A Polymorphism of the POLG2 Gene Is Genetically Associated with the Invasiveness of Urinary Bladder Cancer in Japanese Males
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Materials: Evaluation of Cytotoxicity and Α-Glucosidase Inhibitory Activity of Amide and Polyamino-Derivatives of Lupane Triterpenoids
Supplementary Materials: Evaluation of cytotoxicity and α-glucosidase inhibitory activity of amide and polyamino-derivatives of lupane triterpenoids Oxana B. Kazakova1*, Gul'nara V. Giniyatullina1, Akhat G. Mustafin1, Denis A. Babkov2, Elena V. Sokolova2, Alexander A. Spasov2* 1Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences, 71, pr. Oktyabrya, 450054 Ufa, Russian Federation 2Scientific Center for Innovative Drugs, Volgograd State Medical University, Novorossiyskaya st. 39, Volgograd 400087, Russian Federation Correspondence Prof. Dr. Oxana B. Kazakova Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences 71 Prospeсt Oktyabrya Ufa, 450054 Russian Federation E-mail: [email protected] Prof. Dr. Alexander A. Spasov Scientific Center for Innovative Drugs of the Volgograd State Medical University 39 Novorossiyskaya st. Volgograd, 400087 Russian Federation E-mail: [email protected] Figure S1. 1H and 13C of compound 2. H NH N H O H O H 2 2 Figure S2. 1H and 13C of compound 4. NH2 O H O H CH3 O O H H3C O H 4 3 Figure S3. Anticancer screening data of compound 2 at single dose assay 4 Figure S4. Anticancer screening data of compound 7 at single dose assay 5 Figure S5. Anticancer screening data of compound 8 at single dose assay 6 Figure S6. Anticancer screening data of compound 9 at single dose assay 7 Figure S7. Anticancer screening data of compound 12 at single dose assay 8 Figure S8. Anticancer screening data of compound 13 at single dose assay 9 Figure S9. Anticancer screening data of compound 14 at single dose assay 10 Figure S10. -

A Network Propagation Approach to Prioritize Long Tail Genes in Cancer
bioRxiv preprint doi: https://doi.org/10.1101/2021.02.05.429983; this version posted February 8, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. A Network Propagation Approach to Prioritize Long Tail Genes in Cancer Hussein Mohsen1,*, Vignesh Gunasekharan2, Tao Qing2, Sahand Negahban3, Zoltan Szallasi4, Lajos Pusztai2,*, Mark B. Gerstein1,5,6,3,* 1 Computational Biology & Bioinformatics Program, Yale University, New Haven, CT 06511, USA 2 Breast Medical Oncology, Yale School of Medicine, New Haven, CT 06511, USA 3 Department of Statistics & Data Science, Yale University, New Haven, CT 06511, USA 4 Children’s Hospital Informatics Program, Harvard-MIT Division of Health Sciences and Technology, Harvard Medical School, Boston, MA 02115, USA 5 Department of Molecular Biophysics and Biochemistry, Yale University, New Haven, CT 06511, USA 6 Department of Computer Science, Yale University, New Haven, CT 06511, USA * Corresponding author Abstract Introduction. The diversity of genomic alterations in cancer pose challenges to fully understanding the etiologies of the disease. Recent interest in infrequent mutations, in genes that reside in the “long tail” of the mutational distribution, uncovered new genes with significant implication in cancer development. The study of these genes often requires integrative approaches with multiple types of biological data. Network propagation methods have demonstrated high efficacy in uncovering genomic patterns underlying cancer using biological interaction networks. Yet, the majority of these analyses have focused their assessment on detecting known cancer genes or identifying altered subnetworks. -

Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient with Mutations in POLG2 and OPA1
