Posterior Elbow Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Olecranon Bursitis
Olecranon bursitis What is Olecranon How is Olecranon bursitis bursitis? diagnosed? A bursa is a fluid filled sac It is often simple to diagnose Olecranon that stops soft tissues such bursitis without any special test although as tendons, ligaments and your doctor may wish to do blood tests if they skin rubbing on the bone feel it is caused by infection, arthritis or gout. next to them. Bursitis is Occasionally your GP may want to take some inflammation of the bursa of the fluid out of the bursa with a needle to which can be caused by test for infection to ensure they can give the direct impact or by soft correct treatment, although this is unlikely. They tissue tightness over the may also wish to perform an x-ray where there bursa causing repeated has been an injury to ensure there is no small irritation. Olecranon bursitis is an irritation of fracture or bone chip in the elbow. the bursa over the point of the elbow. What is the treatment for What causes Olecranon bursitis? Olecranon bursitis? It is usually caused by repeated injury or Olecranon bursitis will often settle with no irritation to the bursa by activities such as simply treatment other that ensuring the bursa is leaning on the elbow i.e. when reading or protected from whatever caused the irritation in working at a desk which is why it is sometimes the first place. The ‘PRICE’ treatment protocol is called ‘student’s elbow’. It can also be caused by recommended: a one off injury such as falling onto hard ground during sport. -

OES Site Color Scheme 1
Nuisance Problems You will Grow to Love Thomas V Gocke, MS, ATC, PA-C, DFAAPA President & Founder Orthopaedic Educational Services, Inc. Boone, NC [email protected] www.orthoedu.com Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. 2 LEARNING GOALS At the end of this sessions you will be able to: • Recognize nuisance conditions in the Upper Extremity • Recognize nuisance conditions in the Lower Extremity • Recognize common Pediatric Musculoskeletal nuisance problems • Recognize Radiographic changes associates with common MSK nuisance problems • Initiate treatment plans for a variety of MSK nuisance conditions Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response* When does the Inflammatory response occur: • occurs when injury/infection triggers a non-specific immune response • causes proliferation of leukocytes and increase in blood flow secondary to trauma • increased blood flow brings polymorph-nuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to injured tissues *Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137 Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. -

Sports Medicine Examination Outline
Sports Medicine Examination Content I. ROLE OF THE TEAM PHYSICIAN 1% A. Ethics B. Medical-Legal 1. Physician responsibility 2. Physician liability 3. Preparticipation clearance 4. Return to play 5. Waiver of liability C. Administrative Responsibilities II. BASIC SCIENCE OF SPORTS 16% A. Exercise Physiology 1. Training Response/Physical Conditioning a.Aerobic b. Anaerobic c. Resistance d. Flexibility 2. Environmental a. Heat b.Cold c. Altitude d.Recreational diving (scuba) 3. Muscle a. Contraction b. Lactate kinetics c. Delayed onset muscle soreness d. Fiber types 4. Neuroendocrine 5. Respiratory 6. Circulatory 7. Special populations a. Children b. Elderly c. Athletes with chronic disease d. Disabled athletes B. Anatomy 1. Head/Neck a.Bone b. Soft tissue c. Innervation d. Vascular 2. Chest/Abdomen a.Bone b. Soft tissue c. Innervation d. Vascular 3. Back a.Bone b. Soft tissue c. Innervation 1 d. Vascular 4. Shoulder/Upper arm a. Bone b. Soft tissue c. Innervation d. Vascular 5. Elbow/Forearm a. Bone b. Soft tissue c. Innervation d. Vascular 6. Hand/Wrist a. Bone b. Soft tissue c. Innervation d. Vascular 7. Hip/Pelvis/Thigh a. Bone b. Soft tissue c. Innervation d. Vascular 8. Knee a. Bone b. Soft tissue c. Innervation d. Vascular 9. Lower Leg/Foot/Ankle a. Bone b. Soft tissue c. Innervation d. Vascular 10. Immature Skeleton a. Physes b. Apophyses C. Biomechanics 1. Throwing/Overhead activities 2. Swimming 3. Gait/Running 4. Cycling 5. Jumping activities 6. Joint kinematics D. Pharmacology 1. Therapeutic Drugs a. Analgesics b. Antibiotics c. Antidiabetic agents d. Antihypertensives e. -

