Progressive External Ophthalmoplegia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Materials: Evaluation of Cytotoxicity and Α-Glucosidase Inhibitory Activity of Amide and Polyamino-Derivatives of Lupane Triterpenoids
Supplementary Materials: Evaluation of cytotoxicity and α-glucosidase inhibitory activity of amide and polyamino-derivatives of lupane triterpenoids Oxana B. Kazakova1*, Gul'nara V. Giniyatullina1, Akhat G. Mustafin1, Denis A. Babkov2, Elena V. Sokolova2, Alexander A. Spasov2* 1Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences, 71, pr. Oktyabrya, 450054 Ufa, Russian Federation 2Scientific Center for Innovative Drugs, Volgograd State Medical University, Novorossiyskaya st. 39, Volgograd 400087, Russian Federation Correspondence Prof. Dr. Oxana B. Kazakova Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences 71 Prospeсt Oktyabrya Ufa, 450054 Russian Federation E-mail: [email protected] Prof. Dr. Alexander A. Spasov Scientific Center for Innovative Drugs of the Volgograd State Medical University 39 Novorossiyskaya st. Volgograd, 400087 Russian Federation E-mail: [email protected] Figure S1. 1H and 13C of compound 2. H NH N H O H O H 2 2 Figure S2. 1H and 13C of compound 4. NH2 O H O H CH3 O O H H3C O H 4 3 Figure S3. Anticancer screening data of compound 2 at single dose assay 4 Figure S4. Anticancer screening data of compound 7 at single dose assay 5 Figure S5. Anticancer screening data of compound 8 at single dose assay 6 Figure S6. Anticancer screening data of compound 9 at single dose assay 7 Figure S7. Anticancer screening data of compound 12 at single dose assay 8 Figure S8. Anticancer screening data of compound 13 at single dose assay 9 Figure S9. Anticancer screening data of compound 14 at single dose assay 10 Figure S10. -

Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient with Mutations in POLG2 and OPA1
OBSERVATION Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient With Mutations in POLG2 and OPA1 Silvio Ferraris, MD; Susanna Clark, PhD; Emanuela Garelli, PhD; Guido Davidzon, MD; Steven A. Moore, MD, PhD; Randy H. Kardon, MD, PhD; Rachelle J. Bienstock, PhD; Matthew J. Longley, PhD; Michelangelo Mancuso, MD; Purificación Gutiérrez Ríos, MS; Michio Hirano, MD; William C. Copeland, PhD; Salvatore DiMauro, MD Objective: To describe the clinical features, muscle mitochondrial DNA showed multiple deletions. The re- pathological characteristics, and molecular studies of a sults of screening for mutations in the nuclear genes asso- patient with a mutation in the gene encoding the acces- ciated with PEO and multiple mitochondrial DNA dele- sory subunit (p55) of polymerase ␥ (POLG2) and a mu- tions, including those in POLG (polymerase ␥ gene), ANT1 tation in the OPA1 gene. (gene encoding adenine nucleotide translocator 1), and PEO1, were negative, but sequencing of POLG2 revealed a Design: Clinical examination and morphological, bio- G1247C mutation in exon 7, resulting in the substitution chemical, and molecular analyses. of a highly conserved glycine with an alanine at codon 416 (G416A). Because biochemical analysis of the mutant pro- Setting: Tertiary care university hospitals and molecu- tein showed no alteration in chromatographic properties lar genetics and scientific computing laboratory. and normal ability to protect the catalytic subunit from N-ethylmaleimide, we also sequenced the OPA1 gene and Patient: A 42-year-old man experienced hearing loss, identified a novel heterozygous mutation (Y582C). progressive external ophthalmoplegia (PEO), loss of cen- tral vision, macrocytic anemia, and hypogonadism. His family history was negative for neurological disease, and Conclusion: Although we initially focused on the mu- his serum lactate level was normal. -

Gout Et Al Ultra-Mutation Targets Germline Alleles in an Infant Leukemia Recapitulation of Human Germline Coding Variation in An
