Glossary Animal Physiology Circulatory System (See Also Human Biology 1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Buzzle – Zoology Terms – Glossary of Biology Terms and Definitions Http
Buzzle – Zoology Terms – Glossary of Biology Terms and Definitions http://www.buzzle.com/articles/biology-terms-glossary-of-biology-terms-and- definitions.html#ZoologyGlossary Biology is the branch of science concerned with the study of life: structure, growth, functioning and evolution of living things. This discipline of science comprises three sub-disciplines that are botany (study of plants), Zoology (study of animals) and Microbiology (study of microorganisms). This vast subject of science involves the usage of myriads of biology terms, which are essential to be comprehended correctly. People involved in the science field encounter innumerable jargons during their study, research or work. Moreover, since science is a part of everybody's life, it is something that is important to all individuals. A Abdomen: Abdomen in mammals is the portion of the body which is located below the rib cage, and in arthropods below the thorax. It is the cavity that contains stomach, intestines, etc. Abscission: Abscission is a process of shedding or separating part of an organism from the rest of it. Common examples are that of, plant parts like leaves, fruits, flowers and bark being separated from the plant. Accidental: Accidental refers to the occurrences or existence of all those species that would not be found in a particular region under normal circumstances. Acclimation: Acclimation refers to the morphological and/or physiological changes experienced by various organisms to adapt or accustom themselves to a new climate or environment. Active Transport: The movement of cellular substances like ions or molecules by traveling across the membrane, towards a higher level of concentration while consuming energy. -

Spectral Sensitivities of Wolf Spider Eyes
=ORNELL UNIVERSITY ~',lC.V~;AL ~ULLE(.~E DEF'ARY~,:ENT OF P~-I:~IOLOGY 1300 YORK AVE.~UE NEW YORK, N.Y. Spectral Sensitivities of Wolf Spider Eyes ROBERT D. DBVOE, RALPH J. W. SMALL, and JANIS E. ZVARGULIS From the Department of Physiology, The Johns Hopkins University School of Medicine, Baltimore, Maryland 21205 ABSTRACT ERG's to spectral lights were recorded from all eyes of intact wolf spiders. Secondary eyes have maximum relative sensitivities at 505-510 nm which are unchanged by chromatic adaptations. Principal eyes have ultraviolet sensitivities which are 10 to 100 times greater at 380 nm than at 505 nm. How- ever, two animals' eyes initially had greater blue-green sensitivities, then in 7 to 10 wk dropped 4 to 6 log units in absolute sensitivity in the visible, less in the ultraviolet. Chromatic adaptations of both types of principal eyes hardly changed relative spectral sensitivities. Small decreases in relative sensitivity in the visible with orange adaptations were possibly retinomotor in origin. Second peaks in ERG waveforms were elicited from ultraviolet-adapted principal eyes by wavelengths 400 nm and longer, and from blue-, yellow-, and orange- adapted secondary eyes by wavelengths 580 nm and longer. The second peaks in waveforms were most likely responses of unilluminated eyes to scattered light. It is concluded that both principal and secondary eyes contain cells with a visual pigment absorbing maximally at 505-510 nm. The variable absolute and ultraviolet sensitivities of principal eyes may be due to a second pigment in the same cells or to an ultraviolet-absorbing accessory pigment which excites the 505 nm absorbing visual pigment by radiationless energy transfer. -

