Virulence Determinants and Antimicrobial Profiles of Pasteurella Multocida Isolated from Cattle and Humans in Egypt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Higher Education Database Whed Iau Unesco
WORLD HIGHER EDUCATION DATABASE WHED IAU UNESCO Página 1 de 438 WORLD HIGHER EDUCATION DATABASE WHED IAU UNESCO Education Worldwide // Published by UNESCO "UNION NACIONAL DE EDUCACION SUPERIOR CONTINUA ORGANIZADA" "NATIONAL UNION OF CONTINUOUS ORGANIZED HIGHER EDUCATION" IAU International Alliance of Universities // International Handbook of Universities © UNESCO UNION NACIONAL DE EDUCACION SUPERIOR CONTINUA ORGANIZADA 2017 www.unesco.vg No paragraph of this publication may be reproduced, copied or transmitted without written permission. While every care has been taken in compiling the information contained in this publication, neither the publishers nor the editor can accept any responsibility for any errors or omissions therein. Edited by the UNESCO Information Centre on Higher Education, International Alliance of Universities Division [email protected] Director: Prof. Daniel Odin (Ph.D.) Manager, Reference Publications: Jeremié Anotoine 90 Main Street, P.O. Box 3099 Road Town, Tortola // British Virgin Islands Published 2017 by UNESCO CENTRE and Companies and representatives throughout the world. Contains the names of all Universities and University level institutions, as provided to IAU (International Alliance of Universities Division [email protected] ) by National authorities and competent bodies from 196 countries around the world. The list contains over 18.000 University level institutions from 196 countries and territories. Página 2 de 438 WORLD HIGHER EDUCATION DATABASE WHED IAU UNESCO World Higher Education Database Division [email protected] -

Registered Attendees
Registered Attendees Company Name Job Title Country/Region 1996 Graduate Trainee (Aquaculturist) Zambia 1Life MI Manager South Africa 27four Executive South Africa Sales & Marketing: Microsoft 28twelve consulting Technologies United States 2degrees ETL Developer New Zealand SaaS (Software as a Service) 2U Adminstrator South Africa 4 POINT ZERO INVEST HOLDINGS PROJECT MANAGER South Africa 4GIS Chief Data Scientist South Africa Lead - Product Development - Data 4Sight Enablement, BI & Analytics South Africa 4Teck IT Software Developer Botswana 4Teck IT (PTY) LTD Information Technology Consultant Botswana 4TeckIT (pty) Ltd Director of Operations Botswana 8110195216089 System and Data South Africa Analyst Customer Value 9Mobile Management & BI Nigeria Analyst, Customer Value 9mobile Management Nigeria 9mobile Nigeria (formerly Etisalat Specialist, Product Research & Nigeria). Marketing. Nigeria Head of marketing and A and A utilities limited communications Nigeria A3 Remote Monitoring Technologies Research Intern India AAA Consult Analyst Nigeria Aaitt Holdings pvt ltd Business Administrator South Africa Aarix (Pty) Ltd Managing Director South Africa AB Microfinance Bank Business Data Analyst Nigeria ABA DBA Egypt Abc Data Analyst Vietnam ABEO International SAP Consultant Vietnam Ab-inbev Senior Data Analyst South Africa Solution Architect & CTO (Data & ABLNY Technologies AI Products) Turkey Senior Development Engineer - Big ABN AMRO Bank N.V. Data South Africa ABna Conseils Data/Analytics Lead Architect Canada ABS Senior SAP Business One -