Download Versus Arthritis
Elbow pain Elbow pain information booklet Contents How does the elbow work? 4 What causes elbow pain and stiffness? 6 Should I see a healthcare professional? 8 What can I do to help myself? 9 How are elbow problems diagnosed? 12 What treatments are there for elbow pain? 14 Specific elbow conditions 18 Glossary 26 Research and new developments 27 Keeping active with elbow pain 28 Where can I find out more? 32 We’re the 10 million people living with arthritis. We’re the carers, researchers, health professionals, friends and parents all united in Talk to us 33 our ambition to ensure that one day, no one will have to live with the pain, fatigue and isolation that arthritis causes. We understand that every day is different. We know that what works for one person may not help someone else. Our information is a collaboration of experiences, research and facts. We aim to give you everything you need to know about your condition, the treatments available and the many options you can try, so you can make the best and most informed choices for your lifestyle. We’re always happy to hear from you whether it’s with feedback on our information, to share your story, or just to find out more about the work of Versus Arthritis. Contact us at [email protected] Words shown are explained in the glossary on p.26. Registered office: Versus Arthritis, Copeman House, St Mary’s Gate, Chesterfield S41 7TD in bold Registered Charity England and Wales No. 207711, Scotland No. SC041156. -

Malignant Olecranon Bursitis in the Setting of Multiple Myeloma Relapse
Case Report Malignant olecranon bursitis in the setting of multiple myeloma relapse Maxwell M Krem, MD, PhD,a Samer Z Al-Quran, MD,b Craig L Silverman, MD,c Vallejo Miller, RN,a and William Tse, MD, FACPa aDivision of Blood and Bone Marrow Transplantation, Department of Medicine, and Departments of bPathology and cRadiation Oncology, at the James Graham Brown Cancer Center, University of Louisville School of Medicine, Louisville, Kentucky ultiple myeloma is the most common Case presentation and summary plasma cell neoplasm, with an esti- A 46-year-old man with a longstanding history mated 24,000 cases occurring annu- of multiple myeloma developed swelling of the Mally. 1 Symptomatic multiple myeloma most com- left elbow that was initially painless in September monly presents with one or more of the cardinal 2016. He had been diagnosed with IgA kappa mul- CRAB phenomena of hypercalcemia, renal dys- tiple myeloma and AL deposition in 2011. Over the function, anemia, or lytic bone lesions.2 Less com- course of his disease, he was treated with the follow- monly, patients may present with plasmacytomas ing sequence of therapies: cyclophosphamide, bort- (focal lesions of malignant plasma cells), which may ezomib, and dexamethasone, followed by melphalan- involve bony or soft tissues.1 conditioned autologous peripheral blood stem cell Plasma cell neoplasms occasionally involve the joints, transplant; lenalidomide and dexamethasone; car lzo- including the elbows, typically as plasmacytomas. e mib and dexamethasone; pomalidomide, bortezomib, elbow is an unusual but reported location of plasma- and dexamethasone; and bortezomib, lenalidomide, cytomas.3,4 A case of multiple myeloma and amyloid dexamethasone, doxorubicin, cyclophosphamide, and light-chain (AL) amyloidosis has been reported, with etoposide, followed by second melphalan-conditioned manifestations including pseudomyopathy, bone mar- autologous peripheral blood stem cell transplant. -

