Ethnic Group Development Plan, Myanmar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kayin State Economy Overview Kayin State Profile: Location: Southern Myanmar Shared Borders: Mandalay Division and Shan State To
Kayin State Economy Overview Kayin State Profile: Location: Southern Myanmar Shared borders: Mandalay Division and Shan State to the north Kayah State and Thailand to the east Bago Division and Mon State to the west Area: 30,383 sq. km Ethnicity: the area was previously known as Karen State, and is mainly inhabited by Karen ethnicities, which are also known as Sagaw Karen, Pwo Karen, Bwe Karen, Paku Karen, and other ethnicities, such as Mon, Shan, Burmese, and Pa-O. Population: 1,504,079 (Myanmar National Population and Housing Census 2014) Population density: 51. 8 persons per square kilometer, which ranks 10th in state population density in Myanmar. For the population in urban and rural areas, the census results showed that for every 100 persons, 78 persons lived in rural areas while 22 persons live in urban areas. The Population Pyramid of Kayin State, 2014 Source: 2014 Myanmar Population and Housing Census Geography Kayin state is formed of 4 districts, 7 townships and 458 villages with 30,383 sq. km area of land. The lowland areas, especially in the west, practice rice farming. In the east, many areas are hilly and covered with forests, with people practicing upland farming. The rocky Dawna Mountain range runs along the length of Kayin state in the east, and the southern and western parts of Kayin state, particularly around Hpa-An area. Air and Rail Transport Kayin State lacks railway infrastructure. The main rail line is only linked to the closest town in Mon State. The airport in Hpa-An and Pha-pun are rarely used for domestic and international flights. -

The Situation in Karen State After the Elections PAPER No
EBO ANALYSIS The Situation in Karen State after the Elections PAPER No. 1 2011 THE SITUATION IN KAREN STATE AFTER THE ELECTIONS EBO Analysis Paper No. 1/2011 For over sixty years the Karens have been fighting the longest civil war in recent history. The struggle, which has seen demands for an autonomous state changed to equal recognition within a federal union, has been bloody and characterized by a number of splits within the movement. While all splinter groups ostensibly split to further ethnic Karen aspirations; recent decisions by some to join the Burmese government’s Border Guard Force (BGF) is seen as an end to such aspirations. Although a number of Karen political parties were formed to contest the November elections, the likelihood of such parties seriously securing appropriate ethnic representation without regime capitulation is doubtful. While some have argued, perhaps correctly, that the only legitimate option was to contest the elections, the closeness of some Karen representatives to the current regime can only prolong the status quo. This papers examines the problems currently affecting Karen State after the 7 November elections. THE BORDER GUARD FORCE Despite original promises of being allowed to recruit a total of 9,000 troops, the actual number of the DKBA (Democratic Karen Buddhist Army) or Karen Border Guard Force has been reduced considerably. In fact, a number of the original offers made to the DKBA have been revoked. At a 7 May 2010 meeting held at Myaing Gyi Ngu, DKBA Chairman U Tha Htoo Kyaw stated that ‘According to the SE Commander, the BGF will retain the DKBA badge.’ In fact the DKBA were given uniforms with SPDC military patches and all Karen flags in DKBA areas were removed and replaced by the national flag. -
Improving the Incomes and Nutrition Outcomes of Rural Poor in Northern Kayin State: Nutritional Causal Analysis
Improving the Incomes and Nutrition Outcomes of Rural Poor in Northern Kayin State: Nutritional Causal Analysis Consortium partners: Consortium of Dutch NGO’s (CDN) World Concern Myanmar (WCM) Cordaid Advisory partner: SNV Local implementing partners: Taungoo Thandawn Bwe Moh Bwa Karen Baptist Association (BMB) Taungoo Kehko Kehbah Karen Baptist Association (KKBA) Taungoo Paku Karen Baptist (PKBA) Karuna Myanmar Social Services (KMSS) NCA Consultants: Mekong Economics Myanmar October 2016 – January 2017 P a g e | 1 TABLE OF CONTENTS Table of Figures ........................................................................................................................... 2 List of Tables ................................................................................................................................ 3 List of Acronyms .......................................................................................................................... 3 Executive Summary ...................................................................................................................... 4 1 Methodology ........................................................................................................................ 7 Nutrition Causal Analysis (NCA) .......................................................................................................... 7 NCA in Kayin ........................................................................................................................................ 8 2 Context ............................................................................................................................. -

