Download Versus Arthritis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tennis Elbow Handout 503-293-0161
® ® sports INjury medicine department 9250 SW Hall Blvd., Tigard, OR 97223 Tennis Elbow Handout 503-293-0161 WHAT IS IT? Lateral Epicondylitis Tennis elbow, also known as lateral epicondylitis, is one of the most common painful conditions of the elbow. Inflammation and (Tennis Elbow) pain occur on and around the outer bony bump of the elbow where the muscles and tendons attach to the bone. These structures are responsible for lifting your wrist up so this condition can occur with many activities, not just tennis. Humerus (arm bone) Area of pain Tendon lateral epicondyle WHAT ARE THE SYMPTOMS? Most commonly you will have pain & tenderness on the outer side of the elbow and this pain may even travel down the forearm. Often there is pain and/or weakness with gripping and lifting activities. You may also experience difficulty with twisting activities during sports or even opening the lid of a jar. WHY DOES IT HURT? It hurts because you are putting tension on a place where the tissue is weakened, which is usually due to a degenerative process that seems to take a long time for your body to recognize and heal. WHY DO I HAVE IT? This is a common problem and unfortunately we don’t know why some people get this condition and others do not. Surprisingly, it is not at all clear that it comes from overuse or something that you did “wrong”. There is no doubt that if you do have tennis elbow, it will bother you more to do certain things, but that does not necessarily mean it was caused by those activities. -

Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis Page 1 of 19 and Other Musculoskeletal Conditions
Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis Page 1 of 19 and Other Musculoskeletal Conditions Medical Policy An Independent Licensee of the Blue Cross and Blue Shield Association. Title: Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis and Other Musculoskeletal Conditions Professional Institutional Original Effective Date: July 11, 2001 Original Effective Date: July 1, 2005 Revision Date(s): November 5, 2001; Revision Date(s): December 15, 2005; June 14, 2002; June 13, 2003; October 26, 2012; May 7, 2013; January 28, 2004; June 10, 2004; April 15, 2014 April 21, 2005; December 15, 2005; October 26, 2012; May 7, 2013; April 15, 2014 Current Effective Date: April 15, 2014 Current Effective Date: April 15, 2014 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. Treating health care providers are independent contractors and are neither employees nor agents of Blue Cross and Blue Shield of Kansas and are solely responsible for diagnosis, treatment and medical advice. If your patient is covered under a different Blue Cross and Blue Shield plan, please refer to the Medical Policies of that plan. -
Pathologies of the Elbow
Elbow Lateral Epicondylitis (tennis elbow) PathologyPathology 3030 –– 5050 yearsyears oldold RepetitiveRepetitive micro-traumamicro-trauma ChronicChronic teartear inin thethe originorigin ofof thethe extensorextensor carpicarpi radialisradialis brevisbrevis Lateral Epicondylitis (tennis elbow) MechanismMechanism ofof InjuryInjury OveruseOveruse syndromesyndrome causedcaused byby repeatedrepeated forcefulforceful wristwrist andand fingerfinger movementsmovements TennisTennis playersplayers ProlongedProlonged andand rapidrapid activitiesactivities Lateral Epicondylitis (tennis elbow) ClinicalClinical SignsSigns andand SymptomsSymptoms IncreasedIncreased painpain aroundaround laterallateral epicondyleepicondyle TendernessTenderness inin palpationpalpation CETCET TestsTests AROM;AROM; PROMPROM ResistedResisted teststests LidocaineLidocaine Treatment of Tennis Elbow Medial Epicondylitis (golfer’s elbow) PathologyPathology 3030 -- 5050 yearsyears oldold RepetitiveRepetitive micromicro traumatrauma toto commoncommon flexorflexor tendontendon Medial Epicondylitis (golfer’s elbow) MechanismsMechanisms ofof injuryinjury ThrowingThrowing aa baseballbaseball RacquetballRacquetball oror tennistennis SwimmingSwimming backstrokebackstroke HittingHitting aa golfgolf ballball Medial Epicondylitis (golfer’s elbow) ClinicalClinical signssigns andand symptomssymptoms IncreasedIncreased painpain overover medialmedial epicondyleepicondyle TendernessTenderness onon palpationpalpation CFTCFT TestsTests AROM;AROM; PROMPROM ResistedResisted -