Minufiya Veterinary Journal ISSN: 1110-9750
Minufiya Veterinary Journal ISSN: 1110-9750 Volume 9 September 2015 ISSN (prINt): 1110-9750 published by Faculty oF Veterinary medIcine University oF Sadat City egypt Email: [email protected] Minufiya Veterinary Journal ISSN: 1110-9750 Vol. 9; September 2015 ﻣﺠﻠﺲ إدارة اﻟﻤﺠﻠﺔ رﺋﯿﺲ ﻣﺠﻠﺲ إدارة اﻟﻤﺠﻠﺔ م اﻹﺳﻢ اﻟﻮظﯿﻔﺔ اﻟﺼﻔﺔ ۱ ا.د/ ﺷﻌﺒﺎن ﻣﺤﻤﺪ ﺟﺎد ﷲ ﻋﻤﯿﺪ اﻟﻜﻠﯿﺔ رﺋﯿﺲ ﻣﺠﻠﺲ اﻹدارة ھﯿﺌﺔ اﻟﺘﺤﺮﯾﺮ م اﻹﺳﻢ اﻟﻮظﯿﻔﺔ اﻟﺼﻔﺔ ۱ أ.د/ أﺣﻤﺪ ﻋﺒﺪ اﻟﻤﻨﻌﻢ زﻏﺎوة أﺳﺘﺎذ اﻷﻣﺮاض اﻟﺒﺎطﻨﺔ واﻟﻤﻌﺪﯾﺔ رﺋﯿﺲ ﺗﺤﺮﯾﺮ اﻟﻤﺠﻠﺔ ۲ أ.د/ ﺳﻌﺪ ﻋﺒﺪ اﻟﻔﺘﺎح ﻋﻤﺎره أﺳﺘﺎذ اﻟﺨﻠﯿﺔ و اﻷﻧﺴﺠﺔ ﻋﻀﻮا ً ۳ ا.د/ ﻣﺤﻤﺪ ﻋﺎطﻒ ھﻼل أﺳﺘﺎذ اﻟﺮﻋﺎﯾﺔ وﺗﻨﻤﯿﺔ اﻟﺜﺮوة اﻟﺤﯿﻮاﻧﯿﺔ ﻋﻀﻮا ً ٤ ا.د/ ﺣﻤﺎده ﺿﺎﺣﻲ ﺣﺴﯿﻦ أﺳﺘﺎذ اﻟﺮﻋﺎﯾﺔ وﺗﻨﻤﯿﺔ اﻟﺜﺮوة اﻟﺤﯿﻮاﻧﯿﺔ ﻋﻀﻮا ً ٥ أ.د/ ﺧﺎﻟﺪ ﻣﺤﻤﻮد ﻣﺤﻤﺪ ﺟﻌﻔﺮ أﺳﺘﺎذ اﻟﺘﻐﺬﯾﺔ واﻟﺘﻐﺬﯾﺔ اﻹﻛﻠﯿﻨﯿﻜﯿﺔ ﻋﻀﻮا ً ٦ د/ ﻋﻤﺎد ﻣﺤﻤﻮد ﻣﺤﻤﺪ ﻋﺒﺪ اﻟﺮازق أﺳﺘﺎذ ﻣﺴﺎﻋﺪ اﻟﺘﻮﻟﯿﺪ واﻟﺘﻨﺎﺳﻞ واﻟﺘﻠﻘﯿﺢ اﻻﺻﻄﻨﺎﻋﻲ ﻋﻀﻮا ً ۷ د. ﺷﺮﯾﻒ ﻋﺒﺪ ﷲ زﯾﺪان أﺳﺘﺎذ ﻣﺴﺎﻋﺪ ﺑﻘﺴﻢ اﻟﺼﺤﺔ واﻷﻣﺮاض اﻟﻤﺸﺘﺮﻛﺔ ﻋﻀﻮا ً ۸ د/ ﻣﺒﺮوك ﻋﻄﯿﺔ ﻋﺒﺪ اﻟﺪاﯾﻢ ﻣﺪرس اﻟﻜﯿﻤﯿﺎء اﻟﺤﯿﻮﯾﺔ وﻛﯿﻤﯿﺎء اﻟﺘﻐﺬﯾﺔ ﻋﻀﻮا ً ۹ د/ ﻣﺤﻤﺪ أﺑﻮ اﻟﻌﺰ ﻧﺎﯾﻞ ﻣﺪرس اﻷﻣﺮاض اﻟﺒﺎطﻨﺔ واﻟﻤﻌﺪﯾﺔ ﻋﻀﻮا ً ۱۰ د/ أﺣﻤﺪ ﻣﺤﻤﻮد ﻋﺒﺪ اﻟﻮاﺣﺪ اﻟﺼﯿﻔﻲ ﻣﺪرس اﻷﻣﺮاض اﻟﺒﺎطﻨﺔ واﻟﻤﻌﺪﯾﺔ ﻋﻀﻮا ً ۱۱ د/ أﻛﺮم أﺣﻤﺪ ﺣﺴﻨﯿﻦ ﺳﻼﻣﺔ ﻣﺪرس اﻷﻣﺮاض اﻟﺒﺎطﻨﺔ واﻟﻤﻌﺪﯾﺔ ﻋﻀﻮا ً ۱۲ د/ ﻣﺼﻄﻔﻰ ﻋﺒﺪ اﻟﺠﺎﺑﺮ ﻣﺪرس اﻟﺒﺎﺛﻮﻟﻮﺟﯿﺎ ﻋﻀﻮا ً ۱۳ د/ رﺑﯿﻊ اﻟﺤﺴﯿﻨﻲ اﻣﺒﺎرك ﻣﺪرس اﻟﺮﻗﺎﺑﺔ اﻟﺼﺤﯿﺔ ﻋﻠﻰ اﻷﻏﺬﯾﺔ ﻋﻀﻮا ً ۱٤ ط.ب / ﻋﺒﺎس ﻓﺘﺤﻲ ﻋﺒﺎس ﻣﺼﺮي ﻣﻌﯿﺪ اﻟﺠﺮاﺣﺔ واﻟﺘﺨﺪﯾﺮ واﻷﺷﻌﺔ ﻋﻀﻮا ً ۱٥ ط.ب/ ﻋﺒﺪ اﻟﻔﺘﺎح ﻣﺤﻤﺪ ﻋﺒﺪ اﻟﻔﺘﺎح ﻣﻌﯿﺪ اﻟﺒﺎﺛﻮﻟﻮﺟﯿﺎ اﻹﻛﻠﯿﻨﯿﻜﯿﺔ ﻋﻀﻮا ً ۱٦ أ. -

The Integration of Multivariate Statistical Approaches, Hyperspectral Reflectance, and Data-Driven Modeling for Assessing the Qu
water Article The Integration of Multivariate Statistical Approaches, Hyperspectral Reflectance, and Data-Driven Modeling for Assessing the Quality and Suitability of Groundwater for Irrigation Mosaad Khadr 1,2 , Mohamed Gad 3 , Salah El-Hendawy 4,5,*, Nasser Al-Suhaibani 4, Yaser Hassan Dewir 4,6 , Muhammad Usman Tahir 4, Muhammad Mubushar 4 and Salah Elsayed 7 1 Civil Engineering Department, College of Engineering, University of Bisha, Bisha 61922, Saudi Arabia; [email protected] 2 Irrigation and Hydraulics Department, Faculty of Engineering, Tanta University, Tanta 31734, Egypt 3 Hydrogeology, Evaluation of Natural Resources Department, Environmental Studies and Research Institute (ESRI), University of Sadat City, Minufiya 32897, Egypt; [email protected] 4 Department of Plant Production, College of Food and Agriculture Sciences, King Saud University, KSA, P.O. Box 2460, Riyadh 11451, Saudi Arabia; [email protected] (N.A.