PDF File, and Attaches the File to the Referral Email
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recreational Noise-Induced Hearing Loss
Hearing loss due to recreational exposure to loud sounds A review World Health Organization Hearing loss due to recreational exposure to loud sounds A review World Health Organization Contributors: Etienne Krug, Maria Alarcos Cieza, Shelly Chadha, Laura Sminkey, Thais Morata, DeWet Swanepoel, Adrian Fuente, Warwick Williams, Joseph Cerquone, Ricardo Martinez, Gretchen Stevens, Margie Peden, Sowmya Rao, Paras Agarwal, Eighmey Zeeck, Anna Bladey, Malachi Arunda, Aileen Ncube. Graphics Credits: INIS Communications WHO Library Cataloguing-in-Publication Data Hearing loss due to recreational exposure to loud sounds: a review. 1.Hearing Loss, Noise-Induced. 2.Music. 3.Noise. 4.Recreation. 5.Noise. Transportation. 6.Adolescent. I.World Health Organization. ISBN 978 92 4 150851 3 (NLM classification: WV 270) © World Health Organization 2015 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for non- commercial distribution – should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Can Other People Hear the Noise in My Ears? Not Usually, but Sometimes They Are Able to Hear a (Ertant Type Oftinnitus
Not at all. Tinnitus is the name for these head noises, and they are very common. Nearly 36 million Americans suffer from this discomfort. Tinnitus mav come and go, or you may be aware of a continuous sound. It can vary in pitch from a low roar to a high squeal or whine, and you may hear it in one or both ears. When the ringing is constant, It can be annoying and distracting. More than seven million people are afflicted so severely that they cannot lead normal lives. Can other people hear the noise in my ears? Not usually, but sometimes they are able to hear a (ertant type oftinnitus. This is called objective tinnitus, and it is caused either by abnormalities in blood vessels around the outside of the ear or by muscle spasms, which may sound like clicks or crackling illside the middle ear. There are many causes for subjective tinnitus, the nOlSC only you can hear. Some causes are not serious (a small plug of wax in the ear canal might cause temporary tinnitus). Tinnitus can also be a symptom of more serious middle ear problems such as infection, a hole in the eardrum, an accumulation of fluid, or stiffening (otosclerosis) of the middle ear bones. Tinnitus may also be caused by allergy, high or 10\V blood pressure (blood circulation problems), OUTER EAR MIDDLE EAR INNER EAR \ a tumor, diabetes, thyroid problems, injury to the head or neck, and a variety of other causes including medications such as anti-inflammatories, antibiotics, sedatives/antidepressants, and aspirin. -
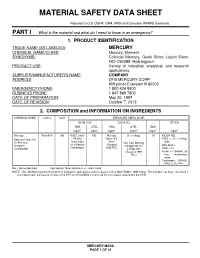
Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION TRADE NAME (AS LABELED) : MERCURY CHEMICAL NAME/CLASS : Mercury; Element SYNONYMS: Colloidal Mercury, Quick Silver; Liquid Silver; NCI-C60399; Hydrargyrum PRODUCT USE : Variety of industrial, analytical, and research applications. SUPPLIER/MANUFACTURER'S NAME : COMPANY ADDRESS : DFG MERCURY CORP 909 pitner Evanston Ill 60202 EMERGENCY PHONE : 1 800 424 9300 BUSINESS PHONE : 1 847 869 7800 DATE OF PREPARATION : May 20, 1997 DATE OF REVISION : October 7, 2013 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # %w/w EXPOSURE LIMITS IN AIR ACGIH-TLV OSHA-PEL OTHER TWA STEL TWA STEL IDLH mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 Mercury 7439-97-6 100 0.025, (skin) NE Mercury 0.1 (ceiling) 10 NIOSH REL: Exposure limits are A4 (Not Vapor: 0.5, STEL = 0.1 (ceiling, for Mercury, Classifiable Skin; Non-alkyl Mercury skin) Inorganic as a Human (Vacated Compounds: 0.1 DFG MAKs: Compounds Carcinogen) 1989 PEL) Ceiling, skin TWA = 0.1 (Vacated 1989 PEAK = 10 •MAK 30 PEL) min., momentary value Carcinogen: EPA-D; IARC-3, TLV-A4 NE = Not Established. See Section 16 for Definitions of Terms Used. NOTE: ALL WHMIS required information is included in appropriate sections based on the ANSI Z400.1-1998 format. This product has been classified in accordance with the hazard criteria of the CPR and the MSDS contains all the information required by the CPR. -