Olecranon Bursitis As Initial Presentation of Gout in Asymptomatic Normouricemic Patients
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector The Egyptian Rheumatologist (2014) 36, 47–50 Egyptian Society for Joint Diseases and Arthritis The Egyptian Rheumatologist www.rheumatology.eg.net www.sciencedirect.com CASE REPORT Olecranon bursitis as initial presentation of gout in asymptomatic normouricemic patients Yasser Emad a,b,*, Yasser Ragab c,d, Nashwa El-Shaarawy e, J.J. Rasker f a Rheumatology and Rehabilitation Department, Faculty of Medicine, Cairo University, Cairo, Egypt b Rheumatology and Rehabilitation Department, Dr. Erfan and Bagedo General Hospital, Jeddah, Saudi Arabia c Radiology Department, Faculty of Medicine, Cairo University, Cairo, Egypt d Radiology Department, Dr. Erfan and Bagedo General Hospital, Jeddah, Saudi Arabia e Rheumatology and Rehabilitation Department, Suez Canal University, Ismailia, Egypt f Rheumatology Department, University of Twente, The Netherlands Received 25 August 2013; accepted 25 August 2013 Available online 4 October 2013 KEYWORDS Abstract Background: Acute bursitis is a less frequent presentation of gout, especially in Olecranon gouty bursitis; normouricemic subjects compared to the typical pattern of acute gouty arthritis. Olecranon bursitis; Aim of the work: The aim of the current case reports is to describe the clinical and the magnetic Gout; resonance imaging features of acute gouty olecranon bursitis as initial presentation of acute gouty MRI features attack. Case report: In this report we describe the clinical and MRI features of three cases presenting with acute gouty olecranon bursitis, in spite of normal serum uric acid and stable renal function. For all cases diagnostic aspiration was carried out to exclude septic bursitis as initial first step of management. -

10 Soft Tissue Injections
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositório Institucional dos Hospitais da Universidade de... Best Practice & Research Clinical Rheumatology Vol. 19, No. 3, pp. 503–527, 2005 doi:10.1016/j.berh.2005.01.003 available online at http://www.sciencedirect.com 10 Soft tissue injections Luı´s P.B.S. Ineˆs MD Rheumatologist Jose´ Anto´nio P. da Silva* MD, PhD Consultant Rheumatologist and Professor of Rheumatology Hospitais da Universidade de Coimbra, 3000-075 Coimbra, Portugal Soft tissue rheumatism includes a wide spectrum of common lesions of the tendons, enthesis, tendon sheaths, bursae, ligaments and fasciae as well as nerve compression syndromes. Studies on the pathogenesis of these lesions do not support a major role for inflammation, thus questioning the rationale for glucocorticoid injections. This chapter reviews current indications for local glucocorticoid injections and available evidence on its efficacy, as well as contra- indications and potential risks. Randomised controlled studies of good methodological quality are rare and there is limited scientific evidence to support the superiority of glucocorticoid injections over alternative treatments. The basic principles of the glucocorticoid injection method are outlined, together with a description of the practical procedure for the more common conditions. Key words: soft tissue rheumatism; treatment; glucocorticoid injection. Periarticular soft tissue rheumatic disorders include a wide spectrum of localised lesions of the tendons, enthesis, tendon sheaths, bursae, ligaments and fasciae as well as nerve compression syndromes. They are extremely common in daily practice and result in significant morbidity and socioeconomic impact. These aspects, together with their tendency to chronicity and recurrence, make the treatment of these conditions an important health care issue. -
Olecranon Bursitis
Physician’s Notes Date: Olecranon Bursitis Mission Statement The mission of ASSH is to advance the science and practice of hand surgery through education, research and advocacy on behalf of patients and practitioners. 6300 North River Road Suite 600 Rosemont, IL 60018-4256 Phone: (847) 384-8300 Fax: (847) 384-1435 E-mail: [email protected] www.handcare.org Diagram for Physician’s use www.handcare.org What is olecranon bursitis? Figure 1. Elbow anatomy with swollen olecranon bursa What are the treatments The olecranon (oh-LEH-cruh-nahn) is the “pointy” bone at for olecranon bursitis? the tip of the elbow. A “bursa”—a small sac of fluid—covers Your doctor likely will ask questions to try to determine if you the tip of this bone, allowing soft tissues such as the skin have a systemic disease that might need to be treated in to slide over the bone. Normally, this sac has only a tiny humerus order to treat the olecranon bursitis. Most people do not. amount of fluid inside of it and is essentially flat. However, sometimes, this area gets irritated and the body makes If you do not have pain, your doctor might recommend extra fluid inside the sac (see Figure 1). This can cause a a resting splint and compression to rest the bursa and big “balloon” to form at the tip of the elbow. help speed recovery. Sometimes elbow pads can help, especially if you find that you are one of those people who What causes olecranon bursitis? radius tend to lean on the tip of the elbow a lot. -