-S.); [email protected] (Y.H.D.); [email protected] (M.U.T.); [email protected] (M.M.) 5 Department of Agronomy, Faculty of Agriculture, Suez Canal University, Ismailia 41522, Egypt 6 Faculty of Agriculture, Kafrelsheikh University, Kafr El-Sheikh 33516, Egypt 7 Agricultural Engineering, Evaluation of Natural Resources Department, Environmental Studies and Research Institute, University of Sadat City, Minufiya 32897, Egypt; [email protected] * Correspondence: [email protected]; Tel.: +966-535318364 Abstract: Sustainable agriculture in arid regions necessitates that the quality of groundwater be care- Citation: Khadr, M.; Gad, M.; fully monitored; otherwise, low-quality irrigation water may cause soil degradation and negatively El-Hendawy, S.; Al-Suhaibani, N.; impact crop productivity. -

Universal Journal of Pharmaceutical Research REVIEWERS of 2020
Universal Journal of Pharmaceutical Research ISSN: 2456-8058 CODEN (USA): UJPRA3 An International Peer Reviewed Open Access Online Journal Email: [email protected] Tel: +91-9997722274 http://www.ujpr.org REVIEWERS OF 2020 We are very thankful for these experts who have evaluated and approved the articles for publication in 2020. Dr. George Zhu, Tehran University of Medical Sciences, Tehran, Iran, [email protected] Dr. Gehan Fawzy Abdel Raoof Kandeel, Pharmacognosy Department, National Research Centre, Dokki, 12622, Giza, Egypt, [email protected] Dr. Marwa A. A. Fayed, University of Sadat City, Egypt, [email protected] Asmaa Ahmed Mohamed Ahmed Khalifa, Pharos University, Alexandria, Egypt, [email protected] Dr. Sabah Hussien El-Ghaiesh, Tanta University, Egypt, [email protected] Dr. Mujde Eryilmaz, Ankara University, Turkey, [email protected] Rola Jadallah, Arab American University, Palestine, [email protected] Aya Mohammed Mohammed Essawy, MTI University- Mokattam, Egypt, [email protected] Dr. Nada Farrag, Misr International University Egypt, [email protected] Dr. Hayriye Eda Şatana Kara, Gazi University, Turkey, [email protected] Dr. Mohamed Ismail Nounou, Appalachian College of Pharmacy, Oakwood, Virginia, USA, [email protected] Dr. Dalia Kamal Zaffar Ali, Modern University for technology and information, Egypt, [email protected] Dr. Mohammad Tauseef, Department of Pharmaceutical Sciences College of Pharmacy, Chicago State University, [email protected] Prof. Dr. Ali Gamal Ahmed Al-kaf, Sana'a university, Yemen, [email protected] Dr. Mahmut Yıldıztekin, Muğla Sıtkı Koçman University, Turkey, [email protected] Kian Navaee, Shahre Daru Pharmaceutical Co., Iran, [email protected] Dr. Mohammad Shaheen Khan, University Malaysia Sabah, Malaysia, [email protected] Hebatallaha A Moustafa, Ain Shams University, Egypt, [email protected] Dr. -

Prof. Dr. Mahsoub Abdul Qadir Al Dawi
