Cyanocobalamin Decision Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Folic Acid, Pyridoxine, and Cyanocobalamin Combination
ORIGINAL INVESTIGATION Folic Acid, Pyridoxine, and Cyanocobalamin Combination Treatment and Age-Related Macular Degeneration in Women The Women’s Antioxidant and Folic Acid Cardiovascular Study William G. Christen, ScD; Robert J. Glynn, ScD; Emily Y. Chew, MD; Christine M. Albert, MD; JoAnn E. Manson, MD Background: Observational epidemiologic studies indi- and visually significant AMD, defined as confirmed in- cate a direct association between homocysteine concentra- cident AMD with visual acuity of 20/30 or worse attrib- tion in the blood and the risk of age-related macular degen- utable to this condition. eration (AMD), but randomized trial data to examine the effect of therapy to lower homocysteine levels in AMD are Results:Afteranaverageof7.3yearsoftreatmentandfollow- lacking. Our objective was to examine the incidence of AMD up, there were 55 cases of AMD in the combination treat- in a trial of combined folic acid, pyridoxine hydrochloride ment group and 82 in the placebo group (relative risk, 0.66; (vitamin B6), and cyanocobalamin (vitamin B12) therapy. 95% confidence interval, 0.47-0.93 [P=.02]). For visually significant AMD, there were 26 cases in the combination Methods: We conducted a randomized, double-blind, treatment group and 44 in the placebo group (relative risk, placebo-controlled trial including 5442 female health care 0.59; 95% confidence interval, 0.36-0.95 [P=.03]). professionals 40 years or older with preexisting cardio- vascular disease or 3 or more cardiovascular disease risk Conclusions: These randomized trial data from a large factors. A total of 5205 of these women did not have a cohort of women at high risk of cardiovascular disease diagnosis of AMD at baseline and were included in this indicate that daily supplementation with folic acid, pyri- analysis. -

IV-23 N. Hydroxocobalamin (Cyanokit®)
N. Hydroxocobalamin (Cyanokit®) I. Classification •Cyanide antidote II. Actions •Binds cyanide ions with more affinity than hemoglobin molecule •Cyanide ion and hydroxocobalamin form cyanocobalamin (Vitamin B12) which is then excreted in the urine. III. Indications •Known or suspected cyanide poisoning - patients at high risk (industrial accidents, fire victims with smoke inhalation, known overdose, etc) with one more more of the following symptoms: - Altered mental status, confusion, seizures, coma - Headache - Chest pain or tightness - Shortness of breath, bradypnea, tachypnea - Hypertension (early), hypotension (late), cardiovascular collapse - Nausea, vomiting - Cardiac arrest - Mydriasis (dilated pupils) IV. Contraindications •Known allergic reaction to hydroxocobalamin or cyanocobalamin V. Adverse effects A. Cardiovascular •Ventricular extrasystoles •Tachycardia •Transient hypertension B. Neurological •Memory impairment •Dizziness •Restlessness C. Respiratory •Dyspnea •Dry Throat •Throat tightness D. Gastrointestinal •Abdominal discomfort •Dysphagia •Vomiting, diarrhea •Hematochezia E. General •Allergic reaction, pruritis, anaphylaxis •Hot flush SUBJECT : PATIENT CARE GUIDELINES AND STANDING ORDERS FOR BLS AND ALS UNITS REFERENCE NO. III-01 PUBLICATION : 1/11/21 IV-23 VI. Administration A. Do not administer hydroxocobalamin through the same IV site/set as the following medications: dopamine, fentanyl, dobutamine, diazepam, nitroglycerin, pentobarbital, propofol, thiopental, sodium thiosulfate, sodium nitrite and ascorbic acid. You must start a second IV to administer hydroxocobalamin in patient’s receiving these medications. B. Adult: •5 grams IV/IO over 15 minutes (Stocked as single 5gm bottle, or two 2.5 gm bottles) -Single 5 gm Bottle - Reconstituted with 200 ml Normal Saline. -Two 2.5 gm Bottles, give over 7.5 minutes each. - Each vial reconstituted with 100 ml Normal Saline. C. Pediatric •100 mg/kg IV/IO of hydroxocobalamin (reconstituted with Normal Saline the same as adults) over 15 minutes. -
Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Vitamin B12 Vitamin D Iodine and Selenium