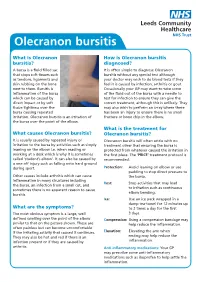
Olecranon Bursitis
Olecranon bursitis What is Olecranon How is Olecranon bursitis bursitis? diagnosed? A bursa is a fluid filled sac It is often simple to diagnose Olecranon that stops soft tissues such bursitis without any special test although as tendons, ligaments and your doctor may wish to do blood tests if they skin rubbing on the bone feel it is caused by infection, arthritis or gout. next to them. Bursitis is Occasionally your GP may want to take some inflammation of the bursa of the fluid out of the bursa with a needle to which can be caused by test for infection to ensure they can give the direct impact or by soft correct treatment, although this is unlikely. They tissue tightness over the may also wish to perform an x-ray where there bursa causing repeated has been an injury to ensure there is no small irritation. Olecranon bursitis is an irritation of fracture or bone chip in the elbow. the bursa over the point of the elbow. What is the treatment for What causes Olecranon bursitis? Olecranon bursitis? It is usually caused by repeated injury or Olecranon bursitis will often settle with no irritation to the bursa by activities such as simply treatment other that ensuring the bursa is leaning on the elbow i.e. when reading or protected from whatever caused the irritation in working at a desk which is why it is sometimes the first place. The ‘PRICE’ treatment protocol is called ‘student’s elbow’. It can also be caused by recommended: a one off injury such as falling onto hard ground during sport. -

OES Site Color Scheme 1
Nuisance Problems You will Grow to Love Thomas V Gocke, MS, ATC, PA-C, DFAAPA President & Founder Orthopaedic Educational Services, Inc. Boone, NC [email protected] www.orthoedu.com Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. 2 LEARNING GOALS At the end of this sessions you will be able to: • Recognize nuisance conditions in the Upper Extremity • Recognize nuisance conditions in the Lower Extremity • Recognize common Pediatric Musculoskeletal nuisance problems • Recognize Radiographic changes associates with common MSK nuisance problems • Initiate treatment plans for a variety of MSK nuisance conditions Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Inflammatory Response* When does the Inflammatory response occur: • occurs when injury/infection triggers a non-specific immune response • causes proliferation of leukocytes and increase in blood flow secondary to trauma • increased blood flow brings polymorph-nuclear leukocytes (which facilitate removal of the injured cells/tissues), macrophages, and plasma proteins to injured tissues *Knight KL, Pain and Pain relief during Cryotherapy: Cryotherapy: Theory, Technique and Physiology, 1st edition, Chattanooga Corporation, Chattanooga, TN 1985, p 127-137 Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. -

A Patient's Guide to Tennis Elbow (Lateral Epicondylitis)
Dr. Edward Kelly www.edwardkellymd.com A Patient’s Guide To Tennis Elbow (Lateral Epicondylitis) WHAT IS TENNIS ELBOW? Tennis elbow is breakdown and degeneration of tendons which attach to the outside (or lateral side) of the elbow. The muscles which work the hand and wrist begin as tendons which attach on a bony prominence on the lateral side of the elbow. This prominence is the lateral epicondyle of the humerus, so tennis elbow is degeneration of the tendons that attach to the lateral epicondyle (and so it is also called “lateral epicondylitis”). The pain can radiate into the forearm and occasionally