OPERATIONAL BRIEF Southeast Myanmar
OPERATIONAL BRIEF Southeast Myanmar OVERVIEW Southeast Myanmar is composed of Kayah, Kayin and Mon states, and Tanintharyi Region, bordering Thailand to the east and south, Bago Region and the Andaman Sea to the west and Shan State to the north. With a population of approximately 5.3 million (2014 national census) this area is inhabited by Mon, Bamar, Kayin, Rakhine, Chin, Kachin, Pa-O, Shan, Salone and Malay ethnic groups. At Myanmar’s independence in 1948, discord between the Government and ethnic groups over federalism instigated armed conflicts between the Myanmar security forces and ethnic armed groups, including New Mon State Party (NMSP), Karen National Union (KNU), Democratic Karen Benevolent Army (DKBA) and Karenni National Progressive Party (KNPP). Routine clashes in rural areas of the southeastern region resulted in decades of instability and the protracted displacement of 110,000 people in ten refugee camps in Thailand as well as 12,400 people in six internally displaced persons (IDP) camps along the Thai- Myanmar border in Shan and Kayin states. In 2015, the ethnic armed groups KNU and DKBA signed the Nationwide Ceasefire Agreement (NCA), marking a historic first step towards restoration of peace in the area. As of May 2017, a total of 2,370 refugees and 9,386 IDPs verified by UNHCR had returned for permanent stay in the area. The total verified refugee population stands at 100,388 people. PARTNERSHIPS Since 2008, WFP has been providing food and nutrition Government Ministries support to people living with HIV (PLHIV) and TB clients in Southeast Myanmar through IOM. To expand its Ministry of Planning and Finance scope, WFP opened its Mawlamyine field office in June Ministry of Social Welfare, Relief and Resettlement Ministry of Education 2014 to support the most vulnerable populations from conflict-affected areas and to assist future returnees Ministry of Health and Sports from Thai border camps with unconditional food/cash Ministry of Agriculture, Livestock and Irrigation transfers during the transitioning period. -

PDF 892.20Kb
Working paper Building on what’s there Insights on social protection and public goods provision from central-east Myanmar Gerard McCarthy September 2016 When citing this paper, please use the title and the following reference number: S-53308-MYA-2 Gerard McCarthy Building on What’s There: Insights on social assistance, public goods and taxation from central-east Myanmar Section 1: Introduction After decades of military rule in Myanmar, the political and economic transitions that are now underway are already impacting on the provision of social protection services and public goods at the local level.1 The progress made towards reaching cease-fires with armed groups around the country has allowed for expansion of the Myanmar government apparatus and services in some of these areas. Government expenditures on health, education, and to a lesser extent social welfare and rural development have increased substantially since 20092. Specific groups of individuals such as pregnant mothers and the elderly are now receiving assistance including direct cash transfers from state ministries, largely financed by international donors. 3 In addition, a National Social Protection Strategy is now in place. Moreover the newly elected National League for Democracy (NLD) government are planning to expand state- provided welfare, social services and other public goods.4 These are all positive developments. Often ignored in attempts to support livelihoods through state-mediated welfare initiatives, however, is Myanmar’s extensive economy of non-state welfare and public goods provisioning. Developed over decades of military rule, often with the direct encouragement of the regime itself, there are 100,000s of localized mechanisms of risk-sharing and social protection operating across Myanmar.5 However, little is known about the relative importance of these networks for households when compared to government support; the extent of the fiscal burden that falls on households; and households’ opinions on this system of care. -
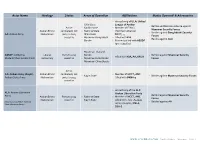
ACLED – Myanmar Conflict Update – Table 1
Actor Name Ideology Status Areas of Operation Affiliations Modus Operandi & Adversaries - Armed wing of ULA: United - Chin State League of Arakan - Battles and Remote violence against Active - Kachin State - Member of FPNCC Myanmar Security Forces Arakan Ethnic combatant; not - Rakhine State (Northern Alliance) - Battles against Bangladeshi Security AA: Arakan Army Nationalism party to 2015 - Shan State - NCCT, , , Forces ceasefire - Myanmar-Bangladesh - Allied with KIA - Battles against ALA Border - Formerly allied with ABSDF (pre-ceasefire) - Myanmar-Thailand ABSDF: All Burma Liberal Party to 2015 Border - Battled against Myanmar Security - Allied with KIA, AA, KNLA Students’ Democratic Front democracy ceasefire - Myanmar-India Border Forces - Myanmar-China Border Active AA: Arakan Army (Kayin): Arakan Ethnic combatant; not - Member of NCCT, ANC - Kayin State - Battles against Myanmar Security Forces Arakan State Army Nationalism party to 2015 - Allied with DKBA-5 ceasefire - Armed wing of the ALP: ALA: Arakan Liberation Arakan Liberation Party - Battled against Myanmar Security Army Arakan Ethnic Party to 2015 - Rakhine State - Member of NCCT, ANC Forces Nationalism ceasefire - Kayin State - Allied with AA: Arakan (Also known as RSLP: Rakhine - Battled against AA State Liberation Party) Army (Kayin), KNLA, SSA-S WWW.ACLEDDATA.COM | Conflict Update – Myanmar – Table 1 Rohingya Ethnic Active ARSA: Arakan Rohingya - Rakhine State Nationalism; combatant; not Salvation Army - Myanmar-Bangladesh UNKNOWN - Battles against Myanmar Security -