THE CASE AGAINST Marine Mammals in Captivity Authors: Naomi A
s l a m m a y t T i M S N v I i A e G t A n i p E S r a A C a C E H n T M i THE CASE AGAINST Marine Mammals in Captivity The Humane Society of the United State s/ World Society for the Protection of Animals 2009 1 1 1 2 0 A M , n o t s o g B r o . 1 a 0 s 2 u - e a t i p s u S w , t e e r t S h t u o S 9 8 THE CASE AGAINST Marine Mammals in Captivity Authors: Naomi A. Rose, E.C.M. Parsons, and Richard Farinato, 4th edition Editors: Naomi A. Rose and Debra Firmani, 4th edition ©2009 The Humane Society of the United States and the World Society for the Protection of Animals. All rights reserved. ©2008 The HSUS. All rights reserved. Printed on recycled paper, acid free and elemental chlorine free, with soy-based ink. Cover: ©iStockphoto.com/Ying Ying Wong Overview n the debate over marine mammals in captivity, the of the natural environment. The truth is that marine mammals have evolved physically and behaviorally to survive these rigors. public display industry maintains that marine mammal For example, nearly every kind of marine mammal, from sea lion Iexhibits serve a valuable conservation function, people to dolphin, travels large distances daily in a search for food. In learn important information from seeing live animals, and captivity, natural feeding and foraging patterns are completely lost. -

The Polyp and the Medusa Life on the Move
The Polyp and the Medusa Life on the Move Millions of years ago, unlikely pioneers sparked a revolution. Cnidarians set animal life in motion. So much of what we take for granted today began with Cnidarians. FROM SHAPE OF LIFE The Polyp and the Medusa Life on the Move Take a moment to follow these instructions: Raise your right hand in front of your eyes. Make a fist. Make the peace sign with your first and second fingers. Make a fist again. Open your hand. Read the next paragraph. What you just did was exhibit a trait we associate with all animals, a trait called, quite simply, movement. And not only did you just move your hand, but you moved it after passing the idea of movement through your brain and nerve cells to command the muscles in your hand to obey. To do this, your body needs muscles to move and nerves to transmit and coordinate movement, whether voluntary or involuntary. The bit of business involved in making fists and peace signs is pretty complex behavior, but it pales by comparison with the suites of thought and movement associated with throwing a curve ball, walking, swimming, dancing, breathing, landing an airplane, running down prey, or fleeing a predator. But whether by thought or instinct, you and all animals except sponges have the ability to move and to carry out complex sequences of movement called behavior. In fact, movement is such a basic part of being an animal that we tend to define animalness as having the ability to move and behave. -

Seeing Through Moving Eyes
bioRxiv preprint doi: https://doi.org/10.1101/083691; this version posted June 1, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Seeing through moving eyes - microsaccadic information sampling provides 2 Drosophila hyperacute vision 3 4 Mikko Juusola1,2*‡, An Dau2‡, Zhuoyi Song2‡, Narendra Solanki2, Diana Rien1,2, David Jaciuch2, 5 Sidhartha Dongre2, Florence Blanchard2, Gonzalo G. de Polavieja3, Roger C. Hardie4 and Jouni 6 Takalo2 7 8 1National Key laboratory of Cognitive Neuroscience and Learning, Beijing, Beijing Normal 9 University, Beijing 100875, China 10 2Department of Biomedical Science, University of Sheffield, Sheffield S10 T2N, UK 11 3Champalimaud Neuroscience Programme, Champalimaud Center for the Unknown, Lisbon, 12 Portugal 13 4Department of Physiology Development and Neuroscience, Cambridge University, Cambridge CB2 14 3EG, UK 15 16 *Correspondence to: [email protected] 17 ‡ Equal contribution 18 19 Small fly eyes should not see fine image details. Because flies exhibit saccadic visual behaviors 20 and their compound eyes have relatively few ommatidia (sampling points), their photoreceptors 21 would be expected to generate blurry and coarse retinal images of the world. Here we 22 demonstrate that Drosophila see the world far better than predicted from the classic theories. 23 By using electrophysiological, optical and behavioral assays, we found that R1-R6 24 photoreceptors’ encoding capacity in time is maximized to fast high-contrast bursts, which 25 resemble their light input during saccadic behaviors. Whilst over space, R1-R6s resolve moving 26 objects at saccadic speeds beyond the predicted motion-blur-limit. -