Hearing Loss
Integrated care for older people (ICOPE) Guidelines on community-level interventions to manage declines in intrinsic capacity Evidence profile: hearing loss Scoping question: Does case finding and provision of hearing aids or assistive listening devices produce any benefit or harm for older people 60 years of age and over with hearing loss? The full ICOPE guidelines and complete set of evidence profiles are available at who.int/ageing/publications/guidelines-icope Painting: “Wet in Wet” by Gusta van der Meer. At 75 years of age, Gusta has an artistic style that is fresh, distinctive and vibrant. A long-time lover of art, she finds that dementia is no barrier to her artistic expression. Appreciated not just for her art but also for the support and encouragement she gives to other artists with dementia, Gusta participates in a weekly art class. Copyright by Gusta van der Meer. All rights reserved Evidence profile: hearing loss Contents Background ....................................................................................................................................................................................................... 1 Part 1: Evidence review .................................................................................................................................................................................... 2 Scoping question in PICO format (population, intervention, comparison, outcome) ............................................................................................. 2 Search strategy -

Tinnitus: Ringing in the SYMPTOMS Ears
Tinnitus: Ringing in the SYMPTOMS Ears By Vestibular Disorders Association TINNITUS WHAT IS TINNITUS? An abnormal noise perceived in one or both Tinnitus is abnormal noise perceived in one or both ears or in the head. ears or in the head. It Tinnitus (pronounced either “TIN-uh-tus” or “tin-NY-tus”) may be can be experienced as a intermittent, or it might appear as a constant or continuous sound. It can ringing, hissing, whistling, be experienced as a ringing, hissing, whistling, buzzing, or clicking sound buzzing, or clicking sound and can vary in pitch from a low roar to a high squeal. and can vary in pitch. Tinnitus is very common. Most studies indicate the prevalence in adults as falling within the range of 10% to 15%, with a greater prevalence at higher ages, through the sixth or seventh decade of life. 1 Gender distinctions ARTICLE are not consistently reported across studies, but tinnitus prevalence is significantly higher in pregnant than non-pregnant women. 2 The most common form of tinnitus is subjective tinnitus, which is noise that other people cannot hear. Objective tinnitus can be heard by an examiner positioned close to the ear. This is a rare form of tinnitus, 068 occurring in less than 1% of cases. 3 Chronic tinnitus can be annoying, intrusive, and in some cases devastating to a person’s life. Up to 25% of those with chronic tinnitus find it severe DID THIS ARTICLE enough to seek treatment. 4 It can interfere with a person’s ability to hear, HELP YOU? work, and perform daily activities. -

Understanding Mesothelioma a Guide for People with Cancer, Their Families and Friends
Understanding Mesothelioma A guide for people with cancer, their families and friends Cancer information For information & support, call Understanding Mesothelioma A guide for people with cancer, their families and friends First published as Understanding Pleural Mesothelioma June 2015. This edition May 2017. © Cancer Council Australia 2017. ISBN 978 1 921041 89 1 Understanding Mesothelioma is reviewed approximately every two years. Check the publication date above to ensure this copy is up to date. Editor: Jenni Bruce. Designer: Paula Marchant. Printer: SOS Print + Media Group. Acknowledgements This edition has been developed by Cancer Council NSW on behalf of all other state and territory Cancer Councils as part of a National Publications Working Group initiative. We thank the reviewers of this booklet: Dr Steven Kao, Medical Oncologist, Chris O’Brien Lifehouse, NSW; Theodora Ahilas, Principal, Maurice Blackburn Lawyers, NSW; Prof David Ball, Director, Lung Service, Peter MacCallum Cancer Centre, VIC; Cely Benchoam, Consumer; Prof Kwun Fong, Thoracic Physician, University of Queensland Thoracic Research Centre, The Prince Charles Hospital, QLD; Victoria Keena, Executive Officer, Asbestos Diseases Research Institute, NSW; Angela Kyttaridis, Social Worker, Concord Repatriation General Hospital, NSW; Dr Judith Lacey, Head of Supportive Care and Integrative Medicine, Chris O’Brien Lifehouse, NSW; Amanda Maple, 13 11 20 Consultant, Cancer Council SA; A/Prof Brian McCaughan, Thoracic Surgeon, Sydney Cardiothoracic Surgeons, Strathfield Private Hospital and University of Sydney, NSW; Jocelyn McLean, Mesothelioma Support Coordinator, Asbestos Diseases Research Institute, NSW; Kirsten Mooney, Thoracic Cancer Nurse Coordinator, WA Cancer and Palliative Care Network, Department of Health, WA; Prof David Morris, University of New South Wales, Department of Surgery, St George Public Hospital, NSW; Rod Smith, Awareness and Support Co-ordinator, Bernie Banton Foundation. -

