Balancing Safety and Efficacy in Pediatric Asthma Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparison of Intramuscular Betamethasone and Oral
Color profile: Disabled Composite Default screen 100 ORIGINAL ARTICLE 100 95 95 75 75 25 25 5 5 0 Comparison of intramuscular 0 betamethasone and oral prednisone in the prevention of relapse of acute asthma John S Chan MD1, Robert L Cowie MD1, Gerald C Lazarenko MD2, Cinde Little RRT1, Sandra Scott RRT1, Gordon T Ford MD FCCP1 1Division of Respiratory Medicine and 2Department of Emergency Medicine, University of Calgary, Calgary, Alberta JS Chan, RL Cowie, GC Lazarenko, C Little, S Scott, tively) and use of inhaled corticosteroids (46% versus 64.3% GT Ford. Comparison of intramuscular betamethasone respectively) (P<0.05). Using intention-to-treat analysis, the and oral prednisone in the prevention of relapse of acute relapse rates for betamethasone and prednisone at day 7 were asthma. Can Respir J 2001;8(3):147-152. 14.9% (13 of 87 patients) and 25% (21 of 84 patients), respectively (P=0.1), and at day 21, the rates were 36.8% (32 OBJECTIVE: To compare the relapse rate after a single intra- of 87 patients) and 31% (26 of 84 patients), respectively muscular injection of a long acting corticosteroid, betametha- (P=0.4). There were no differences in symptom score, peak sone, with oral prednisone in patients discharged from the flows and adverse effects between the two groups at days 7 emergency department (ED) for acute exacerbations of and 21. asthma. CONCLUSIONS: A single dose of intramuscular betametha- PATIENTS AND METHODS: Patients with acute exacer- sone 12 mg was safe and as efficacious as prednisone in pre- bations of asthma who were suitable for discharge from the venting the relapse of acute asthma. -

Long-Term Budesonide Or Nedocromil Mineral Accretion Over a Period of Years
term inhaled corticosteroid (ICS) treatment on bone Long-term Budesonide or Nedocromil mineral accretion over a period of years. Treatment, Once Discontinued, Does Not Alter the Course of Mild to Moderate Asthma in STUDY POPULATION. Cohort follow-up study for a median Children and Adolescents of 7 years with 877 children 5 to 12 years of age who Strunk RC, Sternberg AL, Szefler SJ, et al. J Pediatr. had mild-to-moderate asthma and initially were ran- 2009;154(5):682–687 domly assigned in the Childhood Asthma Management Program. PURPOSE OF THE STUDY. To determine whether long-term, METHODS. Serial dual-energy x-ray absorptiometry scans continuous use of inhaled antiinflammatory medications of the lumbar spine to assess bone mineral density were affects asthma outcomes in children with mild-to-mod- performed for all patients. Annual bone mineral accre- erate asthma after use is discontinued. tion was calculated for 531 boys and 346 girls. STUDY POPULATION. A total of 941 children, 5 to 12 years of RESULTS. Oral corticosteroid bursts produced dose- age, who had previously participated in the Childhood dependent reductions in bone mineral accretion (0.052, Asthma Management Program (CAMP). 0.049, and 0.046 g/cm2 per year with 0, 1–4, and Ն5 courses, respectively) and increases in the risk for osteo- METHODS. During the CAMP trial, subjects received treat- penia (10%, 14%, and 21%, respectively) in boys but ment with budesonide, nedocromil, or placebo for 4.3 not girls. Cumulative ICS use was associated with a small years. During the posttrial period, asthma manage- decrease in bone mineral accretion in boys but not girls ment was provided by primary care physicians ac- but no increased risk for osteopenia. -

FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting
FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting August 31, 2020 sNDA 209482: fluticasone furoate/umeclidinium/vilanterol fixed dose combination to reduce all-cause mortality in patients with chronic obstructive pulmonary disease NDA209482/S-0008 PADAC Clinical and Statistical Briefing Document Fluticasone furoate/umeclidinium/vilanterol fixed dose combination for all-cause mortality DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the supplemental New Drug Application (sNDA) 209482, for fluticasone furoate/umeclidinium/vilanterol, as an inhaled fixed dose combination, for the reduction in all-cause mortality in patients with COPD, to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered -

Protective Effects of Inhaled Ipratropium Bromide on Bronchoconstriction Induced by Adenosine and Methacholine in Asthma
Eur Aesplr J 1992, 5, 56()-665 Protective effects of inhaled ipratropium bromide on bronchoconstriction induced by adenosine and methacholine In asthma N. Crimi, F. Palermo, R. Oliveri, R. Polosa, I. Settinieri, A. Mistretta Protective effects of inhaled ipratropium bromide on bronchoconstriction induced by Istituto di Malattie dell' Apparato adenosine and methacholine in asthma. N. Crimi, F. Palermo, R. Oliveri, R. Po/osa, Respiratorio e Tisiologia, Universita' di Catania, Catania, Italy. I. Seuinier~ A. Mistretta. ABSTRACT: Although adenosine-Induced bronchoconstrictlon is mainly due to Correspondence: N. Crimi mast cell mediator release, vagal reflexes have also been Implicated in this Istituto di Malattie dell' Appara.to response. Respiratorio e Tisiologia We have Investigated the effect of a speciflc muscarlnlc-receptor antagonist, Universita' di Catania ipratroplum bromide, on methacholine- and adenosine-Induced bronchoconstriction Via Passo Gravina 187 In a randomized, placebo-controlled, double-blind study of 12 asthmatic subjects. 95125 Catania Airway response was evaluated as forced expiratory volume in one second (FEV,). Italy Inhaled lpratroplum bromide (40 Jlg), administered 20 mln prior to bronchoprovocation, Increased the provocation dose of Inhaled methacholine and Keywords: Adenosine adenosine required to reduce FEV, by 20% from baseline (PD,.) from 0.11 to 0.79 asthma ipratropium bromide mg (p<O.Ol) and from 0.57 to 1.27 mg (p<0.01), respectively. The mean baseline methacholine FEV, values after administration of lpratroplum bromide were signlfkantly higher than after placebo administration (p<O.OS). However, there was no correlation Received: May 22 1991 between the degree of bronchodllatatlon and dose-ratios for methacholine and Accepted after revision January 7 1992 adenosine. -

Core Safety Profile
Core Safety Profile Active substance: Nedocromil Pharmaceutical form(s)/strength: Eye drops: 20 mg/ml, Inhalation vapour: 5 mg/ml, Pressurised inhalation: 2 mg/dose, 2mg/0,1 mg, Nebuliser solution: 10 mg/2 ml, Inhalation powder: 10 mg/dose, Nasal spray: 10 mg/ml P-RMS: CZ/H/PSUR/0016/001 Date of FAR: 09.10.2010 EU Core Safety Profile (CSP) For Nedocromil sodium NB: This CSP is combining safety information from the three existing pharmaceutical forms: Eye drops, Nasal spray and Inhaler. Information that is specific to one form is identified by a subheading. No subheading indicates that information is valid for all pharmaceuticals forms 4.3 Contraindications For eye drops <Product name> eye drops is contraindicated in patients with known hypersensitivity to nedocromil sodium, benzalkonium chloride or other constituents of the formulation. For Nasal spray and Inhaler <Product name> nasal spray or inhaler is contraindicated in patients with known hypersensitivity to any of the constituents. 4.4 Special warnings and precautions for use For eye drops Patients should be advised not to wear soft contact lenses during treatment with <product name> eye drops. Benzalkonium chloride, a constituent of the formulation, may accumulate in soft contact lenses. This preservative, when slowly released, could possibly irritate the cornea. In patients who continue to wear hard or gas permeable contact lenses during <product name> eye drops treatment, the lenses should be taken out of the eye prior to instillation of the drops. They should be inserted again not earlier than 10 minutes after administration, in order to allow an even conjunctival distribution of the solution. -

