Protective Effects of Inhaled Ipratropium Bromide on Bronchoconstriction Induced by Adenosine and Methacholine in Asthma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Protective Effects of Tiotropium Bromide in Patients with Airways Hyperres P O N S I V E N E S S
European Review for Medical and Pharmacological Sciences 2004; 8: 259-264 Early protective effects of tiotropium bromide in patients with airways hyperres p o n s i v e n e s s C. TERZANO, A. PETROIANNI, A. RICCI, L. D’ANTONI, L. ALLEGRA* Department of Cardiovascular and Respiratory Sciences, Respiratory Diseases Unit, Fondazione E. Lorillard Spencer Cenci, “La Sapienza” University - Rome (Italy) *Institute of Respiratory Diseases, University of Milan, Ospedale Maggiore IRCCS – Milan (Italy) Abstract. – Tiotropium is an anticholiner- Introduction gic drug for Ch ronic Obstructive Pulmonary Di sease (COPD) patients, with a peak b ron- Ti o t rop ium is a qu atern a ry amm o niu m chodilator effect observed after 1.5 to 2 hours and a long duration of action. The aim of our co ngener of atropine. It has been developed study was to quantify the early protection of a as a lon g-acting an ticho linergic bro n c h o d i l a- single dose of inhaled tiotropium against metha- tor for inhalation by patients with chronic ob- choline-induced bronchoconstriction in asthmat- s t ructive pu lmon ary d isease (COPD). Dru g ic patients with airway hyperresponsiveness. p ro p e rties o f ant icho lin ergic agent s have Ten subjects (7M, 3F), with history of asthma been well-kno wn to man y cultures for many and a baseline FEV (Forced Expiratory Volume 1 1 1 c e n t u r i e s . In the 1920s the d iscovery o f the sec) >80% of pred icted, were enrolled in the s t u d y. -

Comparison of Intramuscular Betamethasone and Oral
Color profile: Disabled Composite Default screen 100 ORIGINAL ARTICLE 100 95 95 75 75 25 25 5 5 0 Comparison of intramuscular 0 betamethasone and oral prednisone in the prevention of relapse of acute asthma John S Chan MD1, Robert L Cowie MD1, Gerald C Lazarenko MD2, Cinde Little RRT1, Sandra Scott RRT1, Gordon T Ford MD FCCP1 1Division of Respiratory Medicine and 2Department of Emergency Medicine, University of Calgary, Calgary, Alberta JS Chan, RL Cowie, GC Lazarenko, C Little, S Scott, tively) and use of inhaled corticosteroids (46% versus 64.3% GT Ford. Comparison of intramuscular betamethasone respectively) (P<0.05). Using intention-to-treat analysis, the and oral prednisone in the prevention of relapse of acute relapse rates for betamethasone and prednisone at day 7 were asthma. Can Respir J 2001;8(3):147-152. 14.9% (13 of 87 patients) and 25% (21 of 84 patients), respectively (P=0.1), and at day 21, the rates were 36.8% (32 OBJECTIVE: To compare the relapse rate after a single intra- of 87 patients) and 31% (26 of 84 patients), respectively muscular injection of a long acting corticosteroid, betametha- (P=0.4). There were no differences in symptom score, peak sone, with oral prednisone in patients discharged from the flows and adverse effects between the two groups at days 7 emergency department (ED) for acute exacerbations of and 21. asthma. CONCLUSIONS: A single dose of intramuscular betametha- PATIENTS AND METHODS: Patients with acute exacer- sone 12 mg was safe and as efficacious as prednisone in pre- bations of asthma who were suitable for discharge from the venting the relapse of acute asthma. -