bioRxiv preprint doi: https://doi.org/10.1101/248690; this version posted February 7, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Gout et al Ultra-mutation targets germline alleles in an infant leukemia 1 Recapitulation of human germline coding variation in an ultra-mutated infant leukemia 2 Alexander M Gout1, Rishi S Kotecha2,3,4, Parwinder Kaur5,6, Ana Abad1, Bree Foley7, Kim W 3 Carter8, Catherine H Cole3, Charles Bond9, Ursula R Kees2, Jason Waithman7,*, Mark N 4 Cruickshank1* 5 1Cancer Genomics and Epigenetics Laboratory, Telethon Kids Cancer Centre, Telethon Kids 6 Institute, University of Western Australia, Perth, Australia. 7 2Leukaemia and Cancer Research Laboratory, Telethon Kids Cancer Centre, Telethon Kids 8 Institute, Perth, Australia. 9 3Department of Haematology and Oncology, Princess Margaret Hospital for Children, Perth, 10 Australia. 11 4School of Medicine, University of Western Australia, Perth, Australia. 12 5Personalised Medicine Centre for Children, Telethon Kids Institute, Australia. 13 6Centre for Plant Genetics & Breeding, UWA School of Agriculture & Environment. 14 7Cancer Immunology Unit, Telethon Kids Institute, Perth, Australia. 15 8McCusker Charitable Foundation Bioinformatics Centre, Telethon Kids Institute, Perth, 16 Australia. 17 9School of Molecular Sciences, The University of Western Australia, Perth, Australia. 18 19 * These authors contributed equally to this work. Correspondence and requests for 20 materials should be addressed to J.W. ([email protected]) or to M.N.C. -

WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T (51) International Patent Classification: (72) Inventors: TARNOPOLSKY, Mark; 309-397 King C12N 5/ 0 (2006.01) C12N 15/53 (2006.01) Street West, Dundas, Ontario L9H 1W9 (CA). SAFDAR, A61K 35/12 (2015.01) C12N 15/54 (2006.01) Adeel; c/o McMaster University, 1200 Main Street West, A61K 9/51 (2006.01) C12N 15/55 (2006.01) Hamilton, Ontario L8N 3Z5 (CA). C12N 15/11 (2006.01) C12N 15/85 (2006.01) (74) Agent: TANDAN, Susan; Gowling WLG (Canada) LLP, C12N 15/12 (2006.01) C12N 5/071 (2010.01) One Main Street West, Hamilton, Ontario L8P 4Z5 (CA). (21) International Application Number: (81) Designated States indicated, PCT/CA20 16/050046 (unless otherwise for every kind of national protection available): AE, AG, AL, AM, (22) International Filing Date: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 2 1 January 2016 (21 .01 .2016) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (26) Publication Language: English KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (30) Priority Data: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 62/105,967 2 1 January 2015 (21.01.2015) US SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 62/1 12,940 6 February 2015 (06.02.2015) US TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Mitochondrial DNA Mutations Cause Various Diseases
2013 Neurobiology of Disease in Children Symposium: Mitochondrial Disease, October 30, 2013 Defects of Mitochondrial DNA Replication William C. Copeland Laboratory of Molecular Genetics Mitochondrial DNA mutations cause various diseases * Alpers Disease * Leigh Disease or Syndrome * Barth syndrome * LHON * Beta-oxidation Defects * LIC (Lethal Infantile Cardiomyopathy) * Carnitine-Acyl-Carnitine * Luft Disease Deficiency * MAD * Carnitine Deficiency * MCAD * Co-Enzyme Q10 Deficiency * MELAS * Complex I Deficiency * MERRF * Complex II Deficiency * Mitochondrial Cytopathy * Complex III Deficiency * Mitochondrial DNA Depletion * Complex IV Deficiency * Mitochondrial Encephalopathy * Complex V Deficiency * Mitochondrial Myopathy * COX Deficiency * MNGIE * CPEO * NARP * CPT I Deficiency * Pearson Syndrome * CPT II Deficiency * Pyruvate Carboxylase Deficiency * Glutaric Aciduria Type II * Pyruvate Dehydrogenase Deficiency * KSS * Respiratory Chain * Lactic Acidosis * SCAD * LCAD * SCHAD * LCHAD * VLCAD Origins of mtDNA mutations Damage to DNA •Environmental factors •Endogenous oxidative stress Spontaneous errors •DNA replication •Translesion synthesis •DNA repair re-synthesis Mitochondrial DNA replication p32 - RNaseH 16 Human DNA Polymerases Polymerase Family Chromosome Mol. Wt. (kDa) Function/Comments α (alpha) B Xq21.3-q22.1 165 Initiates replication β (beta) X 8p12-p11 39 BER, other functions γ (gamma) A 15q25 140 Mitochondrial replication & repair δ (delta) B 19q13.3-.4 125 Replication, BER, NER, MMR ε (epsilon) B 12q24.3 255 Replication, checkpoint -
See a Sample Report
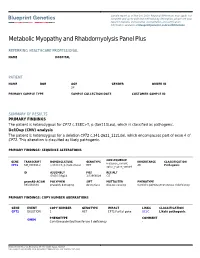