The Nervous System – Target Organ Into the Twenty-First Century
The Nervous System – Target Organ into the Twenty-First Century R. Douglas Hamm MD, CCFP, FRCPC (Occ Med), FCBOM President, Canadian Board of Occupational Medicine CONTENTS 1. WHY NEURONS MAKE GOOD TARGETS FOR OCCUPATIONAL TOXICANTS 2. FROM CLASSICAL PLUMBISM TO BEHAVIORAL TOXICOLOGY 3. TOXICOKINETICS, COMPARTMENTS, AND PBPK MODELS 4. THE DIVERSE TOXICODYNAMICS OF THE NERVOUS SYSTEM 1. Peripheral Neurons (neuronopathy, axonopathy, myelinopathy) 2. Synaptic Neurotransmission (cholinergic pathways) 3. Special Senses (visual, auditory, olfactory) 4. Movement Disorders (parkinsonism, ataxia, tremor) 5. Neuroaffective and Neurocognitive Effects 5. NOTEWORTHY OCCUPATIONAL NEUROTOXICANTS 1. “Heavy metals” (Pb, Hg, Tl) and other elements (Mn, As, Al, Sb, Te) 2. Organic Solvents (toluene, xylene, styrene, C2HCl3, C2Cl4, CH3CCl3, CS2) 3. Gases (HCN, CO, H2S, ethylene oxide) 4. Pesticides (organophosphates, carbamates, organochlorines, pyrethroids, neonicotinoids) 6. CLINICAL NEUROTOXICOLOGY 1. Identification of Occupational Neurotoxic Disorders 2. Biomarkers of Exposure and Effect 3. Clinical Investigations of Neurotoxicity 1. WHY NEURONS MAKE GOOD 2. FROM CLASSICAL PLUMBISM TO TARGETS FOR OCCUPATIONAL BEHAVIORAL TOXICOLOGY TOXICANTS Hippocrates (c. 460-370 BC) has been cited as Neuroanatomical structures have large surface the first ancient author to describe a case of areas and receptor populations, e.g., the occupational neurotoxicity but this has been surface area of the brain’s 100 billion neurons shown to be erroneous (Osler, 1907; Waldron, totals hundreds of square metres. 1973, 1978; Skrabanek, 1986; Vance, 2007). The earliest report appears to be that of Neurons have high rates of metabolism, e.g., Nicander of Colophon (2nd cent. BC) who the brain at 2% body mass consumes 20% of observed that in “psimuthion” i.e. -