Long-Term Budesonide Or Nedocromil Mineral Accretion Over a Period of Years
term inhaled corticosteroid (ICS) treatment on bone Long-term Budesonide or Nedocromil mineral accretion over a period of years. Treatment, Once Discontinued, Does Not Alter the Course of Mild to Moderate Asthma in STUDY POPULATION. Cohort follow-up study for a median Children and Adolescents of 7 years with 877 children 5 to 12 years of age who Strunk RC, Sternberg AL, Szefler SJ, et al. J Pediatr. had mild-to-moderate asthma and initially were ran- 2009;154(5):682–687 domly assigned in the Childhood Asthma Management Program. PURPOSE OF THE STUDY. To determine whether long-term, METHODS. Serial dual-energy x-ray absorptiometry scans continuous use of inhaled antiinflammatory medications of the lumbar spine to assess bone mineral density were affects asthma outcomes in children with mild-to-mod- performed for all patients. Annual bone mineral accre- erate asthma after use is discontinued. tion was calculated for 531 boys and 346 girls. STUDY POPULATION. A total of 941 children, 5 to 12 years of RESULTS. Oral corticosteroid bursts produced dose- age, who had previously participated in the Childhood dependent reductions in bone mineral accretion (0.052, Asthma Management Program (CAMP). 0.049, and 0.046 g/cm2 per year with 0, 1–4, and Ն5 courses, respectively) and increases in the risk for osteo- METHODS. During the CAMP trial, subjects received treat- penia (10%, 14%, and 21%, respectively) in boys but ment with budesonide, nedocromil, or placebo for 4.3 not girls. Cumulative ICS use was associated with a small years. During the posttrial period, asthma manage- decrease in bone mineral accretion in boys but not girls ment was provided by primary care physicians ac- but no increased risk for osteopenia. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -
![Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’](https://docslib.b-cdn.net/cover/3023/pharmacological-and-ionic-characterizations-of-the-muscarinic-receptors-modulating-3h-acetylcholine-release-from-rat-cortical-synaptosomes-753023.webp)
Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’
0270.6474/85/0505-1202$02.00/O The Journal of Neuroscience CopyrIght 0 Society for Neuroscrence Vol. 5, No. 5, pp. 1202-1207 Printed in U.S.A. May 1985 Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’ EDWIN M. MEYER* AND DEBORAH H. OTERO Department of Pharmacology and Therapeutics, University of Florida School of Medicine, Gainesville, Florida 32610 Abstract brain (Gonzales and Crews, 1984). M,-receptors, however, appear pre- and postsynaptically in brain, are regulated by an intrinsic The muscarinic receptors that modulate acetylcholine membrane protein that binds to GTP (g-protein), and may not be release from rat cortical synaptosomes were characterized coupled to changes in phosphatidylinositol turnover. with respect to sensitivity to drugs that act selectively at M, The present studies were designed to determine whether M,- or or Ma receptor subtypes, as well as to changes in ionic Mp-receptors mediate the presynaptic modulation of ACh release. strength and membrane potential. The modulatory receptors These studies involve dose-response curves for the release of appear to be of the M2 type, since they are activated by synaptosomal [3H]ACh in the presence of selected muscarinic ago- carbachol, acetylcholine, methacholine, oxotremorine, and nists and antagonists, as well as treatments that selectively alter MI- bethanechol, but not by pilocarpine, and are blocked by or M,-receptor activity. Our results indicate that the presynaptic atropine, scopolamine, and gallamine (at high concentra- modulation of [3H]ACh release is mediated by MP- but not MI- tions), but not by pirenzepine or dicyclomine. -

FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting
FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting August 31, 2020 sNDA 209482: fluticasone furoate/umeclidinium/vilanterol fixed dose combination to reduce all-cause mortality in patients with chronic obstructive pulmonary disease NDA209482/S-0008 PADAC Clinical and Statistical Briefing Document Fluticasone furoate/umeclidinium/vilanterol fixed dose combination for all-cause mortality DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the supplemental New Drug Application (sNDA) 209482, for fluticasone furoate/umeclidinium/vilanterol, as an inhaled fixed dose combination, for the reduction in all-cause mortality in patients with COPD, to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered -

Core Safety Profile
Core Safety Profile Active substance: Nedocromil Pharmaceutical form(s)/strength: Eye drops: 20 mg/ml, Inhalation vapour: 5 mg/ml, Pressurised inhalation: 2 mg/dose, 2mg/0,1 mg, Nebuliser solution: 10 mg/2 ml, Inhalation powder: 10 mg/dose, Nasal spray: 10 mg/ml P-RMS: CZ/H/PSUR/0016/001 Date of FAR: 09.10.2010 EU Core Safety Profile (CSP) For Nedocromil sodium NB: This CSP is combining safety information from the three existing pharmaceutical forms: Eye drops, Nasal spray and Inhaler. Information that is specific to one form is identified by a subheading. No subheading indicates that information is valid for all pharmaceuticals forms 4.3 Contraindications For eye drops <Product name> eye drops is contraindicated in patients with known hypersensitivity to nedocromil sodium, benzalkonium chloride or other constituents of the formulation. For Nasal spray and Inhaler <Product name> nasal spray or inhaler is contraindicated in patients with known hypersensitivity to any of the constituents. 4.4 Special warnings and precautions for use For eye drops Patients should be advised not to wear soft contact lenses during treatment with <product name> eye drops. Benzalkonium chloride, a constituent of the formulation, may accumulate in soft contact lenses. This preservative, when slowly released, could possibly irritate the cornea. In patients who continue to wear hard or gas permeable contact lenses during <product name> eye drops treatment, the lenses should be taken out of the eye prior to instillation of the drops. They should be inserted again not earlier than 10 minutes after administration, in order to allow an even conjunctival distribution of the solution. -