Sample report as of Nov 1st, 2020. Regional differences may apply. For complete and up-to-date test methodology description, please see your report in Nucleus online portal. Accreditation and certification information available at blueprintgenetics.com/certifications Metabolic Myopathy and Rhabdomyolysis Panel Plus REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL PATIENT NAME DOB AGE GENDER ORDER ID 28 PRIMARY SAMPLE TYPE SAMPLE COLLECTION DATE CUSTOMER SAMPLE ID SUMMARY OF RESULTS PRIMARY FINDINGS The patient is heterozygous for CPT2 c.338C>T, p.(Ser113Leu), which is classified as pathogenic. Del/Dup (CNV) analysis The patient is heterozygous for a deletion CPT2 c.341-2621_1121del, which encompasses part of exon 4 of CPT2. This alteration is classified as likely pathogenic. PRIMARY FINDINGS: SEQUENCE ALTERATIONS CONSEQUENCE GENE TRANSCRIPT NOMENCLATURE GENOTYPE INHERITANCE CLASSIFICATION missense_variant, CPT2 NM_000098.2 c.338C>T, p.(Ser113Leu) HET AR Pathogenic splice_region_variant ID ASSEMBLY POS REF/ALT GRCh37/hg19 1:53668099 C/T gnomAD AC/AN POLYPHEN SIFT MUTTASTER PHENOTYPE 393/282834 probably damaging deleterious disease causing Carnitine palmitoyltransferase II deficiency PRIMARY FINDINGS: COPY NUMBER ABERRATIONS GENE EVENT COPY NUMBER GENOTYPE IMPACT LINKS CLASSIFICATION CPT2 DELETION 1 HET CPT2:Partial gene UCSC Likely pathogenic PHENOTYPE COMMENT OMIM Carnitine palmitoyltransferase II deficiency - Blueprint Genetics Oy, Keilaranta 16 A-B, 02150 Espoo, Finland VAT number: FI22307900, CLIA ID Number: 99D2092375, CAP Number: 9257331 -

Overview of Research on Fusion Genes in Prostate Cancer
2011 Review Article Overview of research on fusion genes in prostate cancer Chunjiao Song1,2, Huan Chen3 1Medical Research Center, Shaoxing People’s Hospital, Shaoxing University School of Medicine, Shaoxing 312000, China; 2Shaoxing Hospital, Zhejiang University School of Medicine, Shaoxing 312000, China; 3Key Laboratory of Microorganism Technology and Bioinformatics Research of Zhejiang Province, Zhejiang Institute of Microbiology, Hangzhou 310000, China Contributions: (I) Conception and design: C Song; (II) Administrative support: Shaoxing Municipal Health and Family Planning Science and Technology Innovation Project (2017CX004) and Shaoxing Public Welfare Applied Research Project (2018C30058); (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: C Song; (V) Data analysis and interpretation: H Chen; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Chunjiao Song. No. 568 Zhongxing Bei Road, Shaoxing 312000, China. Email: [email protected]. Abstract: Fusion genes are known to drive and promote carcinogenesis and cancer progression. In recent years, the rapid development of biotechnologies has led to the discovery of a large number of fusion genes in prostate cancer specimens. To further investigate them, we summarized the fusion genes. We searched related articles in PubMed, CNKI (Chinese National Knowledge Infrastructure) and other databases, and the data of 92 literatures were summarized after preliminary screening. In this review, we summarized approximated 400 fusion genes since the first specific fusion TMPRSS2-ERG was discovered in prostate cancer in 2005. Some of these are prostate cancer specific, some are high-frequency in the prostate cancer of a certain ethnic group. This is a summary of scientific research in related fields and suggests that some fusion genes may become biomarkers or the targets for individualized therapies. -
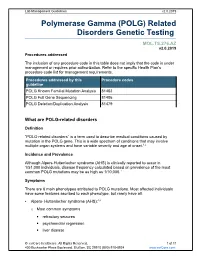
Polymerase Gamma (POLG) Related Disorders Genetic Testing