Introduction; Environment & Review of Eyes in Different Species
The Biological Vision System: Introduction; Environment & Review of Eyes in Different Species James T. Fulton https://neuronresearch.net/vision/ Abstract: Keywords: Biological, Human, Vision, phylogeny, vitamin A, Electrolytic Theory of the Neuron, liquid crystal, Activa, anatomy, histology, cytology PROCESSES IN BIOLOGICAL VISION: including, ELECTROCHEMISTRY OF THE NEURON Introduction 1- 1 1 Introduction, Phylogeny & Generic Forms 1 “Vision is the process of discovering from images what is present in the world, and where it is” (Marr, 1985) ***When encountering a citation to a Section number in the following material, the first numeric is a chapter number. All cited chapters can be found at https://neuronresearch.net/vision/document.htm *** 1.1 Introduction While the material in this work is designed for the graduate student undertaking independent study of the vision sensory modality of the biological system, with a certain amount of mathematical sophistication on the part of the reader, the major emphasis is on specific models down to specific circuits used within the neuron. The Chapters are written to stand-alone as much as possible following the block diagram in Section 1.5. However, this requires frequent cross-references to other Chapters as the analyses proceed. The results can be followed by anyone with a college degree in Science. However, to replicate the (photon) Excitation/De-excitation Equation, a background in differential equations and integration-by-parts is required. Some background in semiconductor physics is necessary to understand how the active element within a neuron operates and the unique character of liquid-crystalline water (the backbone of the neural system). The level of sophistication in the animal vision system is quite remarkable. -