Croet 2001 Annual Report
PuttingCROET science to work for working Oregonians CROET 2001 ANNUAL REPORT Where Healing, Teaching and Discovery Come Together Mission, Purpose, and Table of Contents Mandate CROET, the Center for Research on Occupational and Overview . 2 Environmental Toxicology at OHSU, is dedicated to Mission, Purpose, and Mandate the promotion of health and safety in the workforce. Through basic and applied research, education, and Message from the Director . 3 outreach, CROET seeks to prevent disease and disability among working Oregonians and their CROET — A Resource for Oregon . 4 families, during their employment years and throughout retirement. Advisory Committees . 5 CROET’s Areas of Emphasis . 6 2001 CROET Highlights . 7-9 Financial Summary . 10 Staff and Contact Information . 11 2 Message from the Director Dear Fellow Oregonians, “CROET - Putting Science to Work for Working Oregonians!” Many will have heard this message broadcast over public radio in an effort to increase awareness among Oregonians of the treasure trove of talent and information available to Oregonians through CROET at OHSU. This simple message proved most effective as judged by the dramatic increase in use of our information-packed website, www.croetweb.com. There are many other messages that CROET wishes to broadcast, but time and space are always limited. We have used this report to illustrate some of the basic mechanistic and applied workplace research initiatives that are underway at CROET. Brief study of our Financial Summary reveals the various research activities that are supported by workers’ compensation funds and leveraged federal grant support. On average, a single Oregon dollar leverages four federal dollars for basic and applied research at CROET! This speaks to the quality of CROET’s scientists and staff in competing successfully for highly competitive research dollars from federal agencies such as the National Institutes of Health (NIH). -

Active Symptom Control with Or Without Chemotherapy in the Treatment of Patients with Malignant Pleural Mesothelioma (MS01): a Multicentre Randomised Trial
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Articles Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial Martin F Muers, Richard J Stephens, Patricia Fisher, Liz Darlison, Christopher M B Higgs, Erica Lowry, Andrew G Nicholson, Mary O’Brien, Michael Peake, Robin Rudd, Michael Snee, Jeremy Steele, David J Girling, Matthew Nankivell, Cheryl Pugh, Mahesh K B Parmar, on behalf of the MS01 Trial Management Group* Summary Background Malignant pleural mesothelioma is almost always fatal, and few treatment options are available. Although Lancet 2008; 371: 1685–94 active symptom control (ASC) has been recommended for the management of this disease, no consensus exists for See Comment page 1640 the role of chemotherapy. We investigated whether the addition of chemotherapy to ASC improved survival and *Members listed at end of paper quality of life. Leeds General Infi rmary, Leeds, UK (M F Muers FRCP); MRC Methods 409 patients with malignant pleural mesothelioma, from 76 centres in the UK and two in Australia, were Clinical Trials Unit, London, UK (R J Stephens, D J Girling FRCP, randomly assigned to ASC alone (treatment could include steroids, analgesic drugs, bronchodilators, palliative M Nankivell MSc, radiotherapy [n=136]); to ASC plus MVP (four cycles of mitomycin 6 mg/m², vinblastine 6 mg/m², and cisplatin C Pugh BSc Hons, 50 mg/m² every 3 weeks [n=137]); or to ASC plus vinorelbine (one injection of vinorelbine 30 mg/m² every week for Prof M K B Parmar DPhil); 12 weeks [n=136]). -

Muscular Tension and Tinnitus
MARJA ESTOLA-PARTANEN Muscular Tension and Tinnitus An Experimental Trial of Trigger Point Injections on Tinnitus University of Tampere Tampere 2000 ACADEMIC DISSERTATION University of Tampere, Medical School Tampere University Hospital, Department of Otorhinolaryngology Finland Supervised by Reviewed by Docent Tapani Rahko Professor Kalevi Jokinen University of Tampere University of Oulu Professor Ilmari Pyykkö Karolinska Institutet Distribution University of Tampere Tel. +358 3 215 6055 Sales Office Fax +358 3 215 7150 P. O. B o x 617 [email protected] 33101 Tampere http://granum.uta.fi Finland Cover design by Juha Siro Illustration Hannu Tapiovaara Printed dissertation Electronic dissertation Acta Universitatis Tamperensis 782 Acta Electronica Universitatis Tamperensis 75 ISBN 951-44-4965-7 ISBN 951-44-4972-X ISSN 1455-1616 ISSN 1456-954X http://acta.uta.fi Vammalan Kirjapaino Oy Vammala 2000 MARJA ESTOLA-PARTANEN Muscular Tension and Tinnitus An Experimental Trial of Trigger Point Injections on Tinnitus ACADEMIC DISSERTATION To be presented, with the permission of the Faculty of Medicine of the University of Tampere, for public discussion in the main auditorium of Building K, Medical School of the University of Tampere, Teiskontie 35, Tampere, on December 8th, 2000, at 12 o’clock. University of Tampere Tampere 2000 INDEX A. ABBREVIATIONS B. INTRODUCTION C. REVIEW OF LITERATURE 1. DEFINITION OF TINNITUS 2. CHARACTERIZATION OF TINNITUS 2.1. Characterization by patient description 2.2. Characterization with audiometer 2.2.1. Pitch 2.2.2. Loudness 2.2.3. Masking abilities 2.3. Characterization with VAS-scale 2.4. Inconvenience caused by tinnitus 2.5. Objective measurements of tinnitus 3. -