Curriculum Vitae Identification: Name: Mahsoub Abdel Qader Al Dhowey Hasan Birth Date and Place: May 15, 1972, Qena, Egypt. Faculty / Department: Faculty of Education / Educational Psychology dept. Position: Professor (2016) Address: - South Valley University, Faculty of Education, Qena, Egypt - Mobile: 01153622565 - E-mail: [email protected], [email protected], [email protected] Education: Ph.D., Educational Psychology (Educational & Psychological Statistics Major), South Valley University, Qena, Egypt (2004). M. A., Educational Psychology (Psychological Measurement Major), South Valley University, Qena, Egypt (2001). Special Diploma in Education, Qena Faculty of Education, South Valley University (1998). Bachelor of Science and Education, Mathematics Major, Assiut University (Qena Branch) (1994). Professional Experience: Professor of Educational Psychology: Qena Faculty of Education, South Valley University (2016). Assistant Professor of Educational Psychology: Qena Faculty of Education, South Valley University (2011). Accreditation Specialist: Education Reform Program (ERP), Academy for Educational Development, Head quarters, Cairo, Egypt, (2007-2009) with the following Responsibilities: 1. Initiate and maintain relations with Faculties of Specific Education, Faculties of Kindergarten and Faculty of Art Education Helwan University. 2. Conduct appropriate studies to analyze current situations and provide background documents for future planning. 3. Develop and implement annual work plans for introducing systems and policy changes in the area of education. 4. Prepare annual budgets and oversee expenditure. 5. Develop training packages on strategic planning and assessing academic programs in higher education. 6. Heading 4-day workshop on strategic planning. 7. Heading 3-day workshop on gap analysis for the academic programs. Professional and Organizational Development Advisor (POD): Education Reform Program, Academy for Educational Development, Egypt, Qena Office, (2006- 2007) with the following Responsibilities: 1. -

Curriculum Vitae Prof
Curriculum Vitae Prof. Dr. MOHAMED ATEF YOUSSEF HELAL Name: MOHAMED ATEF YOUSSEF HELAL Place of birth: Motobis, Kafr El-Sheikh, Egypt Date of birth: November 29, 1967 Nationality: Egyptian Marital status: Married and I have 4 children Current Address: Kafrelsheikh University Faculty of Veterinary Medicine, Department of Animal Wealth Development, Egypt. Work Phone: +20473231311 Work Fax: +20473231311 Home phone: +20472696670 Mobile phone: +201094342621 E-mail: [email protected], [email protected] Academic Education: B.V.Sc. Faculty of Veterinary Medicine- 1990 Alexandria University - Egypt Master of Animal breeding Faculty of Veterinary Medicine- 1994 and production Alexandria University - Egypt PhD of Animal breeding and Faculty of Veterinary Medicine- 1999 production Alexandria University - Egypt Current Job: Vice Dean for Post-graduate Studies Affairs Head of Department of Animal Wealth Development, Faculty of Veterinary Medicine, Kafrelsheikh University Terms of reference: Teaching of Animal, Poultry and Fish Breeding and Production courses to the under- and post-graduate veterinary students. Teaching of Veterinary Biostatistics Courses to the under- and post-graduate veterinary students. Supervision of the post graduate students in the faculty. Trainer for under-graduate students (2nd) in summer training. External examiner for under-graduate students in other faculties of veterinary medicine in Egypt. Previous Jobs: 1) Demonstrator of Animal and Poultry production, Faculty of Veterinary Medicine, Alexandria University -
