Model of Airway Inflammation in a Murine Asthma Airway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Protective Effects of Tiotropium Bromide in Patients with Airways Hyperres P O N S I V E N E S S
European Review for Medical and Pharmacological Sciences 2004; 8: 259-264 Early protective effects of tiotropium bromide in patients with airways hyperres p o n s i v e n e s s C. TERZANO, A. PETROIANNI, A. RICCI, L. D’ANTONI, L. ALLEGRA* Department of Cardiovascular and Respiratory Sciences, Respiratory Diseases Unit, Fondazione E. Lorillard Spencer Cenci, “La Sapienza” University - Rome (Italy) *Institute of Respiratory Diseases, University of Milan, Ospedale Maggiore IRCCS – Milan (Italy) Abstract. – Tiotropium is an anticholiner- Introduction gic drug for Ch ronic Obstructive Pulmonary Di sease (COPD) patients, with a peak b ron- Ti o t rop ium is a qu atern a ry amm o niu m chodilator effect observed after 1.5 to 2 hours and a long duration of action. The aim of our co ngener of atropine. It has been developed study was to quantify the early protection of a as a lon g-acting an ticho linergic bro n c h o d i l a- single dose of inhaled tiotropium against metha- tor for inhalation by patients with chronic ob- choline-induced bronchoconstriction in asthmat- s t ructive pu lmon ary d isease (COPD). Dru g ic patients with airway hyperresponsiveness. p ro p e rties o f ant icho lin ergic agent s have Ten subjects (7M, 3F), with history of asthma been well-kno wn to man y cultures for many and a baseline FEV (Forced Expiratory Volume 1 1 1 c e n t u r i e s . In the 1920s the d iscovery o f the sec) >80% of pred icted, were enrolled in the s t u d y. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -
![Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’](https://docslib.b-cdn.net/cover/3023/pharmacological-and-ionic-characterizations-of-the-muscarinic-receptors-modulating-3h-acetylcholine-release-from-rat-cortical-synaptosomes-753023.webp)
Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’
0270.6474/85/0505-1202$02.00/O The Journal of Neuroscience CopyrIght 0 Society for Neuroscrence Vol. 5, No. 5, pp. 1202-1207 Printed in U.S.A. May 1985 Pharmacological and Ionic Characterizations of the Muscarinic Receptors Modulating [3H]Acetylcholine Release from Rat Cortical Synaptosomes’ EDWIN M. MEYER* AND DEBORAH H. OTERO Department of Pharmacology and Therapeutics, University of Florida School of Medicine, Gainesville, Florida 32610 Abstract brain (Gonzales and Crews, 1984). M,-receptors, however, appear pre- and postsynaptically in brain, are regulated by an intrinsic The muscarinic receptors that modulate acetylcholine membrane protein that binds to GTP (g-protein), and may not be release from rat cortical synaptosomes were characterized coupled to changes in phosphatidylinositol turnover. with respect to sensitivity to drugs that act selectively at M, The present studies were designed to determine whether M,- or or Ma receptor subtypes, as well as to changes in ionic Mp-receptors mediate the presynaptic modulation of ACh release. strength and membrane potential. The modulatory receptors These studies involve dose-response curves for the release of appear to be of the M2 type, since they are activated by synaptosomal [3H]ACh in the presence of selected muscarinic ago- carbachol, acetylcholine, methacholine, oxotremorine, and nists and antagonists, as well as treatments that selectively alter MI- bethanechol, but not by pilocarpine, and are blocked by or M,-receptor activity. Our results indicate that the presynaptic atropine, scopolamine, and gallamine (at high concentra- modulation of [3H]ACh release is mediated by MP- but not MI- tions), but not by pirenzepine or dicyclomine. -