Lab Management Guidelines v2.0.2019 Polymerase Gamma (POLG) Related Disorders Genetic Testing MOL.TS.276.AZ v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline POLG Known Familial Mutation Analysis 81403 POLG Full Gene Sequencing 81406 POLG Deletion/Duplication Analysis 81479 What are POLG-related disorders Definition “POLG-related disorders” is a term used to describe medical conditions caused by mutation in the POLG gene. This is a wide spectrum of conditions that may involve multiple organ systems and have variable severity and age at onset.1,2 Incidence and Prevalence Although Alpers-Huttenlocher syndrome (AHS) is clinically reported to occur in 1/51,000 individuals, disease frequency calculated based on prevalence of the most common POLG mutations may be as high as 1/10,000.1 Symptoms There are 6 main phenotypes attributed to POLG mutations. Most affected individuals have some features ascribed to each phenotype, but rarely have all. Alpers- Huttenlocher syndrome (AHS):3,4 o Most common symptoms . refractory seizures . psychomotor regression . liver disease © eviCore healthcare. All Rights Reserved. 1 of 11 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 o Orther possible symptoms . migraine with visual auras . cortical blindness . hypotonia . ataxia . extrapyramidal movements . peripheral neuropathy . progressive spastic paraparesis . renal tubular acidosis . hearing loss . cyclic vomiting . pancreatitis o Development is often normal until disease onset, which is typically before 4 years of age. -

Dominant Mutations in Mtdna Maintenance Gene SSBP1 Cause Optic Atrophy and Foveopathy
Dominant mutations in mtDNA maintenance gene SSBP1 cause optic atrophy and foveopathy Camille Piro-Mégy, … , Maria Sola, Cécile Delettre J Clin Invest. 2020;130(1):143-156. https://doi.org/10.1172/JCI128513. Research Article Genetics Ophthalmology Graphical abstract Find the latest version: https://jci.me/128513/pdf The Journal of Clinical Investigation RESEARCH ARTICLE Dominant mutations in mtDNA maintenance gene SSBP1 cause optic atrophy and foveopathy Camille Piro-Mégy,1 Emmanuelle Sarzi,1 Aleix Tarrés-Solé,2 Marie Péquignot,1 Fenna Hensen,3 Mélanie Quilès,1 Gaël Manes,1 Arka Chakraborty,2 Audrey Sénéchal,1 Béatrice Bocquet,1,4 Chantal Cazevieille,1 Agathe Roubertie,1,4 Agnès Müller,1,5 Majida Charif,6 David Goudenège,6 Guy Lenaers,6 Helmut Wilhelm,7 Ulrich Kellner,8 Nicole Weisschuh,9 Bernd Wissinger,9 Xavier Zanlonghi,10 Christian Hamel,1,4 Johannes N. Spelbrink,3 Maria Sola,2 and Cécile Delettre1 1Institute of Neurosciences of Montpellier, INSERM, University of Montpellier, Montpellier, France. 2Structural MitoLab, Department of Structural Biology, “Maria de Maeztu” Unit of Excellence, Molecular Biology Institute Barcelona (IBMB-CSIC), Barcelona, Spain. 3Radboud Center for Mitochondrial Medicine, Department of Paediatrics, Radboudumc, Nijmegen, Netherlands. 4CHU Montpellier, Centre of Reference for Genetic Sensory Diseases, Gui de Chauliac Hospital, Montpellier, France. 5Faculté de Pharmacie, Université de Montpellier, Montpellier, France. 6UMR CNRS 6015-INSERM U1083, MitoVasc Institute, Angers University, Angers, France. 7University Eye Hospital, Centre for Ophthalmology, University of Tübingen, Tübingen, Germany. 8Rare Retinal Disease Center, AugenZentrum Siegburg, MVZ Augenärztliches Diagnostik- und Therapiecentrum Siegburg GmbH, Siegburg, Germany. 9Institute for Ophthalmic Research, Centre for Ophthalmology, University of Tübingen, Tübingen, Germany. -

A Polymorphism of the POLG2 Gene Is Genetically Associated with the Invasiveness of Urinary Bladder Cancer in Japanese Males
Journal of Human Genetics (2011) 56, 572–576 & 2011 The Japan Society of Human Genetics All rights reserved 1434-5161/11 $32.00 www.nature.com/jhg ORIGINAL ARTICLE A polymorphism of the POLG2 gene is genetically associated with the invasiveness of urinary bladder cancer in Japanese males Chanavee Ratanajaraya1, Hiroyuki Nishiyama2, Meiko Takahashi1,3, Takahisa Kawaguchi1, Ryoichi Saito2, Yoshiki Mikami4, Mikita Suyama1, Mark Lathrop5,6, Ryo Yamada1, Osamu Ogawa2 and Fumihiko Matsuda1,3,5,7 Urinary bladder cancer (UBC) is a common cancer with male predominance. Pathologically it is classified into two distinct tumor entities related to the risk of patients. The low-grade tumors with relatively well-differentiated tumor histology (G1 and G2) at stage Ta are non-invasive and pose a minimal risk, whereas high-grade tumors (G2 and G3) with stages T1 to T4 are aggressive with invasion, and therefore, pose a serious risk for the patients. DNA repair and metabolic process genes may have major roles in cancer progression and development. To identify genes associated with invasiveness of UBC, we have extensively genotyped 802 single nucleotide polymorphisms in 114 genes related to DNA repair mechanisms and metabolic processes. A genetic association study was performed between non-invasive (G1 and G2 with Ta) and invasive (G2 and G3 with T1 to T4) groups of Japanese UBC patients. We found that rs17650301 in POLG2 showed marked difference in genotype distribution between the two groups in males (P¼6.93Â10À4), which was further confirmed in an independent sample set (overall P¼1.67Â10À4). We also found by an in silico analysis that the risk allele of rs17650301 increased the transcription of POLG2. -