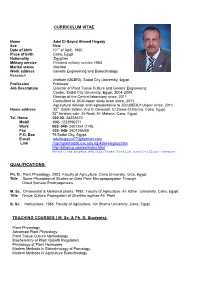
Adelhegazycv
CURRICULUM VITAE Name Adel El-Sayed Ahmed Hegazy Sex Male Date of birth 10 th of April, 1960 Place of birth Cairo, Egypt Nationality Egyptian Military service Finished military service 1983 Marital status Married Work address Genetic Engineering and Biotechnology Research Institute (GEBRI), Sadat City University, Egypt. Profession Professor Job Description Director of Plant Tissue Culture and Genetic Engineering Center, Sadat City University, Egypt, 2004-2009. Director of the Central laboratory since, 2011. Consultant to JICA/Japan study team since, 2011. Agriculture Advisor and representative to JDI/JBEDC1/Japan since, 2011. Home address 25st Salah Salem. Ard El.Genenah, El.Zawia El.Hamra, Cairo, Egypt. 25st Ibrahim sakr. El-Akad, El- Mataria, Cairo, Egypt. Tel. Home 002-02- 24226670. Mobil 002- 1223996271. Work 002- 048- 2601264 (140). Fax 002- 048- 2601266/68 P.O. Box 79 Sadat City, Egypt. E-mail [email protected] Link http://gebrisadat.usc.edu.eg/Adel-Hegazy.htm http://jditokyo.com/en/index.html https://ag.purdue.edu/hla/Pages/Profile.aspx?strAlias=ahegazy QUALIFICATIONS: Ph. D. Plant Physiology, 2003. Faculty of Agriculture, Cairo University, Giza, Egypt. Title Some Physiological Studies on Date Palm Micropropagation Through Direct Somatic Embryogenesis. M. Sc. Ornamental & Medicinal plants, 1992. Faculty of Agriculture, Al- Azhar University, Cairo, Egypt. Title Tissue Culture Propagation of Strelitzia reginae Ait. Plant B. Sc. Horticulture, 1986. Faculty of Agriculture, Ain Shams University, Cairo, Egypt. TEACHING COURSES ( M. Sc. & Ph. D. Students): Plant Physiology. Advanced Plant Physiology. Plant Tissue Culture Methodology. Biochemistry of Plant Growth Regulators. Physiology of Plant Hormones. Modern Methods in Biotechnology of Pomology. -
Published Research Articles in International Journals Suez Canal University (Abstracts)
Published Research Articles in International Journals 2018-2019 Suez Canal University Post-Graduate Studies &Research Sector Published Research Articles in International Journals Suez Canal University (Abstracts) 2018, 2019 Pag 1 Published Research Articles in International Journals 2018-2019 جامعة قناة السويس قطاع الدراسات العليا والبحوث ملخص اﻻبحـاث العلميـــة المنشــورة بالدوريات العلمية العالمــية جامعة قناة السويس 1029-1028 Pag 2 Published Research Articles in International Journals 2018-2019 كلمة السيد اﻻستاذ الدكتور/ رئيس جامعة قناة السويس يعد البحث العلمى أداة اﻷمم للتقدم وصناعة الحضارة واﻻرتقاء بالشعوب وتحقيق رفاهيتها ، ويعد ما تمتلكه أى أمة من أبحاث علمية متقدمة وما تمتلكه من تراث علمى دقيق أحد المعايير المهمة للحكم على تقدم اﻷمة ، ولذا يشهد العالم سباقا وتعاونا فى هذا المجال حتى يستطيع اﻻنسان