Eukaryote Cell Biology - Michelle Gehringer
FUNDAMENTALS OF BIOCHEMISTRY, CELL BIOLOGY AND BIOPHYSICS – Vol. II - Eukaryote Cell Biology - Michelle Gehringer EUKARYOTE CELL BIOLOGY Michelle Gehringer Department of Biochemistry and Microbiology, University of Port Elizabeth, South Africa Keywords: cell theory, cell diversity, eukaryote cell structure, nucleus, chromatin, DNA, organelles, mitochondria, chloroplasts, transcription, RNA, translation, ribosomes, cell cycle, interphase, mitosis, meiosis, signal transduction, growth regulation, cancer, oncogenesis. Contents 1. Introduction 1.1. The first cell 2. Origin of Eukaryotes 3. Cellular differentiation in multicellular organisms 3.1. Plants 3.2. Animals 4. Eukaryotic cell structure 5. Organization of eukaryotic cells 5.1. Plasma membrane 5.2. Extracellular matrices 5.3. Protein synthesis and transport 5.4. Cytoskeleton and movement 5.5. Nucleus 5.5.1 Genomes 5.5.2 Gene expression 5.5.3 Maintaining the genome 5.6. Organelles 6. The cell cycle 6.1. Mitosis 6.2. Meiosis 7. Regulation of cell growth 7.1. Signal transduction 7.2. Programmed cell death 7.3. CancerUNESCO – EOLSS 8. Experimental Models 8.1. Yeast SAMPLE CHAPTERS 8.2. Arabidopsis 8.3. Drosophila 8.4. The mouse 8.5. Cell culture 8.6. Separation of cellular contents 8.7. Tracing biochemical pathways 9. Future Investigations Glossary Bibliography ©Encyclopedia of Life Support Systems (EOLSS) FUNDAMENTALS OF BIOCHEMISTRY, CELL BIOLOGY AND BIOPHYSICS – Vol. II - Eukaryote Cell Biology - Michelle Gehringer Biographical Sketch Summary Cells form the basic unit of life on our planet. They are well organized systems which perform all the essential tasks of eating, respiring, replicating and excreting waste products. The first cells, which are thought to have evolved about 3.8 billion years ago, much resembled present day prokaryotes. -
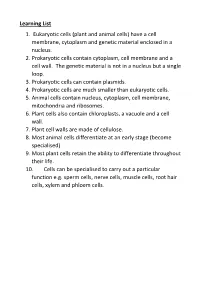
Learning List 1. Eukaryotic Cells (Plant and Animal Cells) Have a Cell Membrane, Cytoplasm and Genetic Material Enclosed in a Nucleus
Learning List 1. Eukaryotic cells (plant and animal cells) have a cell membrane, cytoplasm and genetic material enclosed in a nucleus. 2. Prokaryotic cells contain cytoplasm, cell membrane and a cell wall. The genetic material is not in a nucleus but a single loop. 3. Prokaryotic cells can contain plasmids. 4. Prokaryotic cells are much smaller than eukaryotic cells. 5. Animal cells contain nucleus, cytoplasm, cell membrane, mitochondria and ribosomes. 6. Plant cells also contain chloroplasts, a vacuole and a cell wall. 7. Plant cell walls are made of cellulose. 8. Most animal cells differentiate at an early stage (become specialised) 9. Most plant cells retain the ability to differentiate throughout their life. 10. Cells can be specialised to carry out a particular function e.g. sperm cells, nerve cells, muscle cells, root hair cells, xylem and phloem cells. Cells All living things are made of ________________. Cells can either be ____________________ or ________________________. Plants and animal cells are _________________________. Label the diagram of a plant and animal cell. Compare the structure of a plant and animal cell Bacteria are _______________________ cells. Label the diagram of a bacterial cell. Complete the Venn Diagram to compare eukaryotic and prokaryotic cells Eukaryotic Prokaryotic Function of cell organelles Learning List – Microscopes 1. Light microscopes use light and lenses to form an image of a specimen. 2. Light microscopes are used to se nuclei, chloroplasts, cell wall, cell membrane and mitochondria. Electron microscopes use electrons to form an image. 3. Stains are used to make the specimen visible. 4. Electron microscopes have a higher magnification. -
Animal Models of Fungal Infection: Critical Systems in Development Of
Animal Models of Fungal Infection Critical Systems in Development of New Antifungal Agents Thomas J. Walsh, MD, PhD (hon), FAAM, FIDSA, FECMM, FAAAS Founding Director, Transplantation-Oncology Infectious Diseases Program Chief, Infectious Diseases Translational Research Laboratory Professor of Medicine, Pediatrics, and Microbiology & Immunology Weill Cornell Medical Center of Cornell University Attending Physician, New York Presbyterian Hospital and Hospital for Special Surgery Adjunct Professor of Medicine, University of Maryland School of Medicine Adjunct Professor of Pathology, The Johns Hopkins University School of Medicine Disclosures/Disclaimers • Disclosures: Dr. Walsh has received grants for experimental and clinical antimicrobial pharmacology and therapeutics to his institution from Allergan, Amplyx, Astellas, Lediant, Medicines Company, Merck, Scynexis, Tetraphase, and Viosera and has served as consultant to Amplyx, Astellas, Allergan, ContraFect, Gilead, Lediant, Medicines Company, Merck, Methylgene, Pfizer, and Scynexis • Disclaimers: The views expressed in this talk represent my opinions and do not necessarily represent the views of Weill Cornell Medicine or those of the FDA. Background • Animal model systems are a critical component of the process of discovery and development of new antifungal agents for treatment and prevention of invasive fungal diseases (IFDs). • Models of IFDs in murine, rat, guinea pigs, and rabbits have been developed and studied for development of new systemic antifungal agents. • We will review the conceptual, scientific, and regulatory framework for utilizing these models, cite specific examples of their application, and discuss their predictability for clinical trials. Objectives • Review role of laboratory animal model systems in development of new antifungal agents. • Assess the predictability of these models for predicting outcome in clinical trials. -

