Dblrocuroniuminj.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Study of Different Doses of Rocuronium Bromide For
MedDocs Publishers Annals of Anesthesia and Pain Medicine Open Access | Research Article Comparative study of different doses of rocuronium bromide for endotracheal intubation Nidhi V Sardhara1*; Sonal A Shah2; Dhaval P Pipaliya3; Shivansh Gupta3 1SVP hospital, 13th floor, Room no 13125, Near Ellis bridge, Ahmedabad, Gujarat-380006 2Assistant Professor, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India 3First year Resident, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India *Corresponding Author(s): Nidhi V Sardhara Abstract SVP hospital, 13th floor, Room no 13125, Near Ellis Background: Endotracheal intubation is one of such bridge, Ahmedabad, Gujarat-380006 development without which general anesthesia cannot be Tel: +91-9428-44-7878, Fax: 7926-57-8452 considered safe for any major surgery particularly head and Email: [email protected] neck, thoracic and abdominal surgeries. Ever since the ad- vent of anesthesia, anesthesiologists have been in search of an ideal muscle relaxants which can provide ideal intu- bating conditions in ultrashort duration with minimal side effects. Rocuronium bromide provides fast onset of action, Received: Mar 11, 2020 an intermediate duration of action and rapid recovery, good Accepted: Apr 24, 2020 to excellent intubating conditions at doses having minimal Published Online: Apr 30, 2020 or no haemodynamic changes. Present study is to compare the effect of different doses (0.6 mg/kg, 0.9 mg/kg, 1.2 mg/ Journal: Annals of Anesthesia and Pain Medicine kg) of Rocuronium bromide for endotracheal intubation at Publisher: MedDocs Publishers LLC 60 seconds. Online edition: http://meddocsonline.org/ Material and methods: This study was carried out by Copyright: © Sardhara NV (2020). -

Vecuronium Bromide As Control
A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL. Dissertation submitted In partial fulfillment for the award of M.D DEGREE EXAMINATION M.D. ANAESTHESIOLOGY & CRITICAL CARE BRANCH X GOVT KILPAUK MEDICAL COLLEGE AND HOSPITAL SUBMITTED TO THE TAMILNADU DR. MGR MEDICAL UNIVERSITY CHENNAI APRIL – 2011 1 DECLARATION I, Dr. D.Shunmuga Priya, solemnly declare that the dissertation, “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” is a bonafide work done by me in the Department of Anaesthesiology and Critical Care, Government Kilpauk, Medical College, Chennai under the able guidance of Prof. Dr. P.S. Shanmugam, MD., DA., Professor and HOD, Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai. Place : Chennai Date : (Dr. D.SHUNMUGA PRIYA) 5 CERTIFICATE This is to certify that this dissertation titled “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” has been prepared by Dr. D.SHUNMUGA PRIYA under my supervision in the Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai during the academic period 2008-2011 and is being submitted to the Tamil Nadu Dr. M.G.R. Medical University, Chennai in partial fulfillment of the University regulation for the award of the Degree of Doctor of Medicine (MD Anaesthesiology and Critical Care) and her dissertation is a bonafide work. Prof..Dr. V.Kanagasabai, M.D Prof. Dr. P.S.Shanmugam, M.D., D.A. DEAN Professor & HOD, Government Kilpauk Medical College Department of Anaesthesiology and & Hospital, Critical Care, Chennai. -
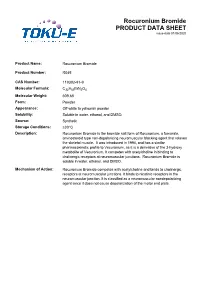
Rocuronium Bromide PRODUCT DATA SHEET Issue Date 01/06/2020
Rocuronium Bromide PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Rocuronium Bromide Product Number: R045 CAS Number: 119302-91-9 Molecular Formula: C32H53BrN2O4 Molecular Weight: 609.68 Form: Powder Appearance: Off-white to yellowish powder Solubility: Soluble in water, ethanol, and DMSO. Source: Synthetic Storage Conditions: ≤30°C Description: Rocuronium Bromide is the bromide salt form of Rocuronium, a fumarate, aminosteroid type non-depolarizing neuromuscular blocking agent that relaxes the skeletal muscle. It was introduced in 1994, and has a similar pharmacokinetic profile to Vecuronium, as it is a derivative of the 3-hydroxy metabolite of Vecuronium. It competes with acetylcholine in binding to cholinergic receptors at neuromuscular junctions. Rocuronium Bromide is soluble in water, ethanol, and DMSO. Mechanism of Action: Rocuronium Bromide competes with acetylcholine and binds to cholinergic receptors at neuromuscular junctions. It binds to nicotinic receptors in the neuromuscular junction. It is classified as a neuromuscular nondepolarizing agent since it does not cause depolarization of the motor end plate. References: Anzenbacherova et al (2015) Interaction of Rocuronium with human liver cytochromes P450. J. Pharmacol. Sci. 127(2):190-195 PMID 25727956 Cembala TM, Sherwin JD, Tidmarsh MD, Appadu BL and Lambert DG (1998) Interaction of neuromuscular blocking drugs with recombinant human m1-m5 muscarinic receptors expressed in Chinese hamster ovary cells. B. J. Pharmacol. 125(5):1088-1094 PMID 9846649 Koksal PM and Gürbüzel M(2015) Analysis of genotoxic activity of ketamine and Rocuronium Bromide using the somatic mutation and recombination test in Drosophila melanogaster. Environ Toxicol Pharmacol. 39(2):628-634 PMID 25682000 Sauer et al (2017) Rocuronium is more hepatotoxic than succinylcholine in vitro. -

