Paranoid – Suspicious; Argumentative; Paranoid; Continually on the Lookout for Trickery and Abuse; Jealous; Tendency to Blame Others; Cold and Humorless
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paranoid – Suspicious; Argumentative; Paranoid; Continually on The
Disorder Gathering 34, 36, 49 Answer Keys A N S W E R K E Y, Disorder Gathering 34 1. Avital Agoraphobia – 2. Ewelina Alcoholism – 3. Martyna Anorexia – 4. Clarissa Bipolar Personality Disorder –. 5. Lysette Bulimia – 6. Kev, Annabelle Co-Dependant Relationship – 7. Archer Cognitive Distortions / all-of-nothing thinking (Splitting) – 8. Josephine Cognitive Distortions / Mental Filter – 9. Mendel Cognitive Distortions / Disqualifying the Positive – 10. Melvira Cognitive Disorder / Labeling and Mislabeling – 11. Liat Cognitive Disorder / Personalization – 12. Noa Cognitive Disorder / Narcissistic Rage – 13. Regev Delusional Disorder – 14. Connor Dependant Relationship – 15. Moira Dissociative Amnesia / Psychogenic Amnesia – (*Jason Bourne character) 16. Eylam Dissociative Fugue / Psychogenic Fugue – 17. Amit Dissociative Identity Disorder / Multiple Personality Disorder – 18. Liam Echolalia – 19. Dax Factitous Disorder – 20. Lorna Neurotic Fear of the Future – 21. Ciaran Ganser Syndrome – 22. Jean-Pierre Korsakoff’s Syndrome – 23. Ivor Neurotic Paranoia – 24. Tucker Persecutory Delusions / Querulant Delusions – 25. Lewis Post-Traumatic Stress Disorder – 26. Abdul Proprioception – 27. Alisa Repressed Memories – 28. Kirk Schizophrenia – 29. Trevor Self-Victimization – 30. Jerome Shame-based Personality – 31. Aimee Stockholm Syndrome – 32. Delphine Taijin kyofusho (Japanese culture-specific syndrome) – 33. Lyndon Tourette’s Syndrome – 34. Adar Social phobias – A N S W E R K E Y, Disorder Gathering 36 Adjustment Disorder – BERKELEY Apotemnophilia -

Comparing the Effectiveness of Mindfulness-Based Cognitive
Special Issue INTERNATIONAL JOURNAL OF HUMANITIES AND May 2016 CULTURAL STUDIES ISSN 2356-5926 Comparing the effectiveness of mindfulness-based cognitive therapy and treatment based on acceptance and commitment therapy on reducing anxiety and depression in women with post-traumatic stress disorder caused by the accident Najaf Abad city of Esfahan Esmaeil Mardani Zadeh MA in Clinical Psychology [email protected] Elham Yousefi MA in Clinical Psychology [email protected] Atousa Khosravi Farsani MA in Psychology Atousa [email protected] Abstract Aims Secondary trauma is a psychological consequence of direct and prolonged contact with a post-traumatic stress disorder person. The purpose of this study was to Compare the effectiveness of mindfulness-based cognitive therapy (MBCT) and treatment based on acceptance and commitment therapy (ACT) on reducing anxiety and depression in women with post-traumatic stress disorder caused by the accident, with controlling the effect of depression, anxiety and stress. Methods: In this quasi-experimental research with pretest-posttest with control group design, 36 women of post-traumatic stress disorder caused by the accident referred to Modarress Psychiatric Hospital of Esfahan, Iran in 2015 were studied. The people who have attained high score on the secondary trauma test were randomly assigned to two experimental groups and one control group. The research instruments were a demographic questionnaire, questionnaire of secondary post-traumatic stress, and questionnaire of depression, anxiety and stress. The interventions (Mindfulness-based cognitive therapy and acceptance commitment therapy) in the experimental group were 8 weeks and once a week, the control group did not receive any training. -