Gnomad Lof Supplement
1 gnomAD supplement gnomAD supplement 1 Data processing 4 Alignment and read processing 4 Variant Calling 4 Coverage information 5 Data processing 5 Sample QC 7 Hard filters 7 Supplementary Table 1 | Sample counts before and after hard and release filters 8 Supplementary Table 2 | Counts by data type and hard filter 9 Platform imputation for exomes 9 Supplementary Table 3 | Exome platform assignments 10 Supplementary Table 4 | Confusion matrix for exome samples with Known platform labels 11 Relatedness filters 11 Supplementary Table 5 | Pair counts by degree of relatedness 12 Supplementary Table 6 | Sample counts by relatedness status 13 Population and subpopulation inference 13 Supplementary Figure 1 | Continental ancestry principal components. 14 Supplementary Table 7 | Population and subpopulation counts 16 Population- and platform-specific filters 16 Supplementary Table 8 | Summary of outliers per population and platform grouping 17 Finalizing samples in the gnomAD v2.1 release 18 Supplementary Table 9 | Sample counts by filtering stage 18 Supplementary Table 10 | Sample counts for genomes and exomes in gnomAD subsets 19 Variant QC 20 Hard filters 20 Random Forest model 20 Features 21 Supplementary Table 11 | Features used in final random forest model 21 Training 22 Supplementary Table 12 | Random forest training examples 22 Evaluation and threshold selection 22 Final variant counts 24 Supplementary Table 13 | Variant counts by filtering status 25 Comparison of whole-exome and whole-genome coverage in coding regions 25 Variant annotation 30 Frequency and context annotation 30 2 Functional annotation 31 Supplementary Table 14 | Variants observed by category in 125,748 exomes 32 Supplementary Figure 5 | Percent observed by methylation. -

DNA Polymerase Gamma and Mitochondrial Disease: Understanding the Consequence of POLG Mutations
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1787 (2009) 312–319 Contents lists available at ScienceDirect Biochimica et Biophysica Acta journal homepage: www.elsevier.com/locate/bbabio Review DNA polymerase gamma and mitochondrial disease: Understanding the consequence of POLG mutations Sherine S.L. Chan ⁎, William C. Copeland ⁎ Laboratory of Molecular Genetics, National Institute of Environmental Health Sciences, National Institutes of Health, PO Box 12233, Research Triangle Park, NC 27709, USA article info abstract Article history: DNA polymerase γ is the only known DNA polymerase in human mitochondria and is essential for Received 31 July 2008 mitochondrial DNA replication and repair. It is well established that defects in mtDNA replication lead to Received in revised form 9 October 2008 mitochondrial dysfunction and disease. Over 160 coding variations in the gene encoding the catalytic subunit Accepted 15 October 2008 of DNA polymerase γ (POLG) have been identified. Our group and others have characterized a number of the Available online 29 October 2008 more common and interesting mutations, as well as those disease mutations in the DNA polymerase γ Keywords: accessory subunit. We review the results of these studies, which provide clues to the mechanisms leading to Mitochondria the disease state. Mitochondrial disease Published by Elsevier B.V. DNA polymerase gamma Mitochondrial DNA replication Oxidative stress 1. Introduction fashion where DNA synthesis is primed by transcription through the H strand origin within the D-loop [6]. After two-thirds of the nascent H Mitochondria have their own small 16.5 kb circular double- strand is replicated, the L strand origin is exposed, allowing initiation stranded DNA that encodes 22 tRNAs, 2 rRNAs and 13 polypeptides of nascent L strand synthesis.