COMPARISON of ROCURONIUM BROMIDE and SUCCINYLCHOLINE CHLORIDE for USE DURING RAPID SEQUENCE INTUBATION in ADULTS Ch
DOI: 10.18410/jebmh/2015/672 ORIGINAL ARTICLE COMPARISON OF ROCURONIUM BROMIDE AND SUCCINYLCHOLINE CHLORIDE FOR USE DURING RAPID SEQUENCE INTUBATION IN ADULTS Ch. Penchalaiah1, N. Jagadeesh Babu2, T. Kumar3 HOW TO CITE THIS ARTICLE: Ch. Penchalaiah, N. Jagadeesh Babu, T. Kumar. ”Comparison of Rocuronium Bromide and Succinylcholine Chloride for Use during Rapid Sequence Intubation in Adults”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 32, August 10, 2015; Page: 4796-4806, DOI: 10.18410/jebmh/2015/672 ABSTRACT: BACKGROUND AND OBJECTIVE: The goal of rapid sequence intubation is to secure the patients airway smoothly and quickly, minimizing the chances of regurgitation and aspiration of gastric contents. Traditionally succinylcholine chloride has been the neuromuscular blocking drug of choice for use in rapid sequence intubation because of its rapid onset of action and profound relaxation. Succinylcholine chloride remains unsurpassed in providing ideal intubating conditions. However the use of succinylcholine chloride is associated with many side effects like muscle pain, bradycardia, hyperkalaemia and rise in intragastric and intraocular pressure. Rocuronium bromide is the only drug currently available which has the rapidity of onset of action like succinylcholine chloride. Hence the present study was undertaken to compare rocuronium bromide with succinylcholine chloride for use during rapid sequence intubation in adult patients. METHODOLOGY: The study population consisted of 90 patients aged between 18-60 years posted for various elective surgeries requiring general anaesthesia. Study population was randomly divided into 3 groups with 30 patients in each sub group. 1. Group I: Intubated with 1 mg kg-1 of succinylcholine chloride (n=30). -