تسخير قوى الطبيعة وثرواتها لراحته وسعادته . كما يعد البحث العلمى الدعامة اﻻساسية لﻻقتصاد والتطور وقناة مهمة ﻻثراء المعرفة اﻻنسانية فى ميادينها كافة ، لذا فإن ما تمتلكه اﻷمة من علماء يعتبر ثروة تفوق كل الثروات الطبيعية . ولذلك تحرص جامعة قناة السويس على تشجيع النشر الدولى الذى سيضع الجامعة فى موقع ﻷئق ضمن التصنيف العالمى للجامعات ، والذى يعتمد من بين معاييره على عدد اﻻبحاث العلمية المنشورة بالدوريات العلمية العالمية ، وتنتهج الجامعة طريقا لتنمية اﻻبداع والتفكير العلمى لدى الشباب حتى يمكن تحقيق التقدم وبناء مستقبل مشرق . وفقنا هللا لما فيه الخير لمصرنا الحبيبة أ.د/ أحمد زكي حسين متولي رئيس جامعة قناة السويس Pag 3 Published Research Articles in International Journals 2018-2019 أصبح البحث العلمى واحد من المجاﻻت الهامة التى تجعل الدول تتطور بسرعة هائلة وتتغلب على المشكﻻت التى تواجهها بطرق علمية حيث ان البحث العلمى فى حياة اﻻنسان ينبع من مصدرين هامين وهما : المصدر اﻻول:- يتمثل فى اﻻنتفاع بفوائد تطبيقية حيث تقوم الجهات المسئولة بتطبيق هذه الفوائد التى نجمت عن اﻻبحاث. -

Assessment of Soil Pollution Levels in North Nile Delta, by Integrating Contamination Indices, GIS, and Multivariate Modeling
sustainability Article Assessment of Soil Pollution Levels in North Nile Delta, by Integrating Contamination Indices, GIS, and Multivariate Modeling Mohamed E. Abowaly 1, Abdel-Aziz A. Belal 2 , Enas E. Abd Elkhalek 1, Salah Elsayed 3, Rasha M. Abou Samra 4, Abdullah S. Alshammari 5, Farahat S. Moghanm 1 , Kamal H. Shaltout 6, Saad A. M. Alamri 7 and Ebrahem M. Eid 7,8,* 1 Soil and Water Department, Faculty of Agriculture, Kafrelsheikh University, Kafr El-Sheikh 33516, Egypt; [email protected] (M.E.A.); [email protected] (E.E.A.E.); [email protected] (F.S.M.) 2 Agricultural Applications, Soil and Marine Science Division, National Authority for Remote Sensing and Space Sciences, Alf Maskan, Cairo 1564, Egypt; [email protected] 3 Agricultural Engineering, Evaluation of Natural Resources Department, Environmental Studies and Research Institute, University of Sadat City, Minufiya 32897, Egypt; [email protected] 4 Environmental Sciences Department, Faculty of Science, Damietta University, New Damietta 34517, Egypt; [email protected] 5 Biology Department, College of Science, Ha’il University, Ha’il 55476, Saudi Arabia; [email protected] 6 Botany Department, Faculty of Science, Tanta University, Tanta 31527, Egypt; [email protected] 7 Biology Department, College of Science, King Khalid University, Abha 61321, Saudi Arabia; Citation: Abowaly, M.E.; Belal, [email protected] A.-A.A.; Abd Elkhalek, E.E.; Elsayed, 8 Botany Department, Faculty of Science, Kafrelsheikh University, Kafr El-Sheikh 33516, Egypt S.; Abou Samra, R.M.; Alshammari, * Correspondence: [email protected] or [email protected]; Tel.: +966-552-717-026 A.S.; Moghanm, F.S.; Shaltout, K.H.; Alamri, S.A.M.; Eid, E.M. -

Perspectives and Policies for Innovation in Egypt