Features of the Application of Art-Therapeutic and Gaming Technology Based on Folk Music in Rehabilitation and Socialization of Children with Health Limitations
Scientific Foundation SPIROSKI, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2020 Aug 15; 8(E):373-381. https://doi.org/10.3889/oamjms.2020.3588 eISSN: 1857-9655 Category: E - Public Health Section: Public Health Education and Training Features of the application of art-therapeutic and gaming technology based on folk music in rehabilitation and socialization of children with health limitations Natalia Ivanovna Anufrieva*, Aleksandr Vlavlenovich Kamenets, Marina Viktorovna Pereverzeva, Marina Gennadievna Kruglova Department of Sociology and Philosophy of Art, Russian State Social University, Wilhelm Pieck Street, 4/1, Moscow 129226, Russia Abstract Edited by: Ksenija Bogoeva-Kostovska AIM: The purpose of the work is to study the specifics and evaluate the effectiveness of the use of art-therapeutic Citation: Anufrieva NI, Kamenets AV, Pereverzeva MV, Kruglova MG. Features of the application of art- and gaming technologies based on musical folklore in the course of rehabilitation of children with health limitations. therapeutic and gaming technology based on folk music in rehabilitation and socialization of children with health MATERIALS AND METHODS: The socialization of such children depends largely on the characteristics of health, limitations. Open Access Maced J Med Sci. 2020 Aug 15; the principles of their training, and the effectiveness of the chosen methods. This justifies the need to analyze the 8(E):373-381. https://doi.org/10.3889/oamjms.2020.3588 *Correspondence: Natalia Ivanovna Anufrieva. practical experience and evaluate the results of efforts of specialists who deal with special children. Department of Sociology and Philosophy of Art, Russian State Social University, Wilhelm Pieck Street, 4/1, Moscow RESULTS: The results of the conducted psychological and pedagogical experiment on the use of art-therapeutic and 129226, Russia. -

DEVELOPMENTAL DELAYS and REGRESSIONS Selective Mutism
CHALLENGING CASE: DEVELOPMENTAL DELAYS AND REGRESSIONS Selective Mutism* CASE Dr. Martin T. Stein Peter’s parents made an appointment with his pe- Selective mutism is an acquired disorder of inter- diatrician because of their increasing concern about personal communication in which a child does not his refusal to speak. After approximately 2 weeks speak in one or more environments where commu- following the start of a new preschool, Peter, 4 years nication typically occurs. These children most often 10 months old, refused to speak to other children or refuse to speak in school and to adults outside the the teacher. During the first week of school, he found home. Some children with selective mutism will not it difficult to separate from his mother or father. He speak to any child; others will use speech with only would cry and cling to them while asking to go a few other children. Parents report normal speech home. This difficult separation experience gradually within the home with at least one parent and some- subsided by the beginning of the third week and times with siblings. The onset of selective mutism is corresponded with the onset of mute behavior. At usually in the preschool or early school age period of home, he spoke only to his mother, with a clear development; often, it is associated with the start of speech pattern and full sentences. He limited his school. responses to his father or two older siblings with Although this disorder is uncommon (1% among body gestures. He appeared to hear well and under- children seen in mental health centers; 0.1% in the stand verbal directions. -