Kayin State - Myanmar
Myanmar Information Management Unit KAYIN STATE - MYANMAR 96° E 98° E Demoso Shadaw NAY PYI TAW SHAN Hpruso India China Leik Tho Myanmar Yedashe Bawlakhe Laos Ywarthit Kaytumati Thandaunggyi KAYAH Thailand Taungoo Baw Ga Li Hpasawng Oktwin Htantabin Thandaunggyi Mese Township Phyu Zigon Kyaukkyi Gyobingauk Penwegon BAGO Okpho Kyauktaga Hpapun Minhla 18° N Nyaunglebin Hpapun 18° N Shwegyin Township Pyuntasa Madauk Letpadan Daik-U Thayarwady THAILAND Thonse Okekan Waw Shan Ywar Thit Ahpyauk Bago Kamarmaung Taikkyi Kyaikto Hlaingbwe Thanatpin Bilin Township YANGON Hlaingbwe Hmawbi Kawa Nyaungdon Hlegu Htantabin Paingkyon Shwepyithar Htaukkyant Thaton Kayan Hpa-An Hlaingtharya KAYIN Myawaddy Thongwa Hpa-An Township Maubin Yangon City MON Township Myawaddy Twantay Thanlyin Tadar Paung Kyauktan Kyondoe Kawhmu Kawkareik Mawlamyine Kyaiklat Kungyangon Kawkareik Township Dedaye Kyaikmaraw Pyapon Chaungzon Waw Lay Myaing (Waw Lay) Mudon AYEYARWADY Gulf Of Martaban Su Ka Li Kyaikkhami Kyainseikgyi Thanbyuzayat 16° N Kyaikdon 16° N Kyainseikgyi Township Lamaing Hpayarthonesu Ye Kilometers Copyright © Myanmar Information Management Unit 2016. May be used free of charge with attribution. 0 15 30 60 96° E Khawzar98° E Legend Map ID: MIMU182v05 Data Sources: MIMU State/Region Capital Railway River/Water Body Elevation (Meter) 1,501 - 2,000 Base Map - MIMU Creation Date: 16 August 2016.A3 Non-Perennial 0 - 250 Main Town Stream and Shore Line 2,001 - 2,500 Projection/Datum: Geographic/WGS84 Boundaries - WFP/MIMU Township Boundary Perennial 251 - 500 2,501 - 3,000 Other Town Elevation: SRTM District Boundary 501 - 750 3,001 - 4,000 Airports Place names - Ministry of Home Affair Email - [email protected] State/Region Boundary 751 - 1,000 4,001 - 5,000 Road (GAD) translated by MIMU www.themimu.info International Boundary 1,001 - 1,500 5,001 - 7,002 Disclaimer: The names shown and the boundaries used on this map do not imply official endorsement or acceptance by the United Nations.. -