Drug Class Review Nasal Corticosteroids
Drug Class Review Nasal Corticosteroids Final Report Update 1 June 2008 The Agency for Healthcare Research and Quality has not yet seen or approved this report The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Dana Selover, MD Tracy Dana, MLS Colleen Smith, PharmD Kim Peterson, MS Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Marian McDonagh, PharmD, Principal Investigator, Drug Effectiveness Review Project Copyright © 2008 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 1 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION ..........................................................................................................................5 Scope and Key Questions .......................................................................................................................7 METHODS ....................................................................................................................................9 Literature Search .....................................................................................................................................9 -
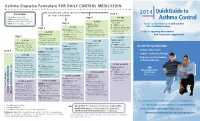
Asthma Control
Asthma Stepwise Formulary FOR DAILY CONTROL MEDICATION QuickGuide to abbreviations: step 6 2014 • ICS: inhaled corticosteroid step 5 • LABA: long-acting beta2-agonist Asthma Control HIGH-DOSE ICS • LTRA: leukotriene receptor antagonist (per step 5) • SABA: short-acting beta2-agonist step 4 LTRA (per step 4) for the care of pediatric and adult patients + LTRA (per step 4) + HIGH-DOSE ICS with established asthma step 3 (mark choice): + oral systemic steroids MEDIUM-DOSE ICS fluticasone (Flovent) MDI: (lowest dose for the shortest (per step 3; mark a choice there) 110 mcg: 2 puffs twice daily duration: 5-10 mg is A tool for ongoing assessment considered low-dose) MEDIUM-DOSE ICS + LTRA: montelukast budesonide (Pulmicort) respules: and treatment adjustment step 2 (mark choice): (Singulair) by mouth: 1.0 mg: 1 respule twice daily 4 mg: 1 tablet once daily, or fluticasone (Flovent) MDI: 1 packet oral granules once daily 110 mcg: 1 puff twice daily HIGH-DOSE ICS budesonide (Pulmicort) respules: (per step 5) LOW-DOSE ICS (mark choice): LABA (per step 3) 0.50 mg: 1 respule twice daily + LABA (per step 4) fluticasone (Flovent) MDI: + HIGH-DOSE ICS LABA (per step 3) Inside the QuickGuide... 44 mcg: 2 puffs twice daily (mark choice): + oral systemic steroids budesonide (Pulmicort) respules: + MEDIUM-DOSE ICS fluticasone (Flovent) MDI: (lowest dose for the shortest 0.25 mg: 1 respule twice daily (mark choice): • Asthma control tables step 1 110 mcg: 2 puffs twice daily duration: 5-10 mg is considered low-dose) fluticasone (Flovent) -

Product Information Tilade Cfc-Free
PRODUCT INFORMATION TILADE CFC-FREE NAME OF THE MEDICINE nedocromil sodium DESCRIPTION Tilade CFC-Free contains nedocromil sodium as a suspension in a non-CFC propellant, 1,1,1,2,3,3,3-heptafluoropropane (HFA-227). Other excipients include povidone, macrogol 600 and menthol. CAS number: 69049-74-74 Nedocromil sodium (Disodium 9-ethyl-6,9-dihydro-4,6-dioxo-10-propyl-4H-pyrano-(3,2- g)quinoline-2,8-dicarboxylate). PHARMACOLOGY Nedocromil sodium inhibits the release of inflammatory mediators from a variety of cell types occurring in the lumen and in the mucosa of the bronchial tree. Laboratory