Eval Tx of Shoulder and Elbow Pain in the Adult Patient
Evaluation & Treatment of Disclaimer Shoulder and Elbow Pain in ! I, William T Crowe, have relevant financial relationships to be the Adult Patient© discussed, directly or indirectly, William T. Crowe, RN-C, FNP, referred to or illustrated with or MSN, MBA without recognition within the presentation as follows: –"None Objectives Anatomy ! Review anatomy of the shoulder and elbow ! Bony structures –" Clavicle ! Define elements of subjective history –" Scapula –" Humerus ! Discuss basic exam of the shoulder and elbow ! Discuss current treatment regimens for common problems Anatomy - clavicle Anatomy - Scapula 1 Anatomy Anatomy ! Connective tissue ! Joint capsule –" Ligaments ! Acromioclavicular –" Hyaline cartilage –" Fibrocartilage (labrum) Anatomy Anatomy ! Passive stabilizers ! Active stabilizers (muscles) –" Ligaments –" Glenohumeral (aka Rotator Cuff) –" Joint capsule (supraspinatus, subscapularis, infraspinatus, teres minor) –" Thoracohumeral (pectoralis major, latissimus dorsi) –" Biceps brachii (crosses both shoulder & elbow) Anatomy Anatomy * ! 4 separate joints –" Glenohumeral –" Acromioclavicular –" Sternoclavicular –" Scapulothoracic 2 Anatomy Anatomy ! Planes of motion ! Normal ROM –" Flexion & extension –" 180 degrees flexion –" Internal & external rotation –" 45 - 60 degrees extension –" Abduction/adduction –" 150 degrees abduction –" Circumduction (combination of above) –" 90 degrees external rotation –" 70-90 degrees internal rotation Anatomy Anatomy ! Bony structures ! Connective tissue –" Humerus –" Ligaments (4 –" Radius -
A Patient's Guide to Olecranon Bursitis
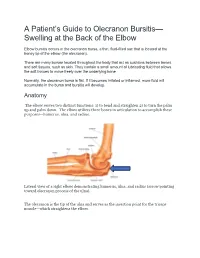
A Patient’s Guide to Olecranon Bursitis— Swelling at the Back of the Elbow Elbow bursitis occurs in the olecranon bursa, a thin, fluid-filled sac that is located at the boney tip of the elbow (the olecranon). There are many bursae located throughout the body that act as cushions between bones and soft tissues, such as skin. They contain a small amount of lubricating fluid that allows the soft tissues to move freely over the underlying bone. Normally, the olecranon bursa is flat. If it becomes irritated or inflamed, more fluid will accumulate in the bursa and bursitis will develop. Anatomy The elbow serves two distinct functions: 1) to bend and straighten 2) to turn the palm up and palm down. The elbow utilizes three bones in articulation to accomplish these purposes—humerus, ulna, and radius. Lateral view of a right elbow demonstrating humerus, ulna, and radius (arrow pointing toward olecranon process of the ulna). The olecranon is the tip of the ulna and serves as the insertion point for the triceps muscle—which straightens the elbow. The triceps muscle inserts into the olecranon process of the elbow and straightens the elbow. The biceps inserts into the radius and bends the elbow. The bones of the elbow are held together by joint capsule, ligaments and tendons. As we age, the strength of both ligaments and bones decrease over time. Ligaments of the elbow viewed from the lateral aspect The Olecranon bursae serves as a buffer between the bony olecranon process and the overlying skin Diagnosis Symptoms Patients who experience olecranon bursitis present with pain, swelling and often bruising over time. -

