Mitochondrial DNA Mutations Cause Various Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Materials: Evaluation of Cytotoxicity and Α-Glucosidase Inhibitory Activity of Amide and Polyamino-Derivatives of Lupane Triterpenoids
Supplementary Materials: Evaluation of cytotoxicity and α-glucosidase inhibitory activity of amide and polyamino-derivatives of lupane triterpenoids Oxana B. Kazakova1*, Gul'nara V. Giniyatullina1, Akhat G. Mustafin1, Denis A. Babkov2, Elena V. Sokolova2, Alexander A. Spasov2* 1Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences, 71, pr. Oktyabrya, 450054 Ufa, Russian Federation 2Scientific Center for Innovative Drugs, Volgograd State Medical University, Novorossiyskaya st. 39, Volgograd 400087, Russian Federation Correspondence Prof. Dr. Oxana B. Kazakova Ufa Institute of Chemistry of the Ufa Federal Research Centre of the Russian Academy of Sciences 71 Prospeсt Oktyabrya Ufa, 450054 Russian Federation E-mail: [email protected] Prof. Dr. Alexander A. Spasov Scientific Center for Innovative Drugs of the Volgograd State Medical University 39 Novorossiyskaya st. Volgograd, 400087 Russian Federation E-mail: [email protected] Figure S1. 1H and 13C of compound 2. H NH N H O H O H 2 2 Figure S2. 1H and 13C of compound 4. NH2 O H O H CH3 O O H H3C O H 4 3 Figure S3. Anticancer screening data of compound 2 at single dose assay 4 Figure S4. Anticancer screening data of compound 7 at single dose assay 5 Figure S5. Anticancer screening data of compound 8 at single dose assay 6 Figure S6. Anticancer screening data of compound 9 at single dose assay 7 Figure S7. Anticancer screening data of compound 12 at single dose assay 8 Figure S8. Anticancer screening data of compound 13 at single dose assay 9 Figure S9. Anticancer screening data of compound 14 at single dose assay 10 Figure S10. -

Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient with Mutations in POLG2 and OPA1
OBSERVATION Progressive External Ophthalmoplegia and Vision and Hearing Loss in a Patient With Mutations in POLG2 and OPA1 Silvio Ferraris, MD; Susanna Clark, PhD; Emanuela Garelli, PhD; Guido Davidzon, MD; Steven A. Moore, MD, PhD; Randy H. Kardon, MD, PhD; Rachelle J. Bienstock, PhD; Matthew J. Longley, PhD; Michelangelo Mancuso, MD; Purificación Gutiérrez Ríos, MS; Michio Hirano, MD; William C. Copeland, PhD; Salvatore DiMauro, MD Objective: To describe the clinical features, muscle mitochondrial DNA showed multiple deletions. The re- pathological characteristics, and molecular studies of a sults of screening for mutations in the nuclear genes asso- patient with a mutation in the gene encoding the acces- ciated with PEO and multiple mitochondrial DNA dele- sory subunit (p55) of polymerase ␥ (POLG2) and a mu- tions, including those in POLG (polymerase ␥ gene), ANT1 tation in the OPA1 gene. (gene encoding adenine nucleotide translocator 1), and PEO1, were negative, but sequencing of POLG2 revealed a Design: Clinical examination and morphological, bio- G1247C mutation in exon 7, resulting in the substitution chemical, and molecular analyses. of a highly conserved glycine with an alanine at codon 416 (G416A). Because biochemical analysis of the mutant pro- Setting: Tertiary care university hospitals and molecu- tein showed no alteration in chromatographic properties lar genetics and scientific computing laboratory. and normal ability to protect the catalytic subunit from N-ethylmaleimide, we also sequenced the OPA1 gene and Patient: A 42-year-old man experienced hearing loss, identified a novel heterozygous mutation (Y582C). progressive external ophthalmoplegia (PEO), loss of cen- tral vision, macrocytic anemia, and hypogonadism. His family history was negative for neurological disease, and Conclusion: Although we initially focused on the mu- his serum lactate level was normal. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Gout Et Al Ultra-Mutation Targets Germline Alleles in an Infant Leukemia Recapitulation of Human Germline Coding Variation in An
bioRxiv preprint doi: https://doi.org/10.1101/248690; this version posted February 7, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. Gout et al Ultra-mutation targets germline alleles in an infant leukemia 1 Recapitulation of human germline coding variation in an ultra-mutated infant leukemia 2 Alexander M Gout1, Rishi S Kotecha2,3,4, Parwinder Kaur5,6, Ana Abad1, Bree Foley7, Kim W 3 Carter8, Catherine H Cole3, Charles Bond9, Ursula R Kees2, Jason Waithman7,*, Mark N 4 Cruickshank1* 5 1Cancer Genomics and Epigenetics Laboratory, Telethon Kids Cancer Centre, Telethon Kids 6 Institute, University of Western Australia, Perth, Australia. 7 2Leukaemia and Cancer Research Laboratory, Telethon Kids Cancer Centre, Telethon Kids 8 Institute, Perth, Australia. 9 3Department of Haematology and Oncology, Princess Margaret Hospital for Children, Perth, 10 Australia. 11 4School of Medicine, University of Western Australia, Perth, Australia. 12 5Personalised Medicine Centre for Children, Telethon Kids Institute, Australia. 13 6Centre for Plant Genetics & Breeding, UWA School of Agriculture & Environment. 14 7Cancer Immunology Unit, Telethon Kids Institute, Perth, Australia. 15 8McCusker Charitable Foundation Bioinformatics Centre, Telethon Kids Institute, Perth, 16 Australia. 17 9School of Molecular Sciences, The University of Western Australia, Perth, Australia. 18 19 * These authors contributed equally to this work. Correspondence and requests for 20 materials should be addressed to J.W. ([email protected]) or to M.N.C. -

WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/115632 Al 28 July 2016 (28.07.2016) W P O P C T (51) International Patent Classification: (72) Inventors: TARNOPOLSKY, Mark; 309-397 King C12N 5/ 0 (2006.01) C12N 15/53 (2006.01) Street West, Dundas, Ontario L9H 1W9 (CA). SAFDAR, A61K 35/12 (2015.01) C12N 15/54 (2006.01) Adeel; c/o McMaster University, 1200 Main Street West, A61K 9/51 (2006.01) C12N 15/55 (2006.01) Hamilton, Ontario L8N 3Z5 (CA). C12N 15/11 (2006.01) C12N 15/85 (2006.01) (74) Agent: TANDAN, Susan; Gowling WLG (Canada) LLP, C12N 15/12 (2006.01) C12N 5/071 (2010.01) One Main Street West, Hamilton, Ontario L8P 4Z5 (CA). (21) International Application Number: (81) Designated States indicated, PCT/CA20 16/050046 (unless otherwise for every kind of national protection available): AE, AG, AL, AM, (22) International Filing Date: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 2 1 January 2016 (21 .01 .2016) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (26) Publication Language: English KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (30) Priority Data: PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, 62/105,967 2 1 January 2015 (21.01.2015) US SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, 62/1 12,940 6 February 2015 (06.02.2015) US TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

The Mtdna Replication-Related Genes TFAM and POLG Are Associated with Leprosy in Han Chinese from Southwest China Journal of De
Journal of Dermatological Science 88 (2017) 349–356 Contents lists available at ScienceDirect Journal of Dermatological Science journa l homepage: www.jdsjournal.com The mtDNA replication-related genes TFAM and POLG are associated with leprosy in Han Chinese from Southwest China a a,d a a a b Dong Wang , Guo-Dong Li , Yu Fan , Deng-Feng Zhang , Rui Bi , Xiu-Feng Yu , b c a,d, Heng Long , Yu-Ye Li , Yong-Gang Yao * a Key Laboratory of Animal Models and Human Disease Mechanisms of the Chinese Academy of Sciences & Yunnan Province, Kunming Institute of Zoology, Kunming, Yunnan, 650223, China b Wenshan Institute of Dermatology, Wenshan, Yunnan, 663000, China c Department of Dermatology, The First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan, 650032, China d Kunming College of Life Science, University of Chinese Academy of Sciences, Kunming, Yunnan 650201, China A R T I C L E I N F O A B S T R A C T Article history: Background: The pathogen Mycobacterium leprae of leprosy is heavily dependent on the host energy Received 2 June 2017 metabolites and nutritional products for survival. Previously we and others have identified associations Received in revised form 7 September 2017 of several mitochondrion-related genes and mitochondrial DNA (mtDNA) copy number alterations with Accepted 13 September 2017 leprosy and/or its subtype. We hypothesized that genetic variants of mtDNA replication-related genes would affect leprosy. Keywords: Objective: We aimed to identify genetic associations between the mtDNA replication-related genes TFAM, Leprosy POLG and leprosy. TFAM Methods: Genetic association study was performed in 2898 individuals from two independent sample POLG fi eQTL sets in Yunnan Province, China. -

Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

The Role of Mitochondrial DNA Mutations in Mammalian Aging Gregory C
Review The Role of Mitochondrial DNA Mutations in Mammalian Aging Gregory C. Kujoth, Patrick C. Bradshaw, Suraiya Haroon, Tomas A. Prolla* ABSTRACT humans is likely to carry these disease-associated mutations. Thus, it is unlikely that these mutations have deleterious itochondrial DNA (mtDNA) accumulates both consequences in normal aging. Studies performed in the base-substitution mutations and deletions with Attardi laboratory have established that some specific base- M aging in several tissues in mammals. Here, we substitution mutations can reach high levels in fibroblast cells examine the evidence supporting a causative role for mtDNA derived from aged individuals [2] and also in skeletal muscle mutations in mammalian aging. We describe and compare [3]. The reason why these specific mutations accumulate in human diseases and mouse models associated with mtDNA is unclear, but they are tissue-specific and occur in mitochondrial genome instability. We also discuss potential mtDNA control sites for replication. Interestingly, the same mechanisms for the generation of these mutations and the group has found a C150T transition mutation that occurs in means by which they may mediate their pathological most or all mtDNA molecules (i.e., a homoplasmic mutation) consequences. Strategies for slowing the accumulation and is present in leukocytes from approximately 17% of attenuating the effects of mtDNA mutations are discussed. individuals aged 99–106 years old. This mutation is associated with a new replication origin position, suggesting that it may Introduction confer a survival advantage in humans [4]. With the development of high-throughput sequencing The mitochondrial theory of aging is based on the premise methods, an unbiased large-scale examination of either that reactive oxygen species (ROS), generated throughout the selected regions or the entire mtDNA sequence has become lifespan of an organism, damage mitochondrial feasible. -

EGL Test Description
2460 Mountain Industrial Boulevard | Tucker, Georgia 30084 Phone: 470-378-2200 or 855-831-7447 | Fax: 470-378-2250 eglgenetics.com Inherited Metabolic Disorders Panel: Sequencing and CNV Analysis Test Code: MM310 Turnaround time: 6 weeks CPT Codes: 81404 x1, 81406 x1, 81405 x1 Condition Description Inherited metabolic disorders refer to diseases caused by defects in genes that are involved in the body’s metabolism. These usually involve the production, conversion, or use of energy. Traditionally, inherited metabolic conditions were broadly classified as disorders of carbohydrate metabolism, amino acid metabolism, organic acid metabolism, or lysosomal storage diseases. This test analyses genes involved in complex metabolic processes in the body including but not limited to the above four categories. Reference: OMIM. Genes ACAD9, ACADL, ACADM, ACADS, ACADVL, ACSF3, AGA, AGL, ALDH5A1, ARSA, ASL, ASS1, ATPAF2, AUH, BCKDHA, BCKDHB, CD320, CLN3, CLN5, CLN6, CLN8, CPS1, CPT1A, CPT2, CYP27A1, DBT, DLD, ENO3, ETFA, ETFB, ETFDH, G6PC, GAA, GALC, GALNS, GBA, GBE1, GLA, GLB1, GM2A, GNPTAB, GYS1, GYS2, HADHA, HADHB, HGSNAT, HMGCL, HMGCS2, HYAL1, IDS, IDUA, IVD, LIPA, LMBRD1, LPIN1, MAN2B1, MANBA, MCCC1, MCCC2, MCEE, MCOLN1, MFSD8, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MMUT, MTR, MTRR, NAGA, NAGLU, NAGS, NEU1, NPC1, NPC2, OPA3, OTC, PC, PCCA, PCCB, PFKM, POLG, PPT1, PYGL, PYGM, SERAC1, SGSH, SLC17A5, SLC22A5, SLC25A13, SLC25A15, SLC25A20, SLC37A4, SLC7A7, SMPD1, SUCLG1, SUMF1, TAZ, TMEM70, TPP1 Indications This test is indicated for: Confirmation of a clinical diagnosis of inherited metabolic disorders. Methodology Next Generation Sequencing: In-solution hybridization of all coding exons is performed on the patient's genomic DNA. Although some deep intronic regions may also be analyzed, this assay is not meant to interrogate most promoter regions, deep intronic regions, or other regulatory elements, and does not detect single or multi-exon deletions or duplications. -

Mechanisms of Mitochondrial DNA Deletion Formation Nadee Nissanka1, Michal Minczuk2, and Carlos T. Moraes1 1Department of Neurol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Apollo Mechanisms of Mitochondrial DNA Deletion Formation Nadee Nissanka1, Michal Minczuk2, and Carlos T. Moraes1 1Department of Neurology, University of Miami Miller School of Medicine 33136, USA; 2Medical Research Council (MRC) Mitochondrial Biology Unit, University of Cambridge, Cambridge, UK; To whom correspondence should be addressed: Carlos T. Moraes, 1420 NW 9th Avenue, Rm.229, Miami, FL 33136; Tel: 305-243- 5858; Fax: 305-243-6955; Email: [email protected] Keywords: mitochondrial DNA, double-strand breaks, mitochondrial DNA deletions, replication Abstract Mitochondrial DNA (mtDNA) encodes a subset of genes which are essential for oxidative phosphorylation. Deletions in the mtDNA can ablate a number of these genes, and result in mitochondrial dysfunction which is associated with bona-fide mitochondrial disorders. Although mtDNA deletions are thought to occur as a result of replication errors or following double-strand breaks, the exact mechanism(s) behind deletion formation have yet to be determined. In this review we discuss the current knowledge about the fate of mtDNA following double-strand breaks, including the molecular players which mediate the degradation of linear mtDNA fragments, and possible mechanisms of re- circularization. We propose that mtDNA deletions formed from replication errors versus following double-strand breaks can be mediated by separate pathways. Mitochondrial DNA The human mitochondrial DNA (mtDNA) is a 16,569 bp circular, double-stranded, supercoiled molecule which was first discovered in 1963 [1]. The mtDNA molecule encodes 37 different genes which are essential for oxidative phosphorylation (OXPHOS) and mitochondrial protein synthesis [2]. -