UNIVERSITY OF THESSALY DEPARTMENT OF PLANNING AND REGIONAL DEVELOPMENT EUROPEAN REGIONAL DEVELOPMENT STUDIES POSTGRADUATE PROGRAM STUDENT EVANGELIA KYRIAZOPOULOU SUPERVISOR PANTOLEON SKAYANNIS PERSPECTIVES AND POLICIES FOR INNOVATION IN EGYPT VOLOS, JANUARY 2015 Institutional Repository - Library & Information Centre - University of Thessaly 04/10/2021 00:43:04 EEST - 170.106.38.176 To Dimitrios Anagnostopoulos i Institutional Repository - Library & Information Centre - University of Thessaly 04/10/2021 00:43:04 EEST - 170.106.38.176 Acknowledgments I would like to express much gratitude to Professor Pantoleon Skayannis who gave me the opportunity to deal with this issue and assumed the role of supervisor. I am indebted for all his advice and guidance in the making of this dissertation. Furthermore I would like to thank my husband and my parents for their patience and practical support throughout my effort. Special thanks also to my three years old daughter, who gave me force with her presence with the promise that whatever I got from my experience, I will try to transmit to her, bringing her the positive image of learning and science. ii Institutional Repository - Library & Information Centre - University of Thessaly 04/10/2021 00:43:04 EEST - 170.106.38.176 ABBREVIATIONS ARTI Agenzia Regionale per la tecnologia e l’innovazione ASRT Academy of Scientific Research and Technology CIA Central Intelligence Agency DFG German Finance Association EIMP Environmental Information and Monitoring Program ESCWA Economic and Social Commission for -

Bioorganic Chemistry 82 (2019) Ii-Xiv
Bioorganic Chemistry 82 (2019) ii-xiv Contents lists available at ScienceDirect Bioorganic Chemistry journal homepage: www.elsevier.com/locate/bioorg Graphical Abstracts/Bioorganic Chemistry 82 (2019) ii-xiv Unusual cadinane-type sesquiterpene glycosides with α-glucosidase inhibitory activities Bioorganic Chemistry 82 (2018) pp. 1–5 from the fruit of Cornus officinalis Sieb. et Zuuc. Jun Hea,1, Jie-kun Xub,1, Xue-ge Pana,b, Xian-sheng Yea,b, Pin-yi Gaoc,YuYana, Chun-yang Xud, ⁎ Gui-fen Qiangd, Guan-hua Dud, Yung-Chi Chenge, Wei-ku Zhanga, aDepartment of Pharmacy & Institute of Clinical Medical Sciences, China-Japan Friendship Hospital, Beijing 100029, People’s Republic of China bSchool of Life Sciences, Beijing University of Chinese Medicine, Beijing 100029, People’s Republic of China cCollege of Pharmaceutical and Biotechnology Engineering, Institute of Functional Molecules, Shenyang University of Chemical Technology, Shenyang 110142, People's Republic of China dState Key Laboratory of Bioactive Substances and Functions of Natural Medicines, Institute of Materia Medica, Chinese Academy of Medical Sciences and Peking Union Medical College and Beijing Key Laboratory of Drug Target and Screening Research, Beijing 100050, People's Republic of China eDepartment of Pharmacology, School of Medicine, Yale University, New Haven, CT 06520, USA Acridine-based (thio)semicarbazones and hydrazones: Synthesis, in vitro urease inhibition, Bioorganic Chemistry 82 (2018) pp. 6–16 molecular docking and in-silico ADME evaluation Ibanga Okon Isaaca, Mariya