Frequently Asked Questions for VEG 1 General 1. Why has VEG 1 been developed? VEG 1 was developed to provide a convenient way of avoiding the most common weak points in a varied vegan diet: vitamin B12, iodine, vitamin D and selenium. Vitamin B12 Vitamin B12 is almost entirely absent from modern plant foods which are not contaminated by bacteria and insects. Even unwashed, organically grown plants do not contain a significant amount of B12. Vegans often have intakes of vitamin B12 well below recommended intakes. Low vitamin B12 intake by vegans routinely leads to reduced activity of some important enzymes and increased levels of homocysteine and methylmalonic acid (MMA). Even moderately elevated homocysteine is associated with increased risk of death, depression, stroke, dementia and birth defects, though it remains unclear how many of these associations reflect true cause and effect. Vegans who do not get vitamin B12 from fortified food or supplements are at increased risk of clinical deficiency symptoms such as anaemia and nervous system damage. The most common early symptoms of vitamin B12 deficiency are tiredness (from anaemia), numbness and tingling (from nervous system damage) and sore tongue. VEG 1 is designed to provide sufficient absorbed vitamin B12 to match national and international recommended intakes. It is designed to be chewed as this increases the reliability of vitamin B12 absorption by dispersing and dissolving the tablet. Vitamin D In the winter – whenever our shadows at midday are more than twice as long as we are – our skin cannot produce vitamin D effectively and even small dietary intakes may become important to avoid deficiency. -

Cyanocobalamin-A Case for Withdrawal
686 Journal of the Royal Society of Medicine Volume 85 November 1992 Cyanocobalamin- a case for withdrawal: discussion paper A G Freeman MD FRCP Meadow Rise, 3 Lakeside, Swindon SN3 IQE Keywords: anaemia, pernicious; optic neuropathies; chronic cyanide intoxication; hydroxocobalamin; cyanocobalamin It seems evident that controversy still surrounds the reduced ability to detoxify the cyanide in the tobacco- treatment of pernicious anaemia and other vitamin smoke to which they are exposed'0. B12 deficiency disorders. The long quest for the 'anti- Patients with tobacco amblyopia who have normal pernicious anaemia factor' in the liver seemed to serum vitamin B12 levels need not continue therapy have ended in 1948 when pure cyanocobalamin was with intramuscular hydroxocobalamin once their isolated. This was found to be very active thera- visual acuity and visual fields have returned to peutically when given by intramuscular injection and normal providing they abstain from further smoking. was non-toxic in extremely high doses'. However, those patients who have low serum vitamin Lederle, in a recent commentary2, advocates that B12 levels or evidence of -defective vitamin B12 patients with pernicious anaemia should now be absorption will need to continue-indefinitely with treated with oral cyanocobalamin. He is not without hydroxocobalamin irrespective of their smoking support in that 40% of patients with pernicious habits as will all patients with pernicious anaemia anaemia in Sweden are being similarly treated3. and other vitamin B12 deficiency disorders who are He further states that such!- treatment is cheap at risk of developing- optic neuropathy if they and effective, produces clinical and haematological are smokers. -

Leucine Improved Growth Performance, Muscle Growth, And
cells Article Leucine Improved Growth Performance, Muscle Growth, and Muscle Protein Deposition Through AKT/TOR and AKT/FOXO3a Signaling Pathways in Hybrid Catfish Pelteobagrus vachelli × Leiocassis longirostris 1, 1, 1, 2,3 2,3 2,3 Ye Zhao y, Jin-Yang Li y, Qin Jiang y, Xiao-Qiu Zhou , Lin Feng , Yang Liu , Wei-Dan Jiang 2,3, Pei Wu 2,3, Jian Zhou 4, Juan Zhao 2 and Jun Jiang 1,3,* 1 College of Animal Science and Technology, Sichuan Agricultural University, Chengdu 611130, China; [email protected] (Y.Z.); [email protected] (J.-Y.L.); [email protected] (Q.J.) 2 Animal Nutrition Institute, Sichuan Agricultural University, Chengdu 611130, China; fi[email protected] (X.-Q.Z.); [email protected] (L.F.); [email protected] (Y.L.); [email protected] (W.-D.J.); [email protected] (P.W.); [email protected] (J.Z.) 3 Fish Nutrition and Safety Production University Key Laboratory of Sichuan Province, Sichuan Agricultural University, Chengdu 611130, China 4 Fisheries Institute of Sichuan Academy of Agricultural Science, Chengdu 611731, China; [email protected] * Correspondence: fi[email protected]; Tel.: +86-28-8629-1133 These authors contributed equally to this work. y Received: 25 October 2019; Accepted: 29 January 2020; Published: 30 January 2020 Abstract: (1) Background: l-leucine (Leu) plays a positive role in regulating protein turnover in skeletal muscle in mammal. However, the molecular mechanism for the effects of Leu on muscle growth and protein deposition is not clearly demonstrated in fish. This study investigated the effects of dietary Leu on growth performance and muscle growth, protein synthesis, and degradation-related signaling pathways of hybrid catfish (Pelteobagrus vachelli Leiocassis longirostris ). -