OBSERVATION Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient With Mutations in POLG2 and OPA1 Silvio Ferraris, MD; Susanna Clark, PhD; Emanuela Garelli, PhD; Guido Davidzon, MD; Steven A. Moore, MD, PhD; Randy H. Kardon, MD, PhD; Rachelle J. Bienstock, PhD; Matthew J. Longley, PhD; Michelangelo Mancuso, MD; Purificación Gutiérrez Ríos, MS; Michio Hirano, MD; William C. Copeland, PhD; Salvatore DiMauro, MD Objective: To describe the clinical features, muscle mitochondrial DNA showed multiple deletions. The re- pathological characteristics, and molecular studies of a sults of screening for mutations in the nuclear genes asso- patient with a mutation in the gene encoding the acces- ciated with PEO and multiple mitochondrial DNA dele- sory subunit (p55) of polymerase ␥ (POLG2) and a mu- tions, including those in POLG (polymerase ␥ gene), ANT1 tation in the OPA1 gene. (gene encoding adenine nucleotide translocator 1), and PEO1, were negative, but sequencing of POLG2 revealed a Design: Clinical examination and morphological, bio- G1247C mutation in exon 7, resulting in the substitution chemical, and molecular analyses. of a highly conserved glycine with an alanine at codon 416 (G416A). Because biochemical analysis of the mutant pro- Setting: Tertiary care university hospitals and molecu- tein showed no alteration in chromatographic properties lar genetics and scientific computing laboratory. and normal ability to protect the catalytic subunit from N-ethylmaleimide, we also sequenced the OPA1 gene and Patient: A 42-year-old man experienced hearing loss, identified a novel heterozygous mutation (Y582C). progressive external ophthalmoplegia (PEO), loss of cen- tral vision, macrocytic anemia, and hypogonadism. His family history was negative for neurological disease, and Conclusion: Although we initially focused on the mu- his serum lactate level was normal. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Gout Et Al Ultra-Mutation Targets Germline Alleles in an Infant Leukemia Recapitulation of Human Germline Coding Variation in An
bioRxiv preprint doi: https://doi.org/10.1101/248690; this version posted February 7, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Gout et al Ultra-mutation targets germline alleles in an infant leukemia 1 Recapitulation of human germline coding variation in an ultra-mutated infant leukemia 2 Alexander M Gout1, Rishi S Kotecha2,3,4, Parwinder Kaur5,6, Ana Abad1, Bree Foley7, Kim W 3 Carter8, Catherine H Cole3, Charles Bond9, Ursula R Kees2, Jason Waithman7,*, Mark N 4 Cruickshank1* 5 1Cancer Genomics and Epigenetics Laboratory, Telethon Kids Cancer Centre, Telethon Kids 6 Institute, University of Western Australia, Perth, Australia. 7 2Leukaemia and Cancer Research Laboratory, Telethon Kids Cancer Centre, Telethon Kids 8 Institute, Perth, Australia. 9 3Department of Haematology and Oncology, Princess Margaret Hospital for Children, Perth, 10 Australia. 11 4School of Medicine, University of Western Australia, Perth, Australia. 12 5Personalised Medicine Centre for Children, Telethon Kids Institute, Australia. 13 6Centre for Plant Genetics & Breeding, UWA School of Agriculture & Environment. 14 7Cancer Immunology Unit, Telethon Kids Institute, Perth, Australia. 15 8McCusker Charitable Foundation Bioinformatics Centre, Telethon Kids Institute, Perth, 16 Australia. 17 9School of Molecular Sciences, The University of Western Australia, Perth, Australia. 18 19 * These authors contributed equally to this work. Correspondence and requests for 20 materials should be addressed to J.W. ([email protected]) or to M.N.C. -

WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T (51) International Patent Classification: (72) Inventors: TARNOPOLSKY, Mark; 309-397 King C12N 5/ 0 (2006.01) C12N 15/53 (2006.01) Street West, Dundas, Ontario L9H 1W9 (CA). SAFDAR, A61K 35/12 (2015.01) C12N 15/54 (2006.01) Adeel; c/o McMaster University, 1200 Main Street West, A61K 9/51 (2006.01) C12N 15/55 (2006.01) Hamilton, Ontario L8N 3Z5 (CA). C12N 15/11 (2006.01) C12N 15/85 (2006.01) (74) Agent: TANDAN, Susan; Gowling WLG (Canada) LLP, C12N 15/12 (2006.01) C12N 5/071 (2010.01) One Main Street West, Hamilton, Ontario L8P 4Z5 (CA). (21) International Application Number: (81) Designated States indicated, PCT/CA20 16/050046 (unless otherwise for every kind of national protection available): AE, AG, AL, AM, (22) International Filing Date: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 2 1 January 2016 (21 .01 .2016) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (26) Publication Language: English KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (30) Priority Data: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 62/105,967 2 1 January 2015 (21.01.2015) US SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 62/1 12,940 6 February 2015 (06.02.2015) US TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

Tyr1 Phosphorylation Promotes Phosphorylation of Ser2 on the C-Terminal Domain
1 Tyr1 phosphorylation promotes phosphorylation of Ser2 on the C-terminal domain 2 of eukaryotic RNA polymerase II by P-TEFb 3 Joshua E. Mayfield1† *, Seema Irani2*, Edwin E. Escobar3, Zhao Zhang4, Nathanial T. 4 Burkholder1, Michelle R. Robinson3, M. Rachel Mehaffey3, Sarah N. Sipe3,Wanjie Yang1, 5 Nicholas A. Prescott1, Karan R. Kathuria1, Zhijie Liu4, Jennifer S. Brodbelt3, Yan Zhang1,5 6 1 Department of Molecular Biosciences, 2Department of Chemical Engineering, 7 3 Department of Chemistry and 5 Institute for Cellular and Molecular Biology, University of 8 Texas, Austin 9 4 Department of Molecular Medicine, Institute of Biotechnology, University of Texas 10 Health Science Center at San Antonio 11 †Current Address: Department of Pharmacology, University of California, San Diego, La 12 Jolla 13 * These authors contributed equally to this paper. 14 Correspondence: Yan Zhang ([email protected]) 15 16 1 17 Summary 18 The Positive Transcription Elongation Factor b (P-TEFb) phosphorylates 19 Ser2 residues of C-terminal domain (CTD) of the largest subunit (RPB1) of RNA 20 polymerase II and is essential for the transition from transcription initiation to 21 elongation in vivo. Surprisingly, P-TEFb exhibits Ser5 phosphorylation activity in 22 vitro. The mechanism garnering Ser2 specificity to P-TEFb remains elusive and 23 hinders understanding of the transition from transcription initiation to elongation. 24 Through in vitro reconstruction of CTD phosphorylation, mass spectrometry 25 analysis, and chromatin immunoprecipitation sequencing (ChIP-seq) analysis, we 26 uncover a mechanism by which Tyr1 phosphorylation directs the kinase activity of 27 P-TEFb and alters its specificity from Ser5 to Ser2. -

Mitochondrial DNA Mutations Cause Various Diseases
2013 Neurobiology of Disease in Children Symposium: Mitochondrial Disease, October 30, 2013 Defects of Mitochondrial DNA Replication William C. Copeland Laboratory of Molecular Genetics Mitochondrial DNA mutations cause various diseases * Alpers Disease * Leigh Disease or Syndrome * Barth syndrome * LHON * Beta-oxidation Defects * LIC (Lethal Infantile Cardiomyopathy) * Carnitine-Acyl-Carnitine * Luft Disease Deficiency * MAD * Carnitine Deficiency * MCAD * Co-Enzyme Q10 Deficiency * MELAS * Complex I Deficiency * MERRF * Complex II Deficiency * Mitochondrial Cytopathy * Complex III Deficiency * Mitochondrial DNA Depletion * Complex IV Deficiency * Mitochondrial Encephalopathy * Complex V Deficiency * Mitochondrial Myopathy * COX Deficiency * MNGIE * CPEO * NARP * CPT I Deficiency * Pearson Syndrome * CPT II Deficiency * Pyruvate Carboxylase Deficiency * Glutaric Aciduria Type II * Pyruvate Dehydrogenase Deficiency * KSS * Respiratory Chain * Lactic Acidosis * SCAD * LCAD * SCHAD * LCHAD * VLCAD Origins of mtDNA mutations Damage to DNA •Environmental factors •Endogenous oxidative stress Spontaneous errors •DNA replication •Translesion synthesis •DNA repair re-synthesis Mitochondrial DNA replication p32 - RNaseH 16 Human DNA Polymerases Polymerase Family Chromosome Mol. Wt. (kDa) Function/Comments α (alpha) B Xq21.3-q22.1 165 Initiates replication β (beta) X 8p12-p11 39 BER, other functions γ (gamma) A 15q25 140 Mitochondrial replication & repair δ (delta) B 19q13.3-.4 125 Replication, BER, NER, MMR ε (epsilon) B 12q24.3 255 Replication, checkpoint -