experiments have shown that nedocromil sodium prevents the release of inflammatory chemotactic and smooth muscle contracting mediators which are preformed or derived from arachidonic acid metabolism by both the lipoxygenase and cyclo-oxygenase pathways in a range of human and animal leucocytes. In the Ascaris suum sensitised monkey subjected to bronchial challenge with specific antigen, nedocromil sodium provides protection against changes in airways resistance and lung compliance. Nedocromil sodium prevents the release of mediators such as histamine, LTC4 and PGD2 from the cellular population of the chronically inflamed bronchus. There is growing evidence that these mediators are important also in lung disease in man, and this additional activity may be expected to give nedocromil sodium extended scope in the management of bronchial asthma in which inflammation, allergy and bronchial hyper-responsiveness are significant physiological factors. Pharmacokinetics After inhalation, nedocromil sodium is deposited throughout the respiratory tract, from which about 5% of the dose is absorbed. By the nature of inhalation dosing, much of the delivered dose is swallowed directly or subsequently upon mucociliary clearance from the large airways. -
![Supplement to NDL [As of December, 17,2008]](https://docslib.b-cdn.net/cover/4691/supplement-to-ndl-as-of-december-17-2008-1564691.webp)
Supplement to NDL [As of December, 17,2008]
Supplement to NDL [As of December, 17,2008] S/N GENERIC NAME DESCRIPTION TGROUP 1 Abacavir sulfate Tablet, 60mg Anti-infective,Anti- retroviral 2 Abacavir sulfate+Lamivudine Tablet, 60mg+30mg Anti-infective,Anti- retroviral 3 Abacavir Tablet, 60mg+30mg+60mg Anti-infective,Anti- sulfate+Lamivudine+Zidovudine retroviral 4 Acarbose Tablet, 50mg, 100mg Oral Anti-diabetic 5 Acemetacin Capsule, 30mg, 60mg, 90mg(D/R) Anti-rheumatic 6 Alfacalcidol Capsule(s/g), 1mcg Vitamins 7 Amikacin Eye drop, 0.3% Ophthalmic, Antibacterial 8 Apraclonidine Eye drop, 0.5%, 1% Ophthalmic, Anti-glaucoma 9 Azelastin Eye drop, 0.05% Ophthalmic, Anti-allergic 10 Betamethasone sodium Injection, 2mg+5mg/2ml Anti-inflammatory phosphate+Betamethasone dipro 11 Bimatoprost Eye drop, 0.003% Ophthalmic, Anti-glaucoma 12 Brimonidine Eye drop, 0.2% Ophthalmic, Anti-glaucoma 13 Bromfenac Eye drop, 0.1% Ophthalmic, Anti- inflammatory 14 Cefditoren Tablet 200mg, 400mg Anti-infective 15 Chloramphenicol+Dexamethasone Eye drop, 0.5%+0.1% Ophthalmic, Anti- infective/Anti-inflammatory combination 16 Ciprofloxacin Eye drop(ointment), 0.3% Ophthalmic, Antibacterial 17 Cisatracurium Injection, 2mg Neuromuscular blocker 18 Clotrimazole Troches, 10mg Orophargeal preparation 19 Cyproterone acetate Tablet, 50mg Anti-androgenic hormone 20 Darunavir Tablet(f/c), 300mg Anti-infective, Anti- retroviral 21 Desloratadine Tablet, 5mg, Syrup, 0.5mg/ml Anti-histamine 22 Dexamethasone acetate +Clotrimazole Cream, 0.4mg+100mg Dermatological, Anti- inflammatory/Anti-infective combination 23 Drospirenone+Ethinyl -
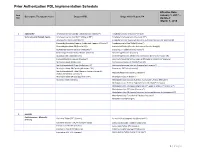
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Effective Date: Item January 1, 2017 – Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA Nbr Updated: March 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet ( Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine Suspension (Dyanavel XR®) Atomoxetine Capsule (Strattera®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine Sulfate Tablet (Evekeo®) Dexmethylphenidate ER (Focalin XR®) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Dextroamphetamine Solution (Procentra®) Clonidine ER Tablet (Generic; Kapvay®) Dextroamphetamine Sulfate Tablet (Generic) Dexmethylphenidate (Focalin®) Guanfacine ER Tablet (Generic) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Lisdexamfetamine