Triceps Brachii Distal Tendon Reattachment with a Double-Row Technique
n tips & techniques Section Editor: Steven F. Harwin, MD Triceps Brachii Distal Tendon Reattachment With a Double-row Technique Zinon T. Kokkalis, MD; Andreas F. Mavrogenis, MD; Sarantis Spyridonos, MD; Panayiotis J. Papagelopoulos, MD, DSc; Robert W. Weiser, MPAS; Dean G. Sotereanos, MD and less commonly intramus- and those with systemic risk Abstract: Case reports and small series have reported vari- cularly or at the musculoten- factors, improved fixation with able results regarding the treatment of choice for patients with dinous junction.2-24 The most augmentation of the tendon’s triceps brachii tendon ruptures. Early surgical repair has been common mechanism of rupture reattachment may be required recommended for acute complete ruptures of the triceps bra- is indirect trauma, commonly at the surgeon’s discretion. chii distal tendon to prevent late functional disability. However, a fall onto the outstretched Most patients with triceps controversy exists regarding the optimum surgical technique hand that causes a forced ec- brachii tendon ruptures re- of reattachment. In addition, various attachment techniques centric triceps brachii muscle port sudden pain in the pos- have been described, with none shown clinically to be superior. contraction. Rarely, ruptures terior aspect of the elbow. In Therefore, the authors present a technique for triceps brachii distal tendon reattachment following acute complete ruptures may occur following surgical the acute setting, pain dur- and evaluate their results in a series of patients. procedures, such as total elbow ing resisted elbow extension, arthroplasty, and in skeletally swelling, ecchymosis, and immature patients with incom- tenderness to palpation over pletely fused or recently fused the triceps insertion are the riceps brachii injuries oc- injuries and less than 1% of all physes.* usual clinical findings. -

MRI of the Small Joints and Extremities/ Illustrative Cases
1/20/2014 Utility of MR Magnetic Resonance Imaging of In Musculoskeletal Imaging Minor Trauma: January 2014 • Noninvasive • Multiplanar capabilities • No ionizing radiation Mark I. Robbins, M.D. • High sensitivity with Musculoskeletal Radiology excellent spatial Rye, New Hampshire USA resolution=early detection How Does MRI Form A Picture? A Paradox • Fat and Water in the • "Simplicity, simplicity, simplicity! I say, let Human body have an your affairs be as two or three, and not a abundance of hundred or a thousand; instead of a million protons count half a dozen, and keep your accounts on • They resonate in a your thumbnail." HD Thoreau, Walden, random frequency "Where I Lived and What I Lived For" (1854) and orientation • “Simplify, but don’t oversimplify” A. Einstein • For today, we’re going with the Concordian Basics Imaging of All Three Planes The Musculoskeletal System • Radiographs are insensitive to non- displaced fractures, infiltrative processes and marrow edema states • Think of Radiographs as the “sed rate” of imaging 1 1/20/2014 MRI Appearance CT based on Hounsfield Units- Cortical bone & tendons Attenution Coefficient CT defines cortical margins, small avulsions and CT Imaging fracture planes, but some processes are CT occult CT versus MRI OSSEOUS TRAUMA • Insensitive to occult bone marrow edema • CASE STUDIES • Can be useful to define fracture planes, avulsions • Beneficial for incomplete or non-union, due to Shortcut to march05- april 05 191.jpg.lnk “edge enhancement” • Can show small osseous bodies, define osteoid matrices