University of Groningen Colour in the Eyes of Insects Stavenga, D.G
University of Groningen Colour in the eyes of insects Stavenga, D.G. Published in: Journal of Comparative Physiology A; Sensory Neural, and Behavioral Physiology DOI: 10.1007/s00359-002-0307-9 IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2002 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Stavenga, D. G. (2002). Colour in the eyes of insects. Journal of Comparative Physiology A; Sensory Neural, and Behavioral Physiology, 188(5), 337-348. https://doi.org/10.1007/s00359-002-0307-9 Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 26-09-2021 J Comp Physiol A (2002) 188: 337–348 DOI 10.1007/s00359-002-0307-9 REVIEW D.G. Stavenga Colour in the eyes of insects Accepted: 15 March 2002 / Published online: 13 April 2002 Ó Springer-Verlag 2002 Abstract Many insect species have darkly coloured provide the input for the visual neuropiles, which eyes, but distinct colours or patterns are frequently process the light signals to detect motion, colours, or featured. -

Description of the Eukaryotic Animal Cell by Kayla Underwood General
Description of the Eukaryotic Animal Cell By Kayla Underwood General Description The animal cell is the basic unit of life in the animal body. Cells are the building blocks of more complicated structures and they are specialized to carry out specialized functions. Cells are highly organized structures and in order to be successful in carrying out its functions they must be able to separate its contents from the external environment. Eukaryotic cell size is limited and it ranges from ten to one-hundred micrometers in diameter. The eukaryotic animal cell has a plasma membrane that surrounds the cell along with internal structures that are referred to as organelles. Organelles are specialized to carry out specific functions such as converting energy to usable forms, synthesizing compounds, and manufacturing structures that are essential to function and reproduction. Major Structures As figure 1 indicates, the major structures of the eukaryotic animal cell are the plasma membrane, the Golgi complex, the nucleus, which contains the nucleolus, a nuclear envelope, and nuclear pores, the endoplasmic reticulum (rough and smooth), lysosomes, mitochondria, peroxizomes, microfilaments, microtubules, cilia, and the centrioles. Each structure is described below. Figure 1: Anatomy of the Animal Cell Source: © 1995-2005 by Michael W. Davidson and the Florida State University. Retrieved May 4, 2005 from http://micro.magnet.fsu.edu/cells/animalcell.html Plasma Membrane A structure that surrounds all cells with the function of separating the cells contents from the outside environment. The plasma membrane serves as a selective barrier in that it only allows certain exchanges to take place between the internal area of the cell and the outside environment. -

The Secrets of Fossils Lesson by Tucker Hirsch
The Secrets of Fossils Lesson by Tucker Hirsch Video Titles: Introduction: A New view of the Evolution of Animals Cambrian Explosion Jenny Clack, Paleontologist: The First Vertebrate Walks on Land Des Collins, Paleontologist: The Burgess Shale Activity Subject: Assessing evolutionary links NEXT GENERATION SCIENCE STANDARDS and evidence from comparative analysis of the fossil MS-LS4-1 Analyze and interpret data for patterns record and modern day organisms. in the fossil record that document the existence, diversity, extinction, and change of life forms Grade Level: 6 – 8 grades throughout the history of life on Earth under the Introduction assumptions that natural laws operate today as In this lesson students make connections between in the past. [Clarification Statement: Emphasis fossils and modern day organisms. Using the is on finding patterns of changes in the level of information about the Cambrian Explosion, they complexity of anatomical structures in organisms explore theories about how and why organisms diversified. Students hypothesize what evidence and the chronological order of fossil appearance might be helpful to connect fossil organisms to in the rock layers.] [Assessment Boundary: modern organisms to show evolutionary connections. Assessment does not include the names of Students use three videos from shapeoflife.org. individual species or geological eras in the fossil record.] Assessments Written MS-LS4-2 Apply scientific ideas to construct an Time 100-120 minutes (2 class periods) explanation for the anatomical similarities and Group Size Varies; single student, student pairs, differences among modern organisms and between entire class modern and fossil organisms to infer evolutionary relationships. [Clarification Statement: Emphasis Materials and Preparation is on explanations of the evolutionary relationships • Access to the Internet to watch 4 Shape of Life videos among organisms in terms of similarity or • Video Worksheet differences of the gross appearance of anatomical • “Ancient-Modern” Activity.