Capsule (Vyvanse®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate IR (Generic) Dextroamphetamine IR Tablet (Zenzedi®) Methylphenidate ER Chew (Quillichew ER®) Dextroamphetamine Solution (Generic for Procentra®) Methylphenidate ER Capsule (Metadate CD®) Guanfacine ER Tablet (Intuniv®) Methylphenidate ER Tablet (Generic; Generic Concerta®; Methamphetamine (Generic; Desoxyn®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Methylphenidate IR (Ritalin®) Modafinil Tablet (Generic) Methylphenidate Solution (Generic; Authorized Generic; Methylin®) Methylphenidate -

COPD/Asthma Class Update
Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35, Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 © Copyright 2012 Oregon State University. All Rights Reserved Class Update: Asthma/COPD Medications Month/Year of Review: July 2014 Last Oregon Review: May 2012/November 2013 PDL Classes: Asthma Controller, Asthma Rescue, COPD Source Documents: OSU College of Pharmacy New drug(s): Anoro® Ellipta® (umeclidinium/vilanterol) Manufacturer: GSK/Theravance Dossier Received: Yes Current Status of PDL Classes: Chronic Obstructive Pulmonary Disease (COPD): Preferred Agents: IPRATROPIUM BROMIDE HFA AER AD, IPRATROPIUM BROMIDE SOLUTION, IPRATROPIUM/ALBUTEROL SULFATE AMPUL-NEB, TIOTROPIUM BROMIDE(SPIRIVA®) CAP W/DEV, IPRATROPIUM/ALBUTEROL (COMBIVENT®) RESPIMAT Non-Preferred Agents: AFORMOTEROL (BROVANA®), FORMOTEROL (PERFOROMIST), ROFLUMILAST (DALIRESP®), INDACATEROL (ARCAPTA®) NEOHALER, ACLIDINIUM (TUDORZA®) PRESSAIR, VILANTEROL/FLUTICASONE (BREO®) ELLIPTA Asthma Controllers and Asthma Rescue Preferred Agents: BECLOMETHASONE DIPROPIONATE(QVAR®), BUDESONIDE (PULMICORT FLEXHALER®), BUDESONIDE / FORMOTEROL FUMARATE (SYMBICORT®), FLUTICASONE PROPIONATE(FLOVENT HFA®), FLUTICASONE PROPIONATE(FLOVENT DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR DISKUS®), FLUTICASONE/SALMETEROL(ADVAIR HFA®), FORMOTEROL (FORADIL®) AEROLIZER, MONTELUKAST SODIUM TAB CHEW/TABLET, SALMETEROL XINAFOATE (SEREVENT®), ALBUTEROL SULFATE SOLUTION/VIAL NEBS, PIRBUTEROL ACETATE, PROAIR® HFA, VENTOLIN® HFA Non-preferred Agents: CICLESONIDE -

Mast Cell Stabilisers
Technological University Dublin ARROW@TU Dublin School of Food Science and Environmental Articles Health 2020 Mast Cell Stabilisers Tao Zhang Technological University Dublin, [email protected] Deirdre Frances Finn Trinity College Dublin, Ireland James William Barlow Royal College of Surgeons in Ireland See next page for additional authors Follow this and additional works at: https://arrow.tudublin.ie/schfsehart Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons Recommended Citation Zhang, T., Finn, D.F., Barlow, J.W. and Walsh, J.J. (2016). Mast cell stabilisers. European Journal of Pharmacology, 778, 158-168. This Review is brought to you for free and open access by the School of Food Science and Environmental Health at ARROW@TU Dublin. It has been accepted for inclusion in Articles by an authorized administrator of ARROW@TU Dublin. For more information, please contact [email protected], [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-Share Alike 4.0 License Authors Tao Zhang, Deirdre Frances Finn, James William Barlow, and John Jarlath Walsh This review is available at ARROW@TU Dublin: https://arrow.tudublin.ie/schfsehart/363 Mast Cell Stabilisers Tao Zhang, Deirdre Frances Finn, James William Barlow and John Jarlath Walsh*. School of Pharmacy and Pharmaceutical Sciences, Trinity College Dublin, Dublin 2, Ireland *Address for correspondence: Dr. John J. Walsh, School of Pharmacy and Pharmaceutical Sciences, Trinity College Dublin, Dublin 2, Ireland. Ph: +353-1-8962806; Fax: +353-1- 8962804; email: [email protected]. 1 Abstract Mast cells play a critical role in type 1 hypersensitivity reactions.