Protective Effects of Inhaled Ipratropium Bromide on Bronchoconstriction Induced by Adenosine and Methacholine in Asthma
Eur Aesplr J 1992, 5, 56()-665 Protective effects of inhaled ipratropium bromide on bronchoconstriction induced by adenosine and methacholine In asthma N. Crimi, F. Palermo, R. Oliveri, R. Polosa, I. Settinieri, A. Mistretta Protective effects of inhaled ipratropium bromide on bronchoconstriction induced by Istituto di Malattie dell' Apparato adenosine and methacholine in asthma. N. Crimi, F. Palermo, R. Oliveri, R. Po/osa, Respiratorio e Tisiologia, Universita' di Catania, Catania, Italy. I. Seuinier~ A. Mistretta. ABSTRACT: Although adenosine-Induced bronchoconstrictlon is mainly due to Correspondence: N. Crimi mast cell mediator release, vagal reflexes have also been Implicated in this Istituto di Malattie dell' Appara.to response. Respiratorio e Tisiologia We have Investigated the effect of a speciflc muscarlnlc-receptor antagonist, Universita' di Catania ipratroplum bromide, on methacholine- and adenosine-Induced bronchoconstriction Via Passo Gravina 187 In a randomized, placebo-controlled, double-blind study of 12 asthmatic subjects. 95125 Catania Airway response was evaluated as forced expiratory volume in one second (FEV,). Italy Inhaled lpratroplum bromide (40 Jlg), administered 20 mln prior to bronchoprovocation, Increased the provocation dose of Inhaled methacholine and Keywords: Adenosine adenosine required to reduce FEV, by 20% from baseline (PD,.) from 0.11 to 0.79 asthma ipratropium bromide mg (p<O.Ol) and from 0.57 to 1.27 mg (p<0.01), respectively. The mean baseline methacholine FEV, values after administration of lpratroplum bromide were signlfkantly higher than after placebo administration (p<O.OS). However, there was no correlation Received: May 22 1991 between the degree of bronchodllatatlon and dose-ratios for methacholine and Accepted after revision January 7 1992 adenosine. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

The Pharmacological Studies on Intrinsic Activities of Acetylcholine, Methacholine, and Carbachol (Homologous Drugs) on Isolated Rat Ileum Preparation
Journal of Medicine and Medical Science Vol. 2(8) pp. 1047-1049, August 2011 Available online@ http://www.interesjournals.org/JMMS Copyright © 2011 International Research Journals Short Communication The pharmacological studies on intrinsic activities of acetylcholine, methacholine, and carbachol (Homologous Drugs) on isolated rat ileum preparation Peter I. Aziba* 1, Sokan J.O. 2, Ifedayo O. 2 and Kasim L.S. 2 1*Department of Pharmacology and 2Department of Pharmaceutical Chemistry Olabisi Onabanjo university, Oachs, Ago_Iwoye. Accepted 24 August, 2011 This study investigated the intrinsic activities of equimolar concentrations of three homologous drugs Actylcholine (Ach), Methacholine (Mch) and Carbachol (Cch) on isolated rat ileum preparation. Contractions were monitored on smoked drum fixed on a kymograph. Heights of contractions were measured in (mm) in order to assess their efficacies.In some experiments Ach- induced contractions were measured in the presence of atropine a competitive muscarinic antagonist. The result showed order of potencies, ranked as Cch>Mch>Ach. This result may explain the low intrinsic activities of Ach when compared to Cch, Mch, due to effect of acetylcholinesterase an enzyme which hydrolyze Ach and limit its efficacy in therapeutic use. Keywords: Intrinsic, homologous drugs, rat ileum, efficacy. INTRODUCTION Theoretically, the term intrinsic activity of a drug was first MATERIALS AND METHODS introduced by Ariens and Van Rossum (1957). The term has been used a great deal in their attempt to explain Rats between (200-305g) were used. The animals were why all drugs do not act in accordance with Clark’s theory maintained in well ventilated conditions, under constant of drug receptor interaction. -