INTUBATING CONDITIONS and INJECTION PAIN - Cisatracurium Or Rocuronium Versus Rocuronium-Cisatracurium Combination
INTUBATING CONDITIONS AND INJECTION PAIN - Cisatracurium or Rocuronium versus Rocuronium-Cisatracurium Combination - * * AHED ZEIDAN ,NAZIH NAHLE , ** *** HILAL MAALIKI AND ANIS BARAKA Summary The present report evaluates the incidence of pain on intravenous injection and the condition of tracheal intubation at one minute following the administration of cisatracurium or rocuronium versus rocuronium- cisatracurium combination. We studied 60 patients, ASA 1, aged 18-60 years, undergoing elective surgical procedures. The patients were randomly assigned to 3 groups who received intravenously either 0.15 mg/kg cisatracurium [2ED95], 0,6 mg rocuronium [2ED95] or a combination of 0.075 mg/kg cisatracurium [1ED95], plus 0.3 mg rocuronium [1ED95]. In the awake patients, the pain on injection of muscle relaxant was assessed on a four point scale (none, mild, moderate, severe). Administration of the relaxant was followed by 1-2 mg/kg of lidocaine and 2 mg/kg propofol. Oro- tracheal intubation was performed 60 seconds following the administration of the relaxant. The intubating conditions were assessed and rated as excellent, good, fair or poor. * MD, Staff Anaesthesiologist, Department of Anaesthesiology, Sahel General Hospital, Beirut, Lebanon. **MD Staff Anaesthesiologist, Department of Anaesthesiology, Beirut Governmental University Hospital, Beirut, Lebanon. *** MD, FRCA, Professor and and Chairman, Department of Anesthesiology, American University of Beirut Medical Center, Beirut, Lebanon. Corresponding Author: Ahed Zeidan, Department of Anaesthesiology, Sahel General Hospital, Airport Ave. P.O. Box: 99/25-Ghobeiry, Beirut-Lebanon. Phone: 961-1-858333. Fax: 961-1-840146, E-mail: [email protected]. 879 M.E.J. ANESTH 18 (5), 2006 880 AHED ZEIDAN ET. AL The administration of 2ED95 cisatracurium resulted in poor intubating conditions at 60s, without pain on injection. -

Reversal of Neuromuscular Bl.Pdf
JosephJoseph F.F. Answine,Answine, MDMD Staff Anesthesiologist Pinnacle Health Hospitals Harrisburg, PA Clinical Associate Professor of Anesthesiology Pennsylvania State University Hospital ReversalReversal ofof NeuromuscularNeuromuscular BlockadeBlockade DefiniDefinitionstions z ED95 - dose required to produce 95% suppression of the first twitch response. z 2xED95 – the ED95 multiplied by 2 / commonly used as the standard intubating dose for a NMBA. z T1 and T4 – first and fourth twitch heights (usually given as a % of the original twitch height). z Onset Time – end of injection of the NMBA to 95% T1 suppression. z Recovery Time – time from induction to 25% recovery of T1 (NMBAs are readily reversed with acetylcholinesterase inhibitors at this point). z Recovery Index – time from 25% to 75% T1. PharmacokineticsPharmacokinetics andand PharmacodynamicsPharmacodynamics z What is Pharmacokinetics? z The process by which a drug is absorbed, distributed, metabolized and eliminated by the body. z What is Pharmacodynamics? z The study of the action or effects of a drug on living organisms. Or, it is the study of the biochemical and physiological effects of drugs. For example; rocuronium reversibly binds to the post synaptic endplate, thereby, inhibiting the binding of acetylcholine. StructuralStructural ClassesClasses ofof NondepolarizingNondepolarizing RelaxantsRelaxants z Steroids: rocuronium bromide, vecuronium bromide, pancuronium bromide, pipecuronium bromide. z Benzylisoquinoliniums: atracurium besylate, mivacurium chloride, doxacurium chloride, cisatracurium besylate z Isoquinolones: curare, metocurine OnsetOnset ofof paralysisparalysis isis affectedaffected by:by: z Dose (relative to ED95) z Potency (number of molecules) z KEO (plasma equilibrium constant - chemistry/blood flow) — determined by factors that modify access to the neuromuscular junction such as cardiac output, distance of the muscle from the heart, and muscle blood flow (pharmacokinetic variables). -
Pdf Medication Assisted Induction Guidelines Final 05072019
Medication Assisted Induction (MAI) Regional Guidelines 2019 Edition Effective June 1, 2019 Lord Fairfax EMS Council, Inc. 180-1 Prosperity Drive Winchester, Virginia 22602 Phone 540-665-0014 Fax 540-722-0094 www.lfems.vaems.org © 2019 LFEMS Medication Assisted Induction (MAI) Guidelines – Revised 05/07/2019 1 LORD FAIRFAX EMERGENCY MEDICAL SERVICES COUNCIL, INC. MEDICATION ASSISTED INDUCTION (MAI) REGIONAL GUIDELINES TABLE OF CONTENTS MEDICATION ASSISTED INDUCTION (MAI) REGIONAL GUIDELINES REVISION HISTORY ........................................................................................................ 3 PREFACE .........................................................................................................................4 MAI AUTHORIZATION TO PRACTICE ............................................................................. 5 REGIONAL PROVIDER GUIDELINES ............................................................................. 6 FENTANYL (SUBLIMAZE®) ........................................................................................... 12 KETAMINE (KETALAR®) ............................................................................................... 13 MIDAZOLAM (VERSED®) .............................................................................................. 14 ROCURONIUM BROMIDE (ZEMURON)(®) ................................................................... 15 VECURONIUM BROMIDE (NORCURON)(®) ................................................................. 16 © 2019 LFEMS Medication Assisted -