Psichologijos Žodynas Dictionary of Psychology
ANGLŲ–LIETUVIŲ KALBŲ PSICHOLOGIJOS ŽODYNAS ENGLISH–LITHUANIAN DICTIONARY OF PSYCHOLOGY VILNIAUS UNIVERSITETAS Albinas Bagdonas Eglė Rimkutė ANGLŲ–LIETUVIŲ KALBŲ PSICHOLOGIJOS ŽODYNAS Apie 17 000 žodžių ENGLISH–LITHUANIAN DICTIONARY OF PSYCHOLOGY About 17 000 words VILNIAUS UNIVERSITETO LEIDYKLA VILNIUS 2013 UDK 159.9(038) Ba-119 Apsvarstė ir rekomendavo išleisti Vilniaus universiteto Filosofijos fakulteto taryba (2013 m. kovo 6 d.; protokolas Nr. 2) RECENZENTAI: prof. Audronė LINIAUSKAITĖ Klaipėdos universitetas doc. Dalia NASVYTIENĖ Lietuvos edukologijos universitetas TERMINOLOGIJOS KONSULTANTĖ dr. Palmira ZEMLEVIČIŪTĖ REDAKCINĖ KOMISIJA: Albinas BAGDONAS Vida JAKUTIENĖ Birutė POCIŪTĖ Gintautas VALICKAS Žodynas parengtas įgyvendinant Europos socialinio fondo remiamą projektą „Pripažįstamos kvalifikacijos neturinčių psichologų tikslinis perkvalifikavimas pagal Vilniaus universiteto bakalauro ir magistro studijų programas – VUPSIS“ (2011 m. rugsėjo 29 d. sutartis Nr. VP1-2.3.- ŠMM-04-V-02-001/Pars-13700-2068). Pirminis žodyno variantas (1999–2010 m.) rengtas Vilniaus universiteto Specialiosios psichologijos laboratorijos lėšomis. ISBN 978-609-459-226-3 © Albinas Bagdonas, 2013 © Eglė Rimkutė, 2013 © VU Specialiosios psichologijos laboratorija, 2013 © Vilniaus universitetas, 2013 PRATARMĖ Sparčiai plėtojantis globalizacijos proce- atvejus, kai jų vertimas į lietuvių kalbą gali sams, informacinėms technologijoms, ne- kelti sunkumų), tik tam tikroms socialinėms išvengiamai didėja ir anglų kalbos, kaip ir etninėms grupėms būdingų žodžių, slengo, -
WHAT Is Selective Mutism?
WHAT is Selective Mutism? A GUIDE to Helping Parents, Educators and Treatment professionals Understand Selective Mutism as a Social Communication Anxiety Disorder Do you know a child who is mute, barely whispers to few others in school or other social settings, but is able to speak when comfortable such as at home? If so, this child may be suffering from Selective Mutism. “Copyright © [2013] Dr. Elisa Shipon-Blum and Selective Mutism Anxiety Research and Treatment Center, Inc. (SMart Center) – www.selectivemutismcenter.org. 215-887-5748 [email protected] All rights reserved. Selective Mutism is a complex childhood anxiety disorder characterized by a child’s inability to speak and communicate in a socially appropriate manner in select social settings, such as school. These children are able to speak and communicate in settings where they are comfortable, secure and relaxed, such as at home. To meet the diagnostic criteria for Selective Mutism (SM) a child has to be able to speak in at least one setting and be mute in at least one other setting. The typical presentation is the ‘timid’ child who can speak and act socially appropriate with family members, close peers and very familiar relatives, yet is mute or barely whispers to a few others in school or perhaps when addressed in public settings such as restaurants or stores More than 90% of children with Selective Mutism also have social anxiety. This disorder is quite debilitating and painful to the child. Children and adolescents with Selective Mutism have an actual FEAR of speaking and of social interactions where there is an expectation to speak and communicate. -

The Effect of Depersonalization and Derealization Symptoms
THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Thesis Submitted to The College of Arts and Sciences of the UNIVERSITY OF DAYTON In Partial Fulfillment of the Requirements for The Degree of Master of Arts in Psychology By Rhiannon A. Gibbs UNIVERSITY OF DAYTON Dayton, Ohio May 2018 THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Name: Gibbs, Rhiannon A. APPROVED BY: _______________________________________ Julie Walsh-Messinger, Ph.D. Faculty Advisor ______________________________________ Roger R. Reeb, Ph.D. Committee Member ______________________________________ Jackson A. Goodnight, Ph.D. Committee Member Concurrence: _______________________________________ Lee Dixon, Ph.D. Chair, Department of Psychology ii © Copyright by Rhiannon A. Gibbs All rights reserved 2018 ABSTRACT THE EFFECT OF DEPERSONALIZATION AND DEREALIZATION SYMPTOMS ON OLFACTION AND OLFACTORY HEDONICS Name: Gibbs, Rhiannon A. University of Dayton Advisor: Dr. Julie Walsh-Messinger. Depersonalization and derealization symptoms affect sensation, perception, and emotion, producing subjective experiences of unreality and affective numbing (Simeon, 2004). Abnormalities in the amygdala, which is associated with emotional reactions such as anxiety and fear (LeDoux, 1993), have been observed in depersonalization and derealization and other psychiatric disorders, such as anxiety and depression (Sierra & Berrios, 1998). Olfactory deficits have been posited as a potential marker for psychiatric -