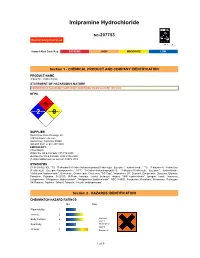
Imipramine Hydrochloride
Imipramine Hydrochloride sc-207753 Material Safety Data Sheet Hazard Alert Code Key: EXTREME HIGH MODERATE LOW Section 1 - CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME Imipramine Hydrochloride STATEMENT OF HAZARDOUS NATURE CONSIDERED A HAZARDOUS SUBSTANCE ACCORDING TO OSHA 29 CFR 1910.1200. NFPA FLAMMABILITY1 HEALTH2 HAZARD INSTABILITY0 SUPPLIER Santa Cruz Biotechnology, Inc. 2145 Delaware Avenue Santa Cruz, California 95060 800.457.3801 or 831.457.3800 EMERGENCY: ChemWatch Within the US & Canada: 877-715-9305 Outside the US & Canada: +800 2436 2255 (1-800-CHEMCALL) or call +613 9573 3112 SYNONYMS C19-H24-N2.HCl, "10, 11-dihydro-5-(3-(dimethylamino)propyl)5Hdibenz[b, f]azepine", hydrochloride, "10, 11-dihydro-N, N-dimethyl- 5H-dibenz[b, f]azepine-5-propanamine HCl", "5-(3-dimethylaminopropyl)-10, 11-dihydro-5H-dibenz[b, f]azepine", hydrochloride, "Antideprin Hydrochloride", Berkomine, Chimoreptin, Chrytemin, "CO Cap", "Imipramine 25", Deprinol, Dimipressin, Dynazina, Efuranol, Feinalmin, Fujisawa, G-22150, IA-Pram, Imavate, Imidol, Imilanyle, Imiprin, "IMP hydrochloride", Iprogen, Iramil, Janimime, Lofepramine, "Melipramin Hydrochloride", "Melipramine Hydrochloride", NSC-114900, Persamine, Pertofram, Presamine, Pryleugan, SK-Pramine, Teperine, Tofranil, Tofranile, "tricyclic antidepressant" Section 2 - HAZARDS IDENTIFICATION CHEMWATCH HAZARD RATINGS Min Max Flammability: 1 Toxicity: 2 Body Contact: 2 Min/Nil=0 Low=1 Reactivity: 1 Moderate=2 High=3 Chronic: 3 Extreme=4 1 of 9 CANADIAN WHMIS SYMBOLS EMERGENCY OVERVIEW RISK Harmful if swallowed. Irritating to eyes, respiratory system and skin. POTENTIAL HEALTH EFFECTS ACUTE HEALTH EFFECTS SWALLOWED ! Accidental ingestion of the material may be harmful; animal experiments indicate that ingestion of less than 150 gram may be fatal or may produce serious damage to the health of the individual. -

Additions and Deletions to the Drug Product List
Prescription and Over-the-Counter Drug Product List 36TH EDITION Cumulative Supplement Number 10 : October 2016 ADDITIONS/DELETIONS FOR PRESCRIPTION DRUG PRODUCT LIST ABACAVIR SULFATE TABLET;ORAL ABACAVIR SULFATE >A> AB STRIDES ARCOLAB LTD EQ 300MG BASE A 091050 001 Oct 28, 2016 Oct NEWA ACETAMINOPHEN; BUTALBITAL TABLET;ORAL BUTALBITAL AND ACETAMINOPHEN >A> AA MIKART INC 300MG;50MG A 207386 001 Nov 15, 2016 Oct NEWA >D> + NEXGEN PHARMA 300MG;50MG A 090956 001 Aug 23, 2011 Oct CTEC >A> AA + 300MG;50MG A 090956 001 Aug 23, 2011 Oct CTEC ACETAMINOPHEN; BUTALBITAL; CAFFEINE CAPSULE;ORAL BUTALBITAL, ACETAMINOPHEN AND CAFFEINE >D> + NEXGEN PHARMA 300MG;50MG;40MG A 040885 001 Nov 16, 2009 Oct CFTG >A> AB + 300MG;50MG;40MG A 040885 001 Nov 16, 2009 Oct CFTG >A> AB NUVO PHARM INC 300MG;50MG;40MG A 207118 001 Oct 28, 2016 Oct NEWA ACETAZOLAMIDE TABLET;ORAL ACETAZOLAMIDE >A> AB HERITAGE PHARMA 125MG A 205530 001 Oct 27, 2016 Oct NEWA >A> AB 250MG A 205530 002 Oct 27, 2016 Oct NEWA ALBUTEROL SULFATE TABLET;ORAL ALBUTEROL SULFATE >A> @ DAVA PHARMS INC EQ 2MG BASE A 072860 002 Dec 20, 1989 Oct CMS1 ALENDRONATE SODIUM TABLET;ORAL ALENDRONATE SODIUM >D> @ SANDOZ EQ 5MG BASE A 075871 001 Apr 22, 2009 Oct CAHN >D> @ EQ 10MG BASE A 075871 002 Apr 22, 2009 Oct CAHN >D> @ EQ 35MG BASE A 075871 004 Apr 22, 2009 Oct CAHN >D> @ EQ 40MG BASE A 075871 003 Apr 22, 2009 Oct CAHN >D> @ EQ 70MG BASE A 075871 005 Apr 22, 2009 Oct CAHN >A> @ UPSHER-SMITH LABS EQ 5MG BASE A 075871 001 Apr 22, 2009 Oct CAHN >A> @ EQ 10MG BASE A 075871 002 Apr 22, 2009 Oct CAHN >A> @ EQ -

