandro, DO, FAOAAM, FACOFP, DABM American Osteopathic Academy of Addiction Medicine 1 James Manlandro, DO, FAOAAM FACOAFP, DABM Disclosures • James Manlandro, DO, FAOAAM, FACOAFP, DABM is a paid speaker for Reckitt Benckiser The contents of this activity may include discussion of off label or investigative drug uses. The faculty is aware that is their responsibility to disclose this information. 2 Planning Committee, Disclosures AAAP aims to provide educational information that is balanced, independent, objective and free of bias and based on evidence. In order to resolve any identified Conflicts of Interest, disclosure information from all planners, faculty and anyone in the position to control content is provided during the planning process to ensure resolution of any identified conflicts. This disclosure information is listed below: The following developers and planning committee members have reported that they have no commercial relationships relevant to the content of this module to disclose: PCSSMAT lead contributors Maria Sullivan, MD, PhD, Adam Bisaga, MD and Frances Levin, MD; AAAP CME/CPD Committee Members Dean Krahn, MD, Kevin Sevarino, MD, PhD, Tim Fong, MD, Robert Milin, MD, Tom Kosten, MD, Joji Suzuki, MD; AOAAM Staff Stephen Wyatt, DO, Nina Albano Vidmer and Lara Renucci; and AAAP Staff Kathryn Cates-Wessel, Miriam Giles and Blair-Victoria Dutra. All faculty have been advised that any recommendations involving clinical medicine must be based on evidence that is accepted within the profession of medicine as adequate justification for their indications and contraindications in the care of patients. All scientific research referred to, reported, or used in the presentation must conform to the generally accepted standards of experimental design, data collection, and analysis.