Analysis of Chronic Tinnitus in Noise-Induced Hearing Loss and Presbycusis
Journal of Clinical Medicine Article Analysis of Chronic Tinnitus in Noise-Induced Hearing Loss and Presbycusis Hee Jin Kang 1, Dae Woong Kang 1, Sung Su Kim 2, Tong In Oh 3 , Sang Hoon Kim 1 and Seung Geun Yeo 1,* 1 Department of Otolaryngology-Head & Neck Surgery, School of Medicine, Kyung Hee University, Seoul 02447, Korea; [email protected] (H.J.K.); [email protected] (D.W.K.); [email protected] (S.H.K.) 2 Medical Research Center for Bioreaction to Reactive Oxygen Species and Biomedical Science Institute, School of Medicine, Graduate School, Kyung Hee University, Seoul 02447, Korea; [email protected] 3 Department of Biomedical Engineering, College of Medicine, Kyung Hee University, Seoul 02447, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-2-958-8980; Fax: +82-2-958-8470 Abstract: Introduction: The most frequent causes of tinnitus associated with hearing loss are noise- induced hearing loss and presbycusis. The mechanism of tinnitus is not yet clear, although several hypotheses have been suggested. Therefore, we aimed to analyze characteristics of chronic tinnitus between noise-induced hearing loss and presbycusis. Materials and Methods: This paper is a retrospective chart review and outpatient clinic-based study of 248 patients with chronic tinnitus from 2015 to 2020 with noise-induced or presbycusis. Pure tone audiometry (PTA), auditory brainstem response (ABR), distortion product otoacoustic emissions (DPOAE), transient evoked otoacoustic emissions (TEOAE), and tinnitograms were conducted. Results: PTA showed that hearing thresholds at all frequencies were higher in patients with noise-induced hearing loss than the presbycusis group. Citation: Kang, H.J.; Kang, D.W.; ABR tests showed that patients with presbycusis had longer wave I and III latencies (p < 0.05 each) Kim, S.S.; Oh, T.I.; Kim, S.H.; Yeo, S.G. -

Make Listening Safe
MAKEMake LISTENINGListening SafeSAFE ii MAKE LISTENING SAFE Concern is growing about the rising exposure to loud sounds in recreational settings such as nightclubs, discotheques, pubs, bars, cinemas, concerts, sporting events and even fitness classes. With the popularization of technology, devices such as music players are often listened to at unsafe volumes and for prolonged periods of time. Regular participation in such activities poses a serious threat of irreversible hearing loss. Cause for concern… The World Health Organization (WHO) estimates that billion young people worldwide could be at risk of hearing loss due to unsafe listening practices. Over 43 million people between the ages of 12–35 years live with disabling hearing loss due to different causes. Among teenagers and young adults aged 12–35 years in middle- and high-income countries: Nearly 50% are exposed to unsafe levels of sound from the use of personal audio devices. Around 40% are exposed to potentially damaging sound levels at clubs, discotheques and bars. Analysis of the National Health and Nutrition Examination Survey (NHANES) data from the United States suggests that between 1994 and 2006, the prevalence of hearing lossa among teenagers 12 to 19 years old rose significantly from 3.5% to 5.3%. This rise may be expected to continue as the number of people listening to music through headphones increased by 75% from 1990 to 2005 in the United States. A 2008 European Commission report states that personal audio devices are being used by an increasing proportion of the population. The increasing sales of smartphones, with 470 million devices sold globally in 2011 alone, is another indicator of potential risk.