Australian Product Information Esmeron
AUSTRALIAN PRODUCT INFORMATION ESMERON® (Rocuronium bromide) 1 NAME OF THE MEDICINE Rocuronium bromide 2 AND 3 QUALITATIVE AND QUANTITATIVE COMPOSITION AND PHARMACEUTICAL FORM Esmeron 25mg = 2.5mL, Esmeron 50mg = 5mL and Esmeron 100mg = 10mL contain rocuronium bromide 10mg/mL, and the following excipients: sodium acetate, sodium chloride, glacial acetic acid and water for injections in a clear, colourless to faintly yellow solution with a pH of 3.8 - 4.2. Rocuronium bromide is administered by intravenous bolus or infusion. 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS Rocuronium is indicated as an adjunct to general anaesthesia to facilitate endotracheal intubation during routine induction, to provide muscle relaxation and to facilitate mechanical ventilation in adults, and paediatric patients from term newborn infants to adolescents. In adults, rocuronium is also indicated as an adjunct to general anaesthesia to facilitate endotracheal intubation during rapid sequence induction when suxamethonium is contraindicated. In adults, rocuronium is also indicated as an adjunct in the intensive care unit (ICU) to facilitate mechanical ventilation. 4.2 DOSE AND METHOD OF ADMINISTRATION Like other neuromuscular blocking agents, Esmeron should only be administered by, or under supervision of, experienced clinicians who are familiar with the action and use of these drugs. The product is for single patient use and contains no antimicrobial agent. As with other neuromuscular blocking agents, the dosage of rocuronium bromide should be individualised in each patient. The anaesthetic method used, the duration of surgery, the method of sedation and the expected duration of mechanical ventilation, the possible interaction with other drugs that are administered concomitantly, and the condition of the patient should be taken into account when determining the dose. -

Bridion, INN-Sugammadex
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Bridion 100 mg/mL solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 mL contains sugammadex sodium equivalent to 100 mg sugammadex. Each vial of 2 mL contains sugammadex sodium equivalent to 200 mg sugammadex. Each vial of 5 mL contains sugammadex sodium equivalent to 500 mg sugammadex. Excipient(s) with known effect Contains up to 9.7 mg/mL sodium (see section 4.4). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear and colourless to slightly yellow solution. The pH is between 7 and 8 and osmolality is between 300 and 500 mOsm/kg. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Reversal of neuromuscular blockade induced by rocuronium or vecuronium in adults. For the paediatric population: sugammadex is only recommended for routine reversal of rocuronium induced blockade in children and adolescents aged 2 to 17 years. 4.2 Posology and method of administration Posology Sugammadex should only be administered by, or under the supervision of an anaesthetist. The use of an appropriate neuromuscular monitoring technique is recommended to monitor the recovery of neuromuscular blockade (see section 4.4). The recommended dose of sugammadex depends on the level of neuromuscular blockade to be reversed. The recommended dose does not depend on the anaesthetic regimen. Sugammadex can be used to reverse different levels of rocuronium or vecuronium induced neuromuscular blockade: Adults Routine reversal: A dose of 4 mg/kg sugammadex is recommended if recovery has reached at least 1-2 post-tetanic counts (PTC) following rocuronium or vecuronium induced blockade. -