Hydroxocobalamin for Injection) for Intravenous Infusion Alternative Therapies, If Available, in Patients with Known Anaphylactic Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------CONTRAINDICATIONS----------------------------- These highlights do not include all the information needed to use None (4) CYANOKIT safely and effectively. See full prescribing information for CYANOKIT. ------------------------WARNINGS AND PRECAUTIONS----------------------- Risk of Anaphylaxis and Other Hypersensitivity Reactions: Consider CYANOKIT® (hydroxocobalamin for injection) for intravenous infusion alternative therapies, if available, in patients with known anaphylactic Initial U.S. Approval: 1975 reactions to hydroxocobalamin or cyanocobalamin. (5.2) Risk of Renal Injury: Acute renal failure with acute tubular necrosis, renal ----------------------------RECENT MAJOR CHANGES-------------------------- impairment and urine calcium oxalate crystals have been reported Warnings and Precautions, Risk of Renal Injury (5.3) 12/2018 following CYANOKIT therapy. Monitor renal function for 7 days Warnings and Precautions, Use of Blood Cyanide Assay (5.7) 12/2018 following CYANOKIT therapy. (5.3) Risk of Increased Blood Pressure: Substantial increases in blood pressure ----------------------------INDICATIONS AND USAGE--------------------------- may occur following CYANOKIT therapy. Monitor blood pressure during CYANOKIT is indicated for the treatment of known or suspected cyanide treatment. (5.4) poisoning. (1) -------------------------------ADVERSE REACTIONS------------------------------ ------------------------DOSAGE AND ADMINISTRATION---------------------- Most common -

Amino B12 Amino B12 and Erectile
Amino B12 Ingredients and Their Roles Glutamine 30mg/ml: Amino Acid Glutamine plays key roles in protein metabolism, cell volumizing, and anti-catabolism. Glutamine also increases your ability to secrete Human Growth Hormone, which helps metabolize body fat and support new muscle growth. Glutamine's anti-catabolism ability prevents the breakdown of your muscles. Arginine 100mg/ml + Ornithine 50mg/ml:Amino Acids Your body uses ornithine to synthesize arginine, then arginine is used to produce nitric oxide. Nitric oxide regulates smooth muscle contraction, which allows it to relax the muscles in blood vessels. Promotes vasodilation and blood flow. The amino acid ornithine is a perfectly-suited supplement to arginine. It is reduced Amino B12 and Erectile Dysfunction to arginine in the body, but this occurs very slowly, so that its effects last a long time. The combination of both amino acids improves the overall regeneration L-arginine improves blood flow. It does so by capability of the body and leads to a noticeable increase creating nitric oxide (NO), a gas that helps dilate in vitality. blood vessels. L-arginine has been shown to help people with heart disease or clogged arteries Lysine 50mg/ml: Amino Acid because of its vessel-widening abilities. Lysine is very important in the creation of carnitine, which converts fatty acids into energy and also lowers The same effect on blood vessels helps improve cholesterol levels. L-lysine also seems to play a role in symptoms of erectile dysfunction (ED). The L- absorbing calcium and helps the body form collagen, citrulline to NO path increases blood flow to a which aids in the growth and maintenance of bones and man’s genitals. -
Dietary Supplements Compendium Volume 1