Kayah State Profile Updated: June 20141
UNHCR SOUTH-EAST MYANMAR INFORMATION MANAGEMENT UNIT KAYAH STATE PROFILE UPDATED: JUNE 20141 State Kayah Flag Previous Name Karenni State Capital Loikaw NumBer of Districts 2 NumBer of Townships 7 Ward and VillaGe 105 Tracts Total population (2012 360,379 Est.) IDPs 34,600 Refugees 11,662 Area 4,510 sq. miles / 11,670 sq. kms North: Shan State East: Mae HonG Son province, Border Thailand West and South: Kayin state o o Latitude 18 30'N and 19 55'N Longitude 94o 40'E and 97o 93'E Map: Myanmar Information Management Unit Kayah, Kayin, Kayan, Kayaw, Bamar, Ethnicities Shan, Pa-O, Background Located in eastern Myanmar, Kayah State is bounded by Shan State to the north, Kayin State to the south and west, and Thailand’s Mae Hon SonG to the East. Previously Known as Karenni State, the territory is inhaBited primarily by the Karenni ethnic Group, also Known as the Red Karen. As a sub-group of the Karen people, the Karenni have maintained a close historical relationship with Kayin State. Low intensity conflict has recurred in Kayah State since the 1947 Constitution established an independent Burma, which included then-Karenni State within the Union of Burma, despite assertions from Karenni representatives that their nation souGht self- determination as independent and sovereiGn. Much of the current displacement from Kayah State dates BacK to the mid-1990s, and the armed clashes before and after the failed 1995 ceasefire Between the Tatmadaw and the Karenni National Progressive Party (KNPP). Counter-insurGency strateGies employed to varying deGrees by both sides have historically exacerbated the forced displacement resultinG from direct armed conflict Between the Government and the non-state actors 1 Disclaimer: These state profiles were printed in June 2014, and will be updated periodically by the UNHCR South-East Myanmar Information Management Unit to reflect new developments, additions and corrections. -

Country Paper (Myanmar Today)
Myanmar Today I. Introduction Myanmar, officially known as the Republic of the Union of Myanmar is geographically situated in the south-east Asia region. As the largest country on mainland South-East Asia, it shares borders with China, Laos and Thailand in the east and Bangladesh, India in the west, the Bay of Bengal to the South-West with the Andaman Sea. The country covers an area of 261228 sq miles (677000 square kilometers), ranging 582 miles (936 kilometers) from east to west and 1275 miles (2051 kilometers) from north to south. Myanmar is made up of over one hundred national races, of which the main national races are Kachin, Kayah, Kayan, Chin, Burma, Mon, Rakhine and Shan. The Population of the country is over 60 million. Urban and Rural ratio in Myanmar is 30:70. II. Background Myanmar has emerged as a new nation in line with its Constitution which adopted on 29 May 2008, and so it is on the right track of transition into new era and new system. The process of building a modern and developed nation has posted milestones of success, and is also moving forward at an accelerating pace. As a developing country, Myanmar has been practicing market economy system to raise socio-economic status of its people. And in building a modern and industrialized nation in accord with the Constitution, Myanmar makes strenuous efforts for proper evolution of market economy through agricultural development in combination with all-round development of other sectors. At the same time Myanmar exercising independent, active and non-aligned foreign policy and upholding the principles of peaceful coexistence among nations, tries its best to catch up with not only regionalization but also globalization process. -