207930Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 207930Orig1s000 PHARMACOLOGY REVIEW(S) Pharmacology and Toxicology Secondary Review for NDA 207930 TO: NDA 207930 (UTIBRON NEOHALER; Combination of glycopyrrolate and indacaterol) FROM: Timothy W. Robison, Ph.D., D.A.B.T. Pharmacology and Toxicology Team Leader Division of Pulmonary, Allergy, and Rheumatology Products DATE: October 1, 2015 NDA 207930 is a 505(b)(1) application for UTIBRON NEOHALER. UTIBRON NEOHALER is a fixed dose combination, in a dry powder inhaler, of glycopyrrolate (NVA237)15.6 mcg (salt) and indacaterol maleate (QAB149) 27.5 mcg (base). The combination was designated as QVA149. The formulation includes magnesium stearate and lactose monohydrate as excipients. The maximum recommended dose is one actuation twice daily (BID) or 31.2 mcg glycopyrrolate and 55 mcg indacaterol per day. UTIBRON NEOHALER is indicated for the long-term, maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema. Dr. Sohn’s reviews dated July 7, 2015 and September 24, 2015 focused on the nonclinical safety assessment of the glycopyrrolate monoproduct and the combination of glycopyrrolate and indacaterol. The Sponsor previously received FDA approval of the indacaterol monoproduct, (NDA 22383). I concur with the recommendations of Dr. Sohn’s reviews dated July 7, 2015 and September 24, 2015 that the nonclinical pharmacology and toxicology of the glycopyrrolate monoproduct and the combination of glycopyrrolate and indacaterol have been adequately studied and should be approved from the nonclinical perspective. The Sponsor has complete nonclinical development programs for the glycopyrrolate and indacaterol monoproducts as well as the combination of glycopyrrolate and indacaterol. -

A Comparative Study of the Effects of Four Choline Esters on the Secretion of Fluid and Glycoprotein from Rat Submandibular Glands
A Comparative Study of the Effects of Four Choline Esters on the Secretion of Fluid and Glycoprotein from Rat Submandibular Glands Yoshiki IWABUCHI, Chihiro AOKI and Taizo MASUHARA Department of Dental Pharmacology, School of Dentistry at Niigata, The Nippon Dental University, Niigata 951, Japan Accepted June 16, 1988 Abstract-The actions of four choline esters, acetylcholine (ACH), methacholine (MET), carbachol (CAR) and bethanechol (BET), on the secretion of saliva and the specific glycoprotein (GP) contained in the secretory cells of the submandibular gland (SMG) of the rat were compared under conditions with and without physo stigmine (PHY). The ED50 values with respect to salivation were 17 mg/kg for ACH, 1060 ag/kg for BET, 810 zig/kg for MET and 75 ug/kg for CAR, whereas after pretreatment with PHY, ED50 values were lowered to 7.5 mg/kg for ACH and 212 fig/kg for MET, but remained unchanged for CAR and BET. SDS-polyacrylamide gel electrophoresis demonstrated that the saliva from the SMG elicited by the four choline esters contained GP I (130 KDa) and GP IV (21.5 KDa), characteristic of the acinus, and a band of GP III (31 KDa), which originates from the granular tubules. The order of intensity of these bands was band l>>band lll=band IV. Among these bands, band I increased in intensity in a dose-dependent manner. These results suggest that the four choline esters act mainly on the acinar cells, but exert some effects on the granular tubules of the rat SMG. In a study on five choline esters, acetyl granular convoluted tubules are secreted in choline, methacholine, carbachol, ethyl ether response to methoxamine at optimal doses of methacholine and carbachol, Molitor (1) (6, 9, 10) and dopamine at large doses (8). -