into the hand. WHAT CAUSES IT? Tennis elbow typically is caused by repetitive gripping and grasping activities or occasionally from direct trauma to the outside of the elbow. Examples include when someone increases the amount of squeezing or gripping they perform, such as trimming the hedge or playing more tennis than usual. Once the tendons get injured it can be difficult to eradicate because those tendons are used every time the hand grips or squeezes. IS IT A SERIOUS CONDITION? Tennis elbow can be a painful and debilitating problem but does not lead to serious problems, like arthritis. However, x-rays or an ultrasound scan may be necessary in some cases to evaluate the elbow joint. An examination by a physician in the office will confirm the diagnosis of lateral epicondylitis. Lateral epicondylitis is the type of condition that will never get so bad that treatment cannot be performed. In many cases, it will resolve over time with non-operative treatments. -

Sports Medicine Examination Outline
Sports Medicine Examination Content I. ROLE OF THE TEAM PHYSICIAN 1% A. Ethics B. Medical-Legal 1. Physician responsibility 2. Physician liability 3. Preparticipation clearance 4. Return to play 5. Waiver of liability C. Administrative Responsibilities II. BASIC SCIENCE OF SPORTS 16% A. Exercise Physiology 1. Training Response/Physical Conditioning a.Aerobic b. Anaerobic c. Resistance d. Flexibility 2. Environmental a. Heat b.Cold c. Altitude d.Recreational diving (scuba) 3. Muscle a. Contraction b. Lactate kinetics c. Delayed onset muscle soreness d. Fiber types 4. Neuroendocrine 5. Respiratory 6. Circulatory 7. Special populations a. Children b. Elderly c. Athletes with chronic disease d. Disabled athletes B. Anatomy 1. Head/Neck a.Bone b. Soft tissue c. Innervation d. Vascular 2. Chest/Abdomen a.Bone b. Soft tissue c. Innervation d. Vascular 3. Back a.Bone b. Soft tissue c. Innervation 1 d. Vascular 4. Shoulder/Upper arm a. Bone b. Soft tissue c. Innervation d. Vascular 5. Elbow/Forearm a. Bone b. Soft tissue c. Innervation d. Vascular 6. Hand/Wrist a. Bone b. Soft tissue c. Innervation d. Vascular 7. Hip/Pelvis/Thigh a. Bone b. Soft tissue c. Innervation d. Vascular 8. Knee a. Bone b. Soft tissue c. Innervation d. Vascular 9. Lower Leg/Foot/Ankle a. Bone b. Soft tissue c. Innervation d. Vascular 10. Immature Skeleton a. Physes b. Apophyses C. Biomechanics 1. Throwing/Overhead activities 2. Swimming 3. Gait/Running 4. Cycling 5. Jumping activities 6. Joint kinematics D. Pharmacology 1. Therapeutic Drugs a. Analgesics b. Antibiotics c. Antidiabetic agents d. Antihypertensives e. -

Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis and Other Musculoskeletal Conditions
Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis Page 1 of 62 and Other Musculoskeletal Conditions Medical Policy An Independent licensee of the Blue Cross Blue Shield Association Title: Extracorporeal Shock Wave Therapy (ESWT) for Plantar Fasciitis and Other Musculoskeletal Conditions Professional Institutional Original Effective Date: July 11, 2001 Original Effective Date: July 1, 2005 Revision Date(s): November 5, 2001; Revision Date(s): December 15, 2005; June 14, 2002; June 13, 2003; October 26, 2012; May 7, 2013; January 28, 2004; June 10, 2004; April 15, 2014; April 14, 2015; April 21, 2005; December 15, 2005; August 4, 2016; January 1, 2017; October 26, 2012; May 7, 2013; August 10, 2017; August 1, 2018; April 15, 2014; April 14, 2015; July 17, 2019, March 11, 2021 August 4, 2016; January 1, 2017; August 10, 2017; August 1, 2018; July 17, 2019, March 11, 2021 Current Effective Date: August 10, 2017 Current Effective Date: August 10, 2017 State and Federal mandates and health plan member contract language, including specific provisions/exclusions, take precedence over Medical Policy and must be considered first in determining eligibility for coverage. To verify a member's benefits, contact Blue Cross and Blue Shield of Kansas Customer Service. The BCBSKS Medical Policies contained herein are for informational purposes and apply only to members who have health insurance through BCBSKS or who are covered by a self-insured group plan administered by BCBSKS. Medical Policy for FEP members is subject to FEP medical policy which may differ from BCBSKS Medical Policy. The medical policies do not constitute medical advice or medical care. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 24, NUMBER 3 - SUMMER 2012 Normal knee anatomy Fig. 1. Anterior knee Inside... pain can be caused by patellofemoral syndrome, • Orthopaedic Components: Quadriceps often called “cyclist’s knee,” muscle What makes a total knee implant? or by patellar tendinitis. • Tennis and Back Pain • Glucosamine and Chondroitin Femur • New Heat Policies - Summer 2012 Patella (kneecap) Imbalances in strength and • Hughston Clinic tone of the lower body Patellar can result in excessive tendon Fibula compressive forces Tibia across the joint. (shinbone) Cycling Overuse Injuries of the Knee Patellofemoral syndrome Compression and shearing across the cartilage of the Quadriceps The economy and higher gas prices are patella can lead to loss of muscle straining wallets and making cycling a more cartilage and the beginning attractive mode of transportation. Health of arthritis. Calf enthusiasts use cycling as a low-impact muscles exercise to improve overall fitness and Patella minimize knee pain. Cities throughout the (kneecap) country are turning old, abandoned railroad Damaged lines into miles of beautiful biking trails and cartilage Femur adding bike lanes to existing roads. In essence, Trochlear cycling is becoming one of the nation’s most groove popular pastimes. Patellar tendinitis Cycling has many health benefits; you Front Quadriceps Cross section of can tone your muscles, improve your view muscle a bent knee cardiovascular fitness, and burn as many as of bent 300 calories an hour during a steady ride. knee People often turn to cycling as a form of Fibula Femur exercise and enjoyment because it is a low- Tibia (thighbone) impact exercise that is easy on the knees. -

Malignant Olecranon Bursitis in the Setting of Multiple Myeloma Relapse
Case Report Malignant olecranon bursitis in the setting of multiple myeloma relapse Maxwell M Krem, MD, PhD,a Samer Z Al-Quran, MD,b Craig L Silverman, MD,c Vallejo Miller, RN,a and William Tse, MD, FACPa aDivision of Blood and Bone Marrow Transplantation, Department of Medicine, and Departments of bPathology and cRadiation Oncology, at the James Graham Brown Cancer Center, University of Louisville School of Medicine, Louisville, Kentucky ultiple myeloma is the most common Case presentation and summary plasma cell neoplasm, with an esti- A 46-year-old man with a longstanding history mated 24,000 cases occurring annu- of multiple myeloma developed swelling of the Mally. 1 Symptomatic multiple myeloma most com- left elbow that was initially painless in September monly presents with one or more of the cardinal 2016. He had been diagnosed with IgA kappa mul- CRAB phenomena of hypercalcemia, renal dys- tiple myeloma and AL deposition in 2011. Over the function, anemia, or lytic bone lesions.2 Less com- course of his disease, he was treated with the follow- monly, patients may present with plasmacytomas ing sequence of therapies: cyclophosphamide, bort- (focal lesions of malignant plasma cells), which may ezomib, and dexamethasone, followed by melphalan- involve bony or soft tissues.1 conditioned autologous peripheral blood stem cell Plasma cell neoplasms occasionally involve the joints, transplant; lenalidomide and dexamethasone; car lzo- including the elbows, typically as plasmacytomas. e mib and dexamethasone; pomalidomide, bortezomib, elbow is an unusual but reported location of plasma- and dexamethasone; and bortezomib, lenalidomide, cytomas.3,4 A case of multiple myeloma and amyloid dexamethasone, doxorubicin, cyclophosphamide, and light-chain (AL) amyloidosis has been reported, with etoposide, followed by second melphalan-conditioned manifestations including pseudomyopathy, bone mar- autologous peripheral blood stem cell transplant. -

