Relationship Build Ing with First Nations and Public Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
October 2008
Volume 20 Issue 8 Published monthly by the Union of Ontario Indians - Anishinabek Nation Single Copy: $2.00 October 2008 IN BRIEF Saskatchewan first province Film school launched Treaty education mandatory TORONTO– With files from the Office of the Treaty Commis- Artist and film- The Leader-Post sioner (OTC) and the Federation maker Shirley REGINA – Saskatchewan be- of Saskatchewan Indian Nations Cheechoo has came the first province to imple- (FSIN). It came as a result of the fulfilled her ment mandatory treaty education 2007 Throne Speech, in which the dream of launch- on Sept. 15, which was also the provincial government commit- Shirley ing a film and ted to mandatory treaty education Cheechoo 134th anniversary of the signing television train- of Treaty 4. for children from kindergarten ing centre for Native youth Under the new agreement, ev- through to Grade 12. and people of diversity. The ery student in the province will be Speaking for the 42 member Weengushk Film Institute educated about the true meaning communities of the Anishinabek will be located on Manitoulin of the treaties and what it means to Nation, Grand Council Chief Beau- Island. be treaty people. cage applauded the Saskatchewan “This is exactly what we’d initiative, but said it shouldn’t have like to see happening in our ter- taken the establishment of a treaty Fire funding ritory and across Canada,” said commission to make it happen. Anishinabek Nation Grand Coun- “The Ipperwash Inquiry rec- out of date cil Chief John Beaucage. “Un- ommendations call for the estab- By Margaret Hele less today’s students who will be lishment of a treaty commission SAULT STE. -

March 7, 2017 Minutes
COUNCIL MEETING MINUTES Tuesday, March 7, 2017: Nbisiing S.S. - Duchesnay: 6:00 pm Present: Chief Scott Mcleod Deputy Chief Muriel Sawyer Councillors June Commanda Rick Stevens Brian Couchie Jason Laronde Chief Executive Officer Dwayne Nashkawa Executive Assistant Mike Sawyer Guest Brian Young Joel Girard Lorraine Liberty Carol Guppy Tracey Restoule Mathilde Bazinet Sandy Graham Regrets: Councillor Cathy Bellefeuille (Personal) Councillor Corey Goulais (Mtg in Sault Ste. Marie) 1. Meeting commenced at 6:02p.m. 2. ADJOURNMENT TO THE COMMITTEE OF THE WHOLE: MOVED BY June Commanda SECONDED BY Rick Stevens to adjourn to the committee of the whole. CARRIED. ** Adjourned to the committee of the whole at 6:03pm ** Community member gave~ presentation to Council to offer a solution to saving the red pine plantations on Radar Rd and Dump Rd. that was planted 30 years ago. To provide proper thinning to allow these plantations to grow properly and maintain sustainability, with no cost to Nipissing First Nation. MOVED BY Rick Stevens SECONDED BY Brian Couchie to direct staff to work with Young Forestry to carry out Red Pine Thinning on Nipissing First Nation reserve lands. CARRIED. MOVED BY Muriel Sawyer SECONDED BY Jason Laronde to adjourn the committee ofthe whole. CARRIED. ** Committee of the whole adjourned at 6:28pm ** 3. ADOPTION OF COUNCIL AGENDA: Additions to agenda: • Item 7. (f) Chiefs Report MOVED BY Brian Couchie SECONDED BY Jason Laronde to approve the Council Agenda of March 7, 2017 as amended. CARRIED. 1 Counc1·1 Meetmg . M"mutes '--" Nipissing First Nation March 7, 2017 4. DISCLOSURES OF CONFLICT: None. -

Casino Rama Split Goes to Mediation
Volume 17 Issue 1 Published monthly by the Union of Ontario Indians - Anishinabek Nation Single Copy: $2.00 Jan-Feb 2005 IN THE Bill would create revenue-sharing framework SAULT STE. MARIE (CP) — Native leaders say the bill would territories.” mittee stage. That the Liberal gov- NEWS The head of the Assembly of First give bands a framework to secure As employers go looking for ernment has allowed the bill to get Nations is applauding an Ontario revenue-sharing agreements with labour and the country faces a short- that far is “momentous,” said Premier’s slurs private-member’s bill that would players in industries such as forestry, age of skilled