1 Serious Emotional Disturbance (SED) Expert Panel
Serious Emotional Disturbance (SED) Expert Panel Meetings Substance Abuse and Mental Health Services Administration (SAMHSA) Center for Behavioral Health Statistics and Quality (CBHSQ) September 8 and November 12, 2014 Summary of Panel Discussions and Recommendations In September and November of 2014, SAMHSA/CBHSQ convened two expert panels to discuss several issues that are relevant to generating national and State estimates of childhood serious emotional disturbance (SED). Childhood SED is defined as the presence of a diagnosable mental, behavioral, or emotional disorder that resulted in functional impairment which substantially interferes with or limits the child's role or functioning in family, school, or community activities (SAMHSA, 1993). The September and November 2014 panels brought together experts with critical knowledge around the history of this federal SED definition as well as clinical and measurement expertise in childhood mental disorders and their associated functional impairments. The goals for the two expert panel meetings were to operationalize the definition of SED for the production of national and state prevalence estimates (Expert Panel 1, September 8, 2014) and discuss instrumentation and measurement issues for estimating national and state prevalence of SED (Expert Panel 2, November 12, 2014). This document provides an overarching summary of these two expert panel discussions and conclusions. More comprehensive summaries of both individual meetings’ discussions and recommendations are found in the appendices to this summary. Appendix A includes a summary of the September meeting and Appendix B includes a summary of the November meeting). The appendices of this document also contain additional information about child, adolescent, and young adult psychiatric diagnostic interviews, functional impairment measures, and shorter mental health measurement tools that may be necessary to predict SED in statistical models. -

Dissociative Experiences in Bipolar Disorder II: Are They Related to Childhood Trauma and Obsessive-Compulsive Symptoms?
Original article Dissociative experiences in bipolar disorder II: Are they related to childhood trauma and obsessive-compulsive symptoms? GUL ERyılmaz1, SERMıN KESEBıR1, IşIl GöğceGöz Gül1, eylem özten1, KayIhan Oğuz KaramustafalIOğlu1 1 Uskudar University Neuropsychiatry Hospital, Psychiatry, Istanbul, Turkey. Received: 12/29/2014 – Accepted: 3/2/2015 DOI: 10.1590/0101-60830000000045 Abstract Objective: The aim of this study is to investigate the presence of dissociative symptoms and whether they are related to childhood trauma and obsessive- -compulsive symptoms in bipolar disorder type II (BD-II). Methods: Thirty-three euthymic patients (HDRS<8, YMRS<5) and 50 healthy subjects were eva- luated by SCID-I and SCID-NP. We excluded all first and second-axis comorbidities. All patients and healthy subjects were examined with the Dissociative Experiences Scale (DES), Childhood Trauma Questionnaire (CTQ-53), and Yale-Brown Obsessive-Compulsive Disorder scale (Y-BOCS). Results: In pairwise comparisons between the BD-II and control groups, the total CTQ, emotional abuse, emotional neglect, DES, and total Y-BOCS scores in the BD-II group were significantly higher than those in the control group (p < 0.05). There were five cases with DES scores over 30 (15.2%) and one case (2%) in the control group. DES was weakly correlated with total CTQ and Y-BOCS in patients diagnosed with BD-II (r = 0.278, p < 0.05 and r = 0.217, p < 0.05, respectively). While there was no correlation between total CTQ and Y-BOCS, the CTQ sexual abuse subscale was found to be related to Y-BOCS (r = 0.330, p < 0.05). -