2015 Dietary Supplements Compendium DSC Volume 1 General Notices and Requirements USP–NF General Chapters USP–NF Dietary Supplement Monographs USP–NF Excipient Monographs FCC General Provisions FCC Monographs FCC Identity Standards FCC Appendices Reagents, Indicators, and Solutions Reference Tables DSC217M_DSCVol1_Title_2015-01_V3.indd 1 2/2/15 12:18 PM 2 Notice and Warning Concerning U.S. Patent or Trademark Rights The inclusion in the USP Dietary Supplements Compendium of a monograph on any dietary supplement in respect to which patent or trademark rights may exist shall not be deemed, and is not intended as, a grant of, or authority to exercise, any right or privilege protected by such patent or trademark. All such rights and privileges are vested in the patent or trademark owner, and no other person may exercise the same without express permission, authority, or license secured from such patent or trademark owner. Concerning Use of the USP Dietary Supplements Compendium Attention is called to the fact that USP Dietary Supplements Compendium text is fully copyrighted. Authors and others wishing to use portions of the text should request permission to do so from the Legal Department of the United States Pharmacopeial Convention. Copyright © 2015 The United States Pharmacopeial Convention ISBN: 978-1-936424-41-2 12601 Twinbrook Parkway, Rockville, MD 20852 All rights reserved. DSC Contents iii Contents USP Dietary Supplements Compendium Volume 1 Volume 2 Members . v. Preface . v Mission and Preface . 1 Dietary Supplements Admission Evaluations . 1. General Notices and Requirements . 9 USP Dietary Supplement Verification Program . .205 USP–NF General Chapters . 25 Dietary Supplements Regulatory USP–NF Dietary Supplement Monographs . -

Adult BLS Standing Orders • Ensure EMS Provider Safety, Consider HAZMAT Activation
Imperial County Public Health Department Emergency Medical Services Agency Policy/Procedure/Protocol Manual Treatment Protocols Date: 07/01/2021 Poisoning/Intoxication/Envenomation - Adult Policy #9160A Adult BLS Standing Orders • Ensure EMS provider safety, consider HAZMAT activation. Recognize, Notify, Isolate • Universal Patient Protocol • Do not approach patient or location if scene safety is in question • Obtain accurate history of incident: o Name of product or substance o Quantity ingested, and/or duration of exposure o Time elapsed since exposure o If safe and accessible, bring medications or bottles to hospital • Move victim(s) to safe environment • Externally decontaminate - PRN • Continuously monitor ECG, blood pressure, pulse oximetry, and capnography (if ALS present) PRN • Give oxygen and provide airway support per Airway Policy • Contact Poison Control Center as needed 1 (800) 222-1222 Suspected Opioid Overdose with Respirations <12 RPM • If possible, avoid the use of a supraglottic device prior to the administration of naloxone • Administer naloxone 0.1 mg/kg, max of 2 mg IN. May repeat up to three (3) times, q5min • May assist family/friends on-scene with administration of patient’s own naloxone • NOTE - Use with caution in opioid dependent pain management patients • Assess vitals, with specific attention to respiratory rate and respiratory drive • Note pupil exam • Note drug paraphernalia or medication bottles near patient Suspected Stimulant Overdose with Sudden Hypoventilation, Oxygen Desaturation, or Apnea • High flow -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -
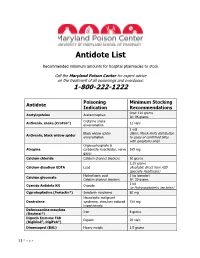
Antidote List
Antidote List Recommended minimum amounts for hospital pharmacies to stock Call the Maryland Poison Center for expert advice on the treatment of all poisonings and overdoses: 1-800-222-1222 Poisoning Minimum Stocking Antidote Indication Recommendations Oral: 120 grams Acetylcysteine Acetaminophen IV: 96 grams Crotaline snake Antivenin, snake (CroFab®) 12 vials envenomation 1 vial Black widow spider (Note: Merck limits distribution Antivenin, black widow spider envenomation to cases of confirmed bites with symptoms only) Organophosphate & Atropine carbamate insecticides, nerve 165 mg gases Calcium chloride Calcium channel blockers 10 grams 2.25 grams Calcium disodium EDTA Lead (Available direct from ASD Specialty Healthcare) Hydrofluoric acid 1 kg (powder) Calcium gluconate Calcium channel blockers IV: 30 grams 1 kit Cyanide Antidote Kit Cyanide (or Hydroxocobalamin, see below) Cyproheptadine (Periactin®) Serotonin syndrome 80 mg Neuroleptic malignant Dantrolene syndrome, stimulant-induced 720 mg hyperthermia Deferoxamine mesylate Iron 8 grams (Desferal®) Digoxin Immune FAB Digoxin 20 vials (Digibind®, DigiFab®) Dimercaprol (BAL) Heavy metals 1.5 grams 1 | P a g e Maryland Poison Center Antidote List – continued Poisoning Minimum Stocking Antidote Indication Recommendations DMSA (Succimer, Chemet®) Heavy metals 2000 mg Folic acid Methanol IV: 150 mg Flumazenil (Romazicon®) Benzodiazepines 10 mg Fomepizole (Antizol®) Ethylene glycol, methanol 12 grams Beta blockers, Glucagon 50 mg calcium channel blockers Hydroxocobalamin (Cyanokit®) Cyanide