workers, aboriginal Bisson. FREDERICTON (CP) – help Natives get a share of the mining and even tourism. communities need to be able to “The reason I think they allowed The latest round of insults in money made from natural resources Efforts like these are part of revi- establish appropriate training sys- it to happen is the government gen- New Brunswick’s legislature on their traditional lands. talizing First Nations economies so tems to fill those positions, Fontaine uinely wants, I think, to measure the has prompted a request from The bill, put forward by provin- that they can provide workers to said. response of the public,” said the the Speaker of the House for cial NDP native affairs critic Gilles benefit the general economy, said “You look at (First Nations) MPP for Timmins-James Bay. more respect. Speaker Bev Bisson, aims to create an equitable Phil Fontaine, National Chief of the unemployment rates at 40 to 90 per When the legislature resumes on Harrison met with Premier way for First Nations in northern Assembly of First Nations. -
Notice of Commencement of Terms of Reference
Notice of Submission of Terms of Reference Detour Lake Permanent Power Project Detour Gold Canada Corporation As part of the planning process for the Detour Lake Permanent Power Project, a Terms of Reference was submitted to the Ministry of the Environment for review as required under the Environmental Assessment Act. If approved, the Terms of Reference will serve as a framework for the preparation and review of the Environmental Assessment for the proposed undertaking. This Environmental Assessment process for approval of the main power supply is one of several environmental assessment processes required to be completed for the Detour Lake Project to be approved. The Detour Lake Project is a proposed open pit gold mine with related processing facilities and infrastructure, to be developed northeast of Cochrane, Ontario at the location of a previously operating mine. The Project is anticipated to be a significant contributor to the local economy. Consultation on the Detour Lake Project was initiated in 2007. While these are separate approvals for different components of the mine development, Detour Gold Corporation will coordinate public consultation opportunities wherever possible. You may inspect the proposed Terms of Reference during normal business hours at the following locations: Ministry of Natural Resources Min. of Northern Development, Mines and Forestry 2 Third Avenue 33 Ambridge Drive Cochrane, ON P0L 1C0 Iroquois Falls, ON P0K 1G0 705-272-4365 705-232-4660 Moosonee Municipal Office Smooth Rock Falls Municipal Office 5 First Street 142 First Avenue Moosonee, ON P0L 1Y0 Smooth Rock Falls, ON P0L 1B0 705-336-2993 705-338-2717 Ministry of the Environment Timmins Public Library Timmins District Office, Hwy 101 East 320 Second Avenue South Porcupine, ON P0N 1H0 Timmins, ON P4N 8A4 705-235-1500 / 1-800-380-6615 705-360-2623 Ministry of the Environment Detour Gold Corporation Environmental Assessment & Approvals Branch Royal Bank Plaza, North Tower 2 St. -

20-24 October 14'20 Meeting
THE CORPORATION OF THE MUNICIPALITY OF HURON SHORES October 14, 2020 (20-24) - Regular The regular meeting of the Council of the Corporation of the Municipality of Huron Shores was held on Wednesday, October 14, 2020, and called to order by Mayor Georges Bilodeau at 7:44 p.m. PRESENT (Council Chambers): Mayor Georges Bilodeau, and Councillors Debora Kirby and Jock Pirrie PRESENT (electronically): Councillors Jane Armstrong, Gord Campbell, Nancy Jones-Scissons, Blair MacKinnon (lost connection from 7:17 - 7:20 p.m., and 8:38 - 8:55 p.m.), and Dale Wedgwood REGRETS: Councillor Darlene Walsh STAFF (Council Chambers): Clerk/Administrator Deborah Tonelli STAFF (electronically): Deputy Clerk Natashia Roberts, and Treasurer John Stenger (left meeting when Council went into closed session) DELEGATION (electronically): GALLERY (electronically): Joanne Falk (left shortly after Council returned to open session); Dan Gray (left when Council went into closed session); Peter Tonazzo (left at 8:11 p.m.); Jim Falconer (left when Council went into into closed session); Cornelia Poeschl (left at approximately 8:20 p.m.); Nancy Richards (left when Council went into closed session); David Ratz (left when Council went into closed session), Dave Smith (left when Council went into closed session) AGENDA REVIEW No changes made. DECLARATION OF PECUNIARY INTEREST Councillor Wedgwood declared a pecuniary interest respecting Item 5, pertaining to the Hughes Supply account. Councillor Kirby declared a pecuniary interest respecting Item 5, pertaining to the Tulloch Engineering account and Item 8b-1 (declared at the time the item came up for discussion on the agenda). Councillor Armstrong declared a pecuniary interest respecting Items 5, pertaining to the Armstrong Enterprise account, and Item 8d-2. -
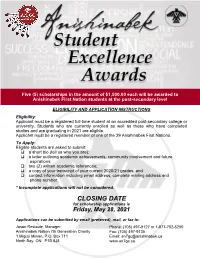
How to Apply
Five (5) scholarships in the amount of $1,500.00 each will be awarded to Anishinabek First Nation students at the post-secondary level ELIGIBILITY AND APPLICATION INSTRUCTIONS Eligibility: Applicant must be a registered full-time student at an accredited post-secondary college or university. Students who are currently enrolled as well as those who have completed studies and are graduating in 2021 are eligible. Applicant must be a registered member of one of the 39 Anishinabek First Nations. To Apply: Eligible students are asked to submit: a short bio (tell us who you are); a letter outlining academic achievements, community involvement and future aspirations; two (2) written academic references; a copy of your transcript of your current 2020/21 grades; and contact information including email address, complete mailing address and phone number. * Incomplete applications will not be considered. CLOSING DATE for scholarship applications is Friday, May 28, 2021 Applications can be submitted by email (preferred), mail, or fax to: Jason Restoule, Manager Phone: (705) 497-9127 or 1-877-702-5200 Anishinabek Nation 7th Generation Charity Fax: (705) 497-9135 1 Migizii Miikan, P.O. Box 711 Email: [email protected] North Bay, ON P1B 8J8 www.an7gc.ca Post-secondary students registered with the following Anishinabek First Nation communities are eligible to apply Aamjiwnaang First Nation Moose Deer Point Alderville First Nation Munsee-Delaware Nation Atikameksheng Anishnawbek Namaygoosisagagun First Nation Aundeck Omni Kaning Nipissing First Nation -
Reliability Performance Overview February 21, 2018 Agenda
First Nations – Reliability Performance Overview February 21, 2018 Agenda Hydro One Operations Review Historical Reliability Performance First Nations Communities Supply 2017 Transmission Reliability Transmission Reliability Improvements 2017 Distribution Reliability Distribution Grid Modernization Planned Work on Assets Serving First Nations Communities 2 Privileged and Confidential – Internal Use Only TOR 170419 Operations Performance ... HYDRO ONE OPERATIONS REVIEW 1005 Distribution Stations 3 Privileged and Confidential – Internal Use Only TOR 170419 Operations Performance ... First Nations Communities Supply Distribution Lines - “Feeders” Generating Step-Up Transmission Step-down Distribution Customer Station Lines Transmission Transformer Stations (First Nation Stations Communities) First Nations Communities: Supplied from 68 Transmission Lines, 59 Transmission Delivery Points and 109 Distribution Feeders 4 4 Privileged and Confidential – Internal Use Only TOR 170419 Operations Performance ... 2017 Transmission System Reliability Performance 2017 Year End Overall Transmission Performance: SAIDI was 42.8 min and SAIFI was 1.1 interruptions per customer delivery point. Main causes of these interruptions are 1) Weather 2) Defective Equipment and 3) Unconfirmed 5 Privileged and Confidential – Internal Use Only TOR 170419 Operations Performance ... Tx System – Primary Causes of Interruptions: (~66% from Weather & Equipment Failures) Power outage causes (2017) Weather 48% Adverse weather (freezing rain, ice, lightning) Equipment -

Appendix a IAMGOLD Côté Gold Project Aboriginal Consultation Plan (Previously Submitted to the Ministry of Northern Development and Mines in 2013