Model of Airway Inflammation in a Murine Asthma Airway
Platelet-Activating Factor Receptor Develops Airway Hyperresponsiveness Independently of Airway Inflammation in a Murine Asthma Model This information is current as of September 24, 2021. Satoshi Ishii, Takahide Nagase, Hideo Shindou, Hajime Takizawa, Yasuyoshi Ouchi and Takao Shimizu J Immunol 2004; 172:7095-7102; ; doi: 10.4049/jimmunol.172.11.7095 http://www.jimmunol.org/content/172/11/7095 Downloaded from References This article cites 69 articles, 31 of which you can access for free at: http://www.jimmunol.org/content/172/11/7095.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2004 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Platelet-Activating Factor Receptor Develops Airway Hyperresponsiveness Independently of Airway Inflammation in a Murine Asthma Model1 Satoshi Ishii,2*§ Takahide Nagase,† Hideo Shindou,*§ Hajime Takizawa,† Yasuyoshi Ouchi,‡ and Takao Shimizu*§ Lipid mediators play an important role in modulating inflammatory responses. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Drug Class Review Nasal Corticosteroids
Drug Class Review Nasal Corticosteroids Final Report Update 1 June 2008 The Agency for Healthcare Research and Quality has not yet seen or approved this report The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Dana Selover, MD Tracy Dana, MLS Colleen Smith, PharmD Kim Peterson, MS Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Marian McDonagh, PharmD, Principal Investigator, Drug Effectiveness Review Project Copyright © 2008 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 1 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION ..........................................................................................................................5 Scope and Key Questions .......................................................................................................................7 METHODS ....................................................................................................................................9 Literature Search .....................................................................................................................................9 -
Asthma Control
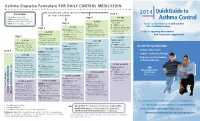
Asthma Stepwise Formulary FOR DAILY CONTROL MEDICATION QuickGuide to abbreviations: step 6 2014 • ICS: inhaled corticosteroid step 5 • LABA: long-acting beta2-agonist Asthma Control HIGH-DOSE ICS • LTRA: leukotriene receptor antagonist (per step 5) • SABA: short-acting beta2-agonist step 4 LTRA (per step 4) for the care of pediatric and adult patients + LTRA (per step 4) + HIGH-DOSE ICS with established asthma step 3 (mark choice): + oral systemic steroids MEDIUM-DOSE ICS fluticasone (Flovent) MDI: (lowest dose for the shortest (per step 3; mark a choice there) 110 mcg: 2 puffs twice daily duration: 5-10 mg is A tool for ongoing assessment considered low-dose) MEDIUM-DOSE ICS + LTRA: montelukast budesonide (Pulmicort) respules: and treatment adjustment step 2 (mark choice): (Singulair) by mouth: 1.0 mg: 1 respule twice daily 4 mg: 1 tablet once daily, or fluticasone (Flovent) MDI: 1 packet oral granules once daily 110 mcg: 1 puff twice daily HIGH-DOSE ICS budesonide (Pulmicort) respules: (per step 5) LOW-DOSE ICS (mark choice): LABA (per step 3) 0.50 mg: 1 respule twice daily + LABA (per step 4) fluticasone (Flovent) MDI: + HIGH-DOSE ICS LABA (per step 3) Inside the QuickGuide... 44 mcg: 2 puffs twice daily (mark choice): + oral systemic steroids budesonide (Pulmicort) respules: + MEDIUM-DOSE ICS fluticasone (Flovent) MDI: (lowest dose for the shortest 0.25 mg: 1 respule twice daily (mark choice): • Asthma control tables step 1 110 mcg: 2 puffs twice daily duration: 5-10 mg is considered low-dose) fluticasone (Flovent) -

The Pharmacological Studies on Intrinsic Activities of Acetylcholine, Methacholine, and Carbachol (Homologous Drugs) on Isolated Rat Ileum Preparation
Journal of Medicine and Medical Science Vol. 2(8) pp. 1047-1049, August 2011 Available online@ http://www.interesjournals.org/JMMS Copyright © 2011 International Research Journals Short Communication The pharmacological studies on intrinsic activities of acetylcholine, methacholine, and carbachol (Homologous Drugs) on isolated rat ileum preparation Peter I. Aziba* 1, Sokan J.O. 2, Ifedayo O. 2 and Kasim L.S. 2 1*Department of Pharmacology and 2Department of Pharmaceutical Chemistry Olabisi Onabanjo university, Oachs, Ago_Iwoye. Accepted 24 August, 2011 This study investigated the intrinsic activities of equimolar concentrations of three homologous drugs Actylcholine (Ach), Methacholine (Mch) and Carbachol (Cch) on isolated rat ileum preparation. Contractions were monitored on smoked drum fixed on a kymograph. Heights of contractions were measured in (mm) in order to assess their efficacies.In some experiments Ach- induced contractions were measured in the presence of atropine a competitive muscarinic antagonist. The result showed order of potencies, ranked as Cch>Mch>Ach. This result may explain the low intrinsic activities of Ach when compared to Cch, Mch, due to effect of acetylcholinesterase an enzyme which hydrolyze Ach and limit its efficacy in therapeutic use. Keywords: Intrinsic, homologous drugs, rat ileum, efficacy. INTRODUCTION Theoretically, the term intrinsic activity of a drug was first MATERIALS AND METHODS introduced by Ariens and Van Rossum (1957). The term has been used a great deal in their attempt to explain Rats between (200-305g) were used. The animals were why all drugs do not act in accordance with Clark’s theory maintained in well ventilated conditions, under constant of drug receptor interaction.