Progressive External Ophthalmoplegia
Progressive external ophthalmoplegia Description Progressive external ophthalmoplegia is a condition characterized by weakness of the eye muscles. The condition typically appears in adults between ages 18 and 40 and slowly worsens over time. The first sign of progressive external ophthalmoplegia is typically drooping eyelids (ptosis), which can affect one or both eyelids. As ptosis worsens, affected individuals may use the forehead muscles to try to lift the eyelids, or they may lift up their chin in order to see. Another characteristic feature of progressive external ophthalmoplegia is weakness or paralysis of the muscles that move the eye ( ophthalmoplegia). Affected individuals have to turn their head to see in different directions, especially as the ophthalmoplegia worsens. People with progressive external ophthalmoplegia may also have general weakness of the muscles used for movement ( myopathy), particularly those in the neck, arms, or legs. The weakness may be especially noticeable during exercise (exercise intolerance). Muscle weakness may also cause difficulty swallowing (dysphagia). When the muscle cells of affected individuals are stained and viewed under a microscope, these cells usually appear abnormal. These abnormal muscle cells contain an excess of cell structures called mitochondria and are known as ragged-red fibers. Although muscle weakness is the primary symptom of progressive external ophthalmoplegia, this condition can be accompanied by other signs and symptoms. In these instances, the condition is referred to as progressive external ophthalmoplegia plus (PEO+). Additional signs and symptoms can include hearing loss caused by nerve damage in the inner ear (sensorineural hearing loss), weakness and loss of sensation in the limbs due to nerve damage (neuropathy), impaired muscle coordination (ataxia), a pattern of movement abnormalities known as parkinsonism, and depression. -
See a Sample Report
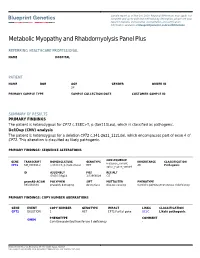
Sample report as of Nov 1st, 2020. Regional differences may apply. For complete and up-to-date test methodology description, please see your report in Nucleus online portal. Accreditation and certification information available at blueprintgenetics.com/certifications Metabolic Myopathy and Rhabdomyolysis Panel Plus REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL PATIENT NAME DOB AGE GENDER ORDER ID 28 PRIMARY SAMPLE TYPE SAMPLE COLLECTION DATE CUSTOMER SAMPLE ID SUMMARY OF RESULTS PRIMARY FINDINGS The patient is heterozygous for CPT2 c.338C>T, p.(Ser113Leu), which is classified as pathogenic. Del/Dup (CNV) analysis The patient is heterozygous for a deletion CPT2 c.341-2621_1121del, which encompasses part of exon 4 of CPT2. This alteration is classified as likely pathogenic. PRIMARY FINDINGS: SEQUENCE ALTERATIONS CONSEQUENCE GENE TRANSCRIPT NOMENCLATURE GENOTYPE INHERITANCE CLASSIFICATION missense_variant, CPT2 NM_000098.2 c.338C>T, p.(Ser113Leu) HET AR Pathogenic splice_region_variant ID ASSEMBLY POS REF/ALT GRCh37/hg19 1:53668099 C/T gnomAD AC/AN POLYPHEN SIFT MUTTASTER PHENOTYPE 393/282834 probably damaging deleterious disease causing Carnitine palmitoyltransferase II deficiency PRIMARY FINDINGS: COPY NUMBER ABERRATIONS GENE EVENT COPY NUMBER GENOTYPE IMPACT LINKS CLASSIFICATION CPT2 DELETION 1 HET CPT2:Partial gene UCSC Likely pathogenic PHENOTYPE COMMENT OMIM Carnitine palmitoyltransferase II deficiency - Blueprint Genetics Oy, Keilaranta 16 A-B, 02150 Espoo, Finland VAT number: FI22307900, CLIA ID Number: 99D2092375, CAP Number: 9257331