Summary of Consultation to Support the Côté Gold Project Closure Plan Côté Gold Project Appendix A IAMGOLD Côté Gold Project Aboriginal Consultation Plan (previously submitted to the Ministry of Northern Development and Mines in 2013 Stakeholder Consultation Plan (2013) TC180501 | October 2018 CÔTÉ GOLD PROJECT PROVINCIAL INDIVIDUAL ENVIRONMENTAL ASSESSMENT PROPOSED TERMS OF REFERENCE APPENDIX D PROPOSED STAKEHOLDER CONSULTATION PLAN Submitted to: IAMGOLD Corporation 401 Bay Street, Suite 3200 Toronto, Ontario M5H 2Y4 Submitted by: AMEC Environment & Infrastructure, a Division of AMEC Americas Limited 160 Traders Blvd. East, Suite 110 Mississauga, Ontario L4Z 3K7 July 2013 TABLE OF CONTENTS PAGE 1.0 INTRODUCTION ............................................................................................................ 1-1 1.1 Introduction ......................................................................................................... 1-1 1.2 Provincial EA and Consultation Plan Requirements ........................................... 1-1 1.3 Federal EA and Consultation Plan Requirements .............................................. 1-2 1.4 Responsibility for Plan Implementation .............................................................. 1-3 2.0 CONSULTATION APPROACH ..................................................................................... 2-1 2.1 Goals and Objectives ......................................................................................... 2-1 2.2 Stakeholder Identification .................................................................................. -

Administrative ,,, / Report
ADMINISTRATIVE ,,, / REPORT,., Administration Department Public Document Yes No TIS" SUBJECT: Indigenous Engagement Framework and 2020 Report Back on Progress RECOMMENDATION: That Council approve the Indigenous Engagement Framework and accept the 2020 Report Back on Progress EXPLANATION: In 2019, Council approved the draft Indigenous Engagement Framework. Direction was provided to turn the draft document into Report and to report back on activities. The COVID- 19 global pandemic interrupted a number of activities in 2020. For example, the Mushkegowuk Cup was postponed and the inability to meet face-to-face led to the cancellation of a many of meetings of the City of Timmins Indigenous Advisory Committee. Be that as it may, much progress was made in a number of strategic areas. Addressing Human Needs: Worked collaboratively with the Cochrane DSSAB, Living Space and Northern College to ensure the safest possible shelter services were available during the pandemic. Lobbied senior levels of government for support for the Mushkegowuk Council' s Fire Keepers Street Outreach application for funding. Worked collaboratively with the Timmins Native Friendship Centre and Living Space to ensure adequate winter shelter services and cold weather alerts during 2019-20. Timmins hosted 166 evacuees for a seventeen day period in August from Fort Hope, ensuring COVID- 19 protocols were in place including 24/7 on site nurses and access to a physician. Timmins supported the development of the Kanachihih Youth Treatment Centre. Delivering on the Calls to Action The Indigenous Advisory Committee met throughout the year, with a hiatus during the state of emergency and lockdown. COT —HR -035( F4) -v05 Revised: March 31. -

Community Profiles for the Oneca Education And
FIRST NATION COMMUNITY PROFILES 2010 Political/Territorial Facts About This Community Phone Number First Nation and Address Nation and Region Organization or and Fax Number Affiliation (if any) • Census data from 2006 states Aamjiwnaang First that there are 706 residents. Nation • This is a Chippewa (Ojibwe) community located on the (Sarnia) (519) 336‐8410 Anishinabek Nation shores of the St. Clair River near SFNS Sarnia, Ontario. 