POLR2C Mutations Are Associated with Primary Ovarian Insufficiency in Women
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author J Endocr Manuscript Author Soc. Author manuscript; Manuscript Author available in PMC 2017 October 20. Published in final edited form as: J Endocr Soc. 2017 March 1; 1(3): 162–173. doi:10.1210/js.2016-1014. POLR2C Mutations Are Associated With Primary Ovarian Insufficiency in Women Mika Moriwaki1, Barry Moore2, Timothy Mosbruger3, Deborah W. Neklason4, Mark Yandell2, Lynn B. Jorde2, and Corrine K. Welt1 1Division of Endocrinology, Metabolism and Diabetes, University of Utah, Salt Lake City, Utah 84112 2UStar Center for Genetic Discovery, Department of Human Genetics, University of Utah, Salt Lake City, Utah 84112 3Bioinformatics, Huntsman Cancer Institute, University of Utah, Salt Lake City, Utah 84112 4Division of Genetic Epidemiology, Department of Internal Medicine, University of Utah, Salt Lake City, Utah 84112 Abstract Context—Primary ovarian insufficiency (POI) results from a premature loss of oocytes, causing infertility and early menopause. The etiology of POI remains unknown in a majority of cases. Objective—To identify candidate genes in families affected by POI. Design—This was a family-based genetic study. Setting—The study was performed at two academic institutions. Patients and Other Participants—A family with four generations of women affected by POI (n = 5). Four of these women, three with an associated autoimmune diagnosis, were studied. The controls (n = 387) were recruited for health in old age. Intervention—Whole-genome sequencing was performed. Main Outcome Measure—Candidate genes were identified by comparing gene mutations in three family members and 387 control subjects analyzed simultaneously using the pedigree Variant Annotation, Analysis and Search Tool. -

Common Genetic Aberrations Associated with Metabolic Interferences in Human Type-2 Diabetes and Acute Myeloid Leukemia: a Bioinformatics Approach
International Journal of Molecular Sciences Article Common Genetic Aberrations Associated with Metabolic Interferences in Human Type-2 Diabetes and Acute Myeloid Leukemia: A Bioinformatics Approach Theodora-Christina Kyriakou 1, Panagiotis Papageorgis 1,2 and Maria-Ioanna Christodoulou 3,* 1 Tumor Microenvironment, Metastasis and Experimental Therapeutics Laboratory, Basic and Translational Cancer Research Center, Department of Life Sciences, European University Cyprus, Nicosia 2404, Cyprus; [email protected] (T.-C.K.); [email protected] (P.P.) 2 European University Cyprus Research Center, Nicosia 2404, Cyprus 3 Tumor Immunology and Biomarkers Laboratory, Basic and Translational Cancer Research Center, Department of Life Sciences, European University Cyprus, Nicosia 2404, Cyprus * Correspondence: [email protected] Abstract: Type-2 diabetes mellitus (T2D) is a chronic metabolic disorder, associated with an increased risk of developing solid tumors and hematological malignancies, including acute myeloid leukemia (AML). However, the genetic background underlying this predisposition remains elusive. We herein aimed at the exploration of the genetic variants, related transcriptomic changes and disturbances in metabolic pathways shared by T2D and AML, utilizing bioinformatics tools and repositories, as well as publicly available clinical datasets. Our approach revealed that rs11709077 and rs1801282, on PPARG, rs11108094 on USP44, rs6685701 on RPS6KA1 and rs7929543 on AC118942.1 comprise Citation: Kyriakou, T.-C.; common SNPs susceptible to the two diseases and, together with 64 other co-inherited proxy SNPs, Papageorgis, P.; Christodoulou, M.-I. may affect the expression patterns of metabolic genes, such as USP44, METAP2, PPARG, TIMP4 and Common Genetic Aberrations RPS6KA1, in adipose tissue, skeletal muscle, liver, pancreas and whole blood. -