Olecranon Bursitis As Initial Presentation of Gout in Asymptomatic Normouricemic Patients
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector The Egyptian Rheumatologist (2014) 36, 47–50 Egyptian Society for Joint Diseases and Arthritis The Egyptian Rheumatologist www.rheumatology.eg.net www.sciencedirect.com CASE REPORT Olecranon bursitis as initial presentation of gout in asymptomatic normouricemic patients Yasser Emad a,b,*, Yasser Ragab c,d, Nashwa El-Shaarawy e, J.J. Rasker f a Rheumatology and Rehabilitation Department, Faculty of Medicine, Cairo University, Cairo, Egypt b Rheumatology and Rehabilitation Department, Dr. Erfan and Bagedo General Hospital, Jeddah, Saudi Arabia c Radiology Department, Faculty of Medicine, Cairo University, Cairo, Egypt d Radiology Department, Dr. Erfan and Bagedo General Hospital, Jeddah, Saudi Arabia e Rheumatology and Rehabilitation Department, Suez Canal University, Ismailia, Egypt f Rheumatology Department, University of Twente, The Netherlands Received 25 August 2013; accepted 25 August 2013 Available online 4 October 2013 KEYWORDS Abstract Background: Acute bursitis is a less frequent presentation of gout, especially in Olecranon gouty bursitis; normouricemic subjects compared to the typical pattern of acute gouty arthritis. Olecranon bursitis; Aim of the work: The aim of the current case reports is to describe the clinical and the magnetic Gout; resonance imaging features of acute gouty olecranon bursitis as initial presentation of acute gouty MRI features attack. Case report: In this report we describe the clinical and MRI features of three cases presenting with acute gouty olecranon bursitis, in spite of normal serum uric acid and stable renal function. For all cases diagnostic aspiration was carried out to exclude septic bursitis as initial first step of management. -

Overuse Injuries in Elite Athletes
ATHLETES: OVERUSE MRI of Overuse INJURIES VERY COMMON Injury in the Elite Athlete • Muscle William B. Morrison, M.D. Associate Professor of • Joints Radiology Thomas Jefferson • Tendon University Hospital Philadelphia, PA USA • Ligament • Bone [email protected] How is this Relevant to My Practice? • High performance athletes get similar injuries as ‘regular’ people… but: – More of them, & at a younger age MUSCLE / SOFT TISSUE – More commonly imaged – Secondary gain involved INJURY • All the cases here are high performance athletes – but most injuries are conventional • Exceptions – Some weird sport-specific patterns of stress and other injuries – Acute injuries as opposed to overuse •Overuse –DOMS Muscle Injury Delayed Onset Muscle • Acute injury Soreness (DOMS) – Tendon – Myotendinous junction • All athletes are susceptible if they – Muscle belly change training regimen • Athletes tend to work out intensely – leads to muscle injury • Rarely imaged (“no pain no gain”) – Weightlifting / aerobic exercise – 24hr later – soreness – Can be severe, even look like a tear 1 Acute Muscle Injury • Direct → muscle belly, esp quadriceps T2 – esp rugby, football • Indirect → myotendinous junction – eccentric contraction – sudden acceleration / DOMS: Lateral gastrocnemius deceleration Finding can be subtle, even with T2 and fat sat Professional football player Acute Injury – T1 Quadriceps hematoma Muscle belly injury Myotendinous Unit Hit with helmet • Myotendinous Junction – ‘weak link’ of normal myotendinous complex T2 – Common place for injury – Most common mechanism: eccentric contraction (muscle lengthens and contracts at the same High time) T1 = blood Gastrocnemius tear: Grade 1 Muscle Strain “V” sign • Ill-defined edema T2 T1 STIR Weishaupt D, JCAT 2001; 25:677 2 Gd Gd can help identify Grade 2 Muscle Strain subtle muscle injury AKA “Partial Tear” STIR Professional baseball player Grade 1 strain Sartorius m.