AVAILABLE from ABSTRACT DOCUMENT RESUME Mental
DOCUMENT RESUME ED 431 981 CG 029 333 TITLE Mental Health in Schools: New Roles for School Nurses. Addressing Barriers to Student Learning. INSTITUTION California Univ., Los Angeles. Center for Mental Health in Schools. SPONS AGENCY Health Resources and Services Administration (DHHS/PHS), Washington, DC. Maternal and Child Health Bureau. PUB DATE 1997-04-00 NOTE 298p. AVAILABLE FROM School Mental Health Project, Center for Mental Health in Schools, Dept. of Psychology, UCLA, 405 Hilgard Ave., Los Angeles, CA 90095-1563; Tel: 310-825-3634; Fax: 310-206-8716; e-mail: [email protected]; Web site: http://smhp.psych.ucla.edu (minimal fee to cover copying, postage and handling). PUB TYPE Guides Classroom Learner (051) Guides Classroom Teacher (052) EDRS PRICE MF01/PC12 Plus Postage. DESCRIPTORS Confidentiality; Due Process; Elementary Secondary Education; *Mental Health; Prevention; *Professional Development; *School Nurses; *Staff Role; Student Development IDENTIFIERS Consent; Screening Programs ABSTRACT This set of three continuing education units is designed to be used as a professional development tool for school nurses. Each unit consists of several sections designed to stand alone. Thus, the total set can be used and taught in a straightforward sequence, or one or more units and sections can be combined into a personalized course. Each section begins with specific objectives and focusing questions to guide reading and review. Interspersed throughout each section is boxed information designed to help the learner think in greater depth about the material. Test questions are provided at the end of each section as an additional study aid. Unit 1, "Placing Mental Health into the Context of Schools and the 21st Century," provides an overview and discusses enhancing health development; addressing barriers to learning; moving toward a comprehensive approach; and responding to students' problems. -
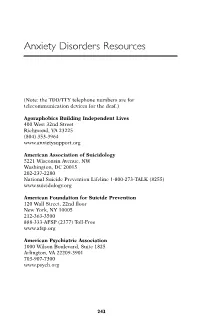
Anxiety Disorders Resources
Anxiety Disorders Resources (Note: the TDD/TTY telephone numbers are for telecommunication devices for the deaf.) Agoraphobics Building Independent Lives 400 West 32nd Street Richmond, VA 23225 (804) 353-3964 www.anxietysupport.org American Association of Suicidology 5221 Wisconsin Avenue, NW Washington, DC 20015 202-237-2280 National Suicide Prevention Lifeline 1-800-273-TALK (8255) www.suicidology.org American Foundation for Suicide Prevention 120 Wall Street, 22nd floor New York, NY 10005 212-363-3500 888-333-AFSP (2377) Toll-Free www.afsp.org American Psychiatric Association 1000 Wilson Boulevard, Suite 1825 Arlington, VA 22209-3901 703-907-7300 www.psych.org 243 244 ANXIETY DISORDERS RESOURCES American Psychological Association 750 First Street, N.E. Washington, DC 20002-4242 800-374-2721 202-336-5500 TDD/TTY: 202-336-6213 www.apa.org Anxiety Disorders Association of America 8730 Georgia Avenue, Suite 600 Silver Spring, MD 20910 240-485-1001 www.adaa.org Association for Behavioral and Cognitive Therapies 305 Seventh Avenue, 16th floor New York, NY 10001 (212) 647-1890 www.aabt.org Doctors Guide www.docguide.com Freedom from Fear 308 Seaview Avenue Staten Island, NY 10305 718-351-1717 www.freedomfromfear.org International Society for Traumatic Stress Studies 60 Revere Drive, Suite 500 Northbrook IL 60062 847-480-9028 www.istss.org MedlinePlus: Health Information www.medlineplus.gov Mental Health America (formerly National Mental Health Association) 2000 N. Beauregard St., 6t floor Alexandria, VA 22311 800-969-6MHA (6642) 703-684-7722 TTY: 800-433-5959 www.mentalhealthamerica.net ANXIETY DISORDERS RESOURCES 245 National Alliance for the Mentally Ill Colonial Place Three 2107 Wilson Boulevard, Suite 300 Arlington, VA 22201-3042 800-950-NAMI (6264) 703-524-7600 TDD: 703-516-7227 www.nami.org National Anxiety Foundation 3135 Custer Drive Lexington, KY 40517-4001 606-272-7166 National Center for Posttraumatic Stress Disorder U.S. -

FF #145 Panic. 3Rd Ed
! FAST FACTS AND CONCEPTS #145 PANIC DISORDER AT THE END-OF-LIFE VJ Periyakoil MD Background Anxiety and fear occur commonly in the dying patient. However, disabling anxiety and/or panic is not a normal aspect of the dying process. Separating “normal” death-related anxiety from pathological panic is an important palliative care skill. Definitions • A panic attack is defined in the DSM-IV as “a discrete period of intense fear or discomfort, in which four (or more) of the following symptoms develop abruptly and reach a peak within 10 minutes: palpitations, pounding heart or accelerated heart rate, sweating, trembling or shaking, sensations of shortness of breath or smothering, feeling of choking, chest pain or discomfort, nausea or abdominal distress, feeling dizzy, unsteady, lightheaded or faint, derealization or depersonalization, fear of losing control or going crazy, fear of dying. • Derealization describes a sensation of feeling estranged or detached from one’s environment. • Depersonalization is an altered and unreal perception of self, one’s feelings and/or situation. Described by one patient as “feeling like you are on the outside looking in”. Diagnosis • A combination of physical symptoms (feeling dizzy, weak, nauseous, unsteady, lightheaded, breathless) and affective symptoms (fear of loss of control) are used to diagnose a panic disorder. • Terminally ill patients may often have many of the physical symptoms listed above as a part of their illness process. Thus the presence of derealization, depersonalization and fear of loss of control are more useful in making the diagnosis of panic disorder in the terminally ill. • A contributing feature to the diagnosis of panic disorder is if a patient develops recurrent symptoms, worries about future ‘attacks’ and alters her/his behavior in anticipation of such attacks.