Progressive External Ophthalmoplegia
Progressive external ophthalmoplegia Description Progressive external ophthalmoplegia is a condition characterized by weakness of the eye muscles. The condition typically appears in adults between ages 18 and 40 and slowly worsens over time. The first sign of progressive external ophthalmoplegia is typically drooping eyelids (ptosis), which can affect one or both eyelids. As ptosis worsens, affected individuals may use the forehead muscles to try to lift the eyelids, or they may lift up their chin in order to see. Another characteristic feature of progressive external ophthalmoplegia is weakness or paralysis of the muscles that move the eye ( ophthalmoplegia). Affected individuals have to turn their head to see in different directions, especially as the ophthalmoplegia worsens. People with progressive external ophthalmoplegia may also have general weakness of the muscles used for movement ( myopathy), particularly those in the neck, arms, or legs. The weakness may be especially noticeable during exercise (exercise intolerance). Muscle weakness may also cause difficulty swallowing (dysphagia). When the muscle cells of affected individuals are stained and viewed under a microscope, these cells usually appear abnormal. These abnormal muscle cells contain an excess of cell structures called mitochondria and are known as ragged-red fibers. Although muscle weakness is the primary symptom of progressive external ophthalmoplegia, this condition can be accompanied by other signs and symptoms. In these instances, the condition is referred to as progressive external ophthalmoplegia plus (PEO+). Additional signs and symptoms can include hearing loss caused by nerve damage in the inner ear (sensorineural hearing loss), weakness and loss of sensation in the limbs due to nerve damage (neuropathy), impaired muscle coordination (ataxia), a pattern of movement abnormalities known as parkinsonism, and depression. -
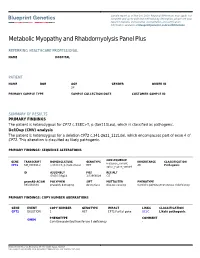
See a Sample Report
Sample report as of Nov 1st, 2020. Regional differences may apply. For complete and up-to-date test methodology description, please see your report in Nucleus online portal. Accreditation and certification information available at blueprintgenetics.com/certifications Metabolic Myopathy and Rhabdomyolysis Panel Plus REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL PATIENT NAME DOB AGE GENDER ORDER ID 28 PRIMARY SAMPLE TYPE SAMPLE COLLECTION DATE CUSTOMER SAMPLE ID SUMMARY OF RESULTS PRIMARY FINDINGS The patient is heterozygous for CPT2 c.338C>T, p.(Ser113Leu), which is classified as pathogenic. Del/Dup (CNV) analysis The patient is heterozygous for a deletion CPT2 c.341-2621_1121del, which encompasses part of exon 4 of CPT2. This alteration is classified as likely pathogenic. PRIMARY FINDINGS: SEQUENCE ALTERATIONS CONSEQUENCE GENE TRANSCRIPT NOMENCLATURE GENOTYPE INHERITANCE CLASSIFICATION missense_variant, CPT2 NM_000098.2 c.338C>T, p.(Ser113Leu) HET AR Pathogenic splice_region_variant ID ASSEMBLY POS REF/ALT GRCh37/hg19 1:53668099 C/T gnomAD AC/AN POLYPHEN SIFT MUTTASTER PHENOTYPE 393/282834 probably damaging deleterious disease causing Carnitine palmitoyltransferase II deficiency PRIMARY FINDINGS: COPY NUMBER ABERRATIONS GENE EVENT COPY NUMBER GENOTYPE IMPACT LINKS CLASSIFICATION CPT2 DELETION 1 HET CPT2:Partial gene UCSC Likely pathogenic PHENOTYPE COMMENT OMIM Carnitine palmitoyltransferase II deficiency - Blueprint Genetics Oy, Keilaranta 16 A-B, 02150 Espoo, Finland VAT number: FI22307900, CLIA ID Number: 99D2092375, CAP Number: 9257331