Care Management and Referral Guidelines
CARE MANAGEMENT AND REFERRAL GUIDELINES 2018 EDITION These Care Management and Referral Guidelines were approved by the HHP Quality and Clinical Integration committee. They are available on the Hawai‘i Pacific Health intranet and Hawai‘i Pacific Health and Hawai‘i Health Partners websites. TABLE OF CONTENTS Disclaimer. 3 Authors/Contributors. 3 Foreword. 4 Purpose. 5 Ownership of Guidelines and Archiving. 5 Methodology . 5 Development of the Care Management and Referral Guidelines . 5 Selection of Topics. 5 CM/RGs Development Workgroup . 6 Dissemination of the Care Management and Referral Guidelines. 7 Updating of the Care Management and Referral Guidelines. 7 Updating Process of Care Manaagement and Referral Guidelines Flowchart. 8 Monitoring and Evaluation. 9 ADULT / PEDIATRIC Allergy/Immunotherapy. 12 Stepwise approach for managing asthma in youths ≥ 12 years of age and adults. 14 Bone and Joint. 16 Otolaryngology. 19 Pulmonary Medicine . 21 ADULT Gastroenterology. 26 Neurology . 29 Ophthalmology. 30 Urology . 31 Adult Behavioral Health Treatment for Generalized Anxiety Disorder Alogrithm. 33 Treatment for Generalized Anxiety Disorder. 34 1st Line of Medications. 34 2nd Line of Medications . 34 Anxiety Medication Related Problems & Considerations. 35 Major Depressive Disorder Algorithm . 36 Interpretation of PHQ-9 Scores for Major Depressive Disorder . 37 Treatment for Major Depressive Disorder. 37 1st Line of Medications. 37 2nd Line of Medications . 37 Depression Medication Related Problems & Considerations. 38 Mood Disorder and Bipolar Algorithm. 39 TABLE OF CONTENTS | 1 TABLE OF CONTENTS continued Pharmacologic Treatment for Manic Phase. 40 Pharmacologic Treatment for Depression. 40 Pharmacologic Treatment for Maintenance . 41 PEDIATRIC Initial Evaluation of a Patient with Chest Pain. 44 Constipation Work-up and Management Algorithm. -

2020 Aetna Standard Plan
Plan for your best health Aetna Standard Plan Aetna.com Aetna is the brand name used for products and services provided by one or more of the Aetna group of subsidiary companies, including Aetna Life Insurance Company and its affiliates (Aetna). Aetna Pharmacy Management refers to an internal business unit of Aetna Health Management, LLC. Aetna Pharmacy Management administers, but does not offer, insure or otherwise underwrite the prescription drug benefits portion of your health plan and has no financial responsibility therefor. 2020 Pharmacy Drug Guide - Aetna Standard Plan Table of Contents INFORMATIONAL SECTION..................................................................................................................6 *ADHD/ANTI-NARCOLEPSY/ANTI-OBESITY/ANOREXIANTS* - DRUGS FOR THE NERVOUS SYSTEM.................................................................................................................................16 *ALLERGENIC EXTRACTS/BIOLOGICALS MISC* - BIOLOGICAL AGENTS...............................18 *ALTERNATIVE MEDICINES* - VITAMINS AND MINERALS....................................................... 19 *AMEBICIDES* - DRUGS FOR INFECTIONS.....................................................................................19 *AMINOGLYCOSIDES* - DRUGS FOR INFECTIONS.......................................................................19 *ANALGESICS - ANTI-INFLAMMATORY* - DRUGS FOR PAIN AND FEVER............................19 *ANALGESICS - NONNARCOTIC* - DRUGS FOR PAIN AND FEVER.........................................