978 Tashmoo Avenue (Fax) 336‐0382 • There are 253 private dwellings in this community. SARNIA, Ontario (Southwest Region) • The land base is 12.57 square kilometres. N7T 7H5 • Census data from 2006 states that there are 506 residents. Alderville First Nation • This community is located in South‐Central Ontario. It is 11696 Second Line (905) 352‐2011 Anishinabek Nation intersected by County Road 45, and is located on the south side P.O. Box 46 (Fax) 352‐3242 Ogemawahj of Rice Lake and is 30km north of Cobourg. ROSENEATH, Ontario (Southeast Region) • There are 237 private dwellings in this community. K0K 2X0 • The land base is 12.52 square kilometres. COPYRIGHT OF THE ONECA EDUCATION PARTNERSHIPS PROGRAM 1 FIRST NATION COMMUNITY PROFILES 2010 • Census data from 2006 states that there are 406 residents. • This Algonquin community Algonquins of called Pikwàkanagàn is situated Pikwakanagan First on the beautiful shores of the Nation (613) 625‐2800 Bonnechere River and Golden Anishinabek Nation Lake. It is located off of Highway P.O. Box 100 (Fax) 625‐1149 N/A 60 and is 1 1/2 hours west of Ottawa and 1 1/2 hours south of GOLDEN LAKE, Ontario Algonquin Park. -

FINAL 2009 Annual Report
NEOnet 2009 Annual Report Infrastructure Enhancement Application Education and Awareness 2009 Annual Report Table of Contents Message from the Chair ..............................................................................................2 Corporate Profile........................................................................................................3 Mandate ....................................................................................................................3 Regional Profile ..........................................................................................................4 Catchment Area.......................................................................................................................................................5 NEOnet Team .............................................................................................................6 Organizational Chart..............................................................................................................................................6 Core Staff Members...............................................................................................................................................7 Leaving staff members..........................................................................................................................................8 Board of Directors ..................................................................................................................................................9 -

Indigenous Peoples' Advisory Committee Minutes of The
INDIGENOUS PEOPLES’ ADVISORY COMMITTEE MINUTES OF THE MEETING HELD Friday, November 9, 2018 @ 11:00 a.m. Schumacher Board Office – with v/c to NLBO Committee Members Present: Howard Archibald - First Nations Trustee – DSB Ontario North East and Chair of IPAC Arline Chasle - Director of Education, Timiskaming First Nation (v/c from New Liskeard Board Office) Rose Thomas - Education Officer, Matachewan First Nation t/c Neil Iserhoff - Education Director, Taykwa Tagamou Nation Cathy Naveau - Education Director, Mattagami First Nation Saunders Porter - Trustee, DSB Ontario North East Rosemary Pochopsky - Acting Chair for today and Trustee, DSB Ontario North East Committee Members Absent: Lynn Mongrain - Representative, Temagami First Nation (teleconference) James McGrogan - Incoming Director of Education, Wahgoshig First Nation Administration Present: Lesleigh Dye - Director of Education, District School Board Ontario North East Pearl Fong-West - Superintendent of Business and Finance Lisa Innes - Vice Principal, Indigenous Education Administration Absent: Resource Persons & Guests Present Anne Commando-Dube - Education Partnership Liaison, Wabun Tribal Council Audrey McLaren - Education Partnership Coordinator, Timiskaming First Nation(v/c from New Liskeard Board Office) Doug Shearer - Trustee, DSB Ontario North East Resource Persons & Regular Guests -Absent Bernice Brunette - Executive Director, Ininew Indian Friendship Centre, Cochrane Chris McKay - Wawatay FN James Wesley - Director of Education, Kashechewan First Nation Derek McKay -