Rapid Urban Diagnostic Report
THE REPUBLIC OF THE UNION OF MYANMAR RAPID URBAN DIAGNOSTIC REPORT Prepared for Department of Urban and Housing Development, Ministry of Construction With technical assistance from UN Habitat RAPID URBAN DIAGNOSTIC REPORT MYANMAR TABLE OF CONTENTS A. CONTEXT AND BACKGROUND OF RAPID URBAN DIAGNOSTIC REPORT MYANMAR P. 4 A.I EXECUTIVE SUMMARY P. 4 A.II GENERAL BACKGROUND P. 5 A.III BACKGROUND OF RAPID URBAN DIAGNOSTIC P. 5 A.IV PURPOSE OF RAPID URBAN DIAGNOSTIC REPORT MYANMAR P. 6 B. RAPID URBAN DIAGNOSTIC REPORT MYANMAR P. 7 B.I URBANIZATION P. 7 B.I.1 CURRENT LEVEL OF URBANIZATION P. 7 B.I.2 URBANIZATION IN MYANMAR IN REGIONAL PERSPECTIVE P. 9 B.I.3 DRIVERS AND TRENDS OF URBANIZATION P. 11 B.I.3.1 DRIVERS OF URBANIZATION P. 11 B.I.3.2 PROJECTION OF URBANIZATION P. 12 B.I.3.3 SPATIAL DIMENSION OF URBANIZATION IN MYANMAR P. 13 B.II MYANMAR’S SYSTEM OF URBAN CENTERS AND GROWTH CORRIDORS P. 14 B.III URBAN GOVERNANCE IN TOWNSHIPS/SECONDARY CITIES P. 19 B.III.1 CONSTITUTIONAL FRAMEWORK P. 19 B.III.2 ADMINISTRATIVE ORGANIZATION AT THE TOWNSHIP LEVEL P. 20 B.III.2.1 THE TOWNSHIP ADMINISTRATOR AS CENTRAL ACTOR AT TOWNSHIP LEVEL P. 20 B.III.2.2 THE TOWNSHIP COMMITTEES P. 20 B.III.2.3 A SPECIAL CASE: THE TOWNSHIP MUNICIPAL AFFAIRS COMMITTEE AND THE DEPARTMENT OF MUNICIPAL AFFAIRS (DEVELOPMENT AFFAIRS ORGANIZATION) P. 22 B.III.2.3.1 ORIGINS OF DMA P. 22 B.III.2.3.2 DMA’S FISCAL POSITION P. -

Maximizing Transport Benefits Through Community Engagement Project
Technical Assistance Consultant’s Report Project Number: 46422-002 December 2015 Republic of the Union of Myanmar: Maximizing Transport Benefits through Community Engagement (Financed by the Technical Assistance Special Fund) Prepared by the Mekong Economics, Ltd. and the Adventist Development Relief Agency Myanmar For the Ministry of Construction and the Asian Development Bank This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. Kayin and Mon State Context, Stakeholders and Engagement Kayin and Mon States Context, Stakeholders and Engagement Guidance for the Asian Development Bank (ADB) and implementing partners December 2015 Mekong Economics / ADRA Myanmar 1 Kayin and Mon State Context, Stakeholders and Engagement Table of Contents Acronyms ....................................................................................... 3 Introduction .................................................................................... 6 Terminology ......................................................................................... 8 A note on place names and administrative demarcation .................................... 8 Ethnographic overview ............................................................................ 9 Overview of Conflict and peace in Kayin and Mon States ........................... 10 The Peace Process since 2011 .................................................................. 12 Humanitarian impacts: -

IDP 2011 Eng Cover Master
Thailand Burma Border Consortium 2011 DISPLACEMENT AND POVERTY IN SOUTH EAST BURMA / MYANMAR With Field Assessments and Situation Updates by: Committee for Internally Displaced Karen People Karen Offi ce of Relief and Development Karenni Social Welfare and Development Centre Mon Relief and Development Committee Shan Relief and Development Committee Thailand Burma Border Consortium 12/5 Convent Road, Bangrak, Bangkok, 10500, Thailand [email protected] www.tbbc.org Front cover photo : Post-election displacement, Hpapun Township, 2011, CIDKP CONTENTS EXECUTIVE SUMMARY ................................................................................................................. 1 1. METHODOLOGY ...................................................................................................................... 5 1.1 Design, Data Collection and Analysis ................................................................................ 6 1.2 Household Survey Sample ................................................................................................ 8 1.3 Limitations ......................................................................................................................... 9 2. TRENDS IN SOUTH EAST BURMA / MYANMAR* .................................................................. 11 2.1 Protracted Confl ict ............................................................................................................. 12 2.2 Resource Curse and Development ..................................................................................