The Neuromuscular Junction: Pharmacologic Applications During Anesthesia Page 1 Cynthia A
138 The Neuromuscular Junction: Pharmacologic Applications During Anesthesia Page 1 Cynthia A. Lien, M.D. New York, NewYork Introduction The neuromuscular junction and neuromuscular transmission are well-studied phenomenon. The system is designed to allow translation of an electrical impulse into a motor action potential and subsequent muscular contraction. While at first glance relatively simple in design, an appreciation of its complexity has added to the understanding and development of drugs used to modulate its function. That being said, there is increasing evidence that while monitors of depth of neuromuscular block lessen the degree of postoperative residual neuromuscular block, patients continue to arrive to the postanesthesia care unit with unacceptable levels of neuromuscular block and are prone to an increased incidence of critical respiratory events. A recent survey of practices of attitudes toward the use of neuromuscular blockers and use of neuromuscular blockers indicated that while approximately 20% of respondents felt that postoperative NMB was a significant problem, 66% of practitioners do not routinely administer an anticholinesterase and when they don’t approximately 40% base their decisions on clinical tests of residual neuromuscular block and absence of visible or palpable fade in response to train-of-four monitoring with conventional nerve stimulators. Quantitative monitors are available in only 5% of practices and only 10% feel that they should be part of minimal monitoring standards. The Neuromuscular Junction: Prejunctional Components The nerve terminal contains the synaptic vesicles in which acetylcholine is stored and, while they can be found throughout the motor nerve terminal, they tend to be concentrated around active zones on the nerve terminal membrane. -

In the United States District Court for the Middle District of Alabama Northern Division
Case 2:11-cv-00438-WKW-TFM Document 259 Filed 08/28/15 Page 1 of 10 IN THE UNITED STATES DISTRICT COURT FOR THE MIDDLE DISTRICT OF ALABAMA NORTHERN DIVISION THOMAS D. ARTHUR, ) ) Plaintiff, ) ) v. ) CASE NO. 2:11-cv-438-WKW ) (WO – Do Not Publish) WALTER MYERS, et al., ) ) Defendants. ) DISCOVERY ORDER I. INTRODUCTION This § 1983 lawsuit has been pending for over four years. By the time this case was reassigned to the undersigned in August 2014, the Eleventh Circuit had resolved Arthur’s appeal of the dismissal of his complaint, the former judge to whom this case was assigned had conducted a two-day evidentiary hearing on Arthur’s Eighth Amendment method-of-execution and Fourteenth Amendment equal protection claims, years of discovery had been conducted on the use of pentobarbital as the first drug in Alabama’s three-drug lethal injection protocol and the performance of the consciousness assessment, and summary judgment had been resolved with respect to Arthur’s Eighth and Fourteenth Amendment claims. All that was left to finally resolve Arthur’s claims, at least before the district court, was for the undersigned to hold a final hearing and to enter a memorandum opinion and Case 2:11-cv-00438-WKW-TFM Document 259 Filed 08/28/15 Page 2 of 10 final judgment on Arthur’s claims. However, before a final hearing could be held, the State announced in September 2014 that it had changed its lethal injection protocol to substitute midazolam hydrochloride for pentobarbital as the first drug, and rocuronium bromide for pancuronium bromide as the second drug in its three-drug cocktail. -

The Choice of Optimal Modern Muscle Relaxants (Rocuronium Bromide, Atracurium Besilate and Cisatracurius Besilate) in One-Day Surgery in Children
An archive of organic and inorganic chemical sciences DOI: 10.32474/AOICS.2020.04.000192 ISSN: 2637-4609 Research Article The choice of optimal modern muscle relaxants (rocuronium bromide, Atracurium Besilate and cisatracurius besilate) in One-day Surgery in Children Nasibova EM* Department of Pediatric Surgery, Azerbaijan Medical University, Baku *Corresponding author: Department of Pediatric Surgery, Nasibova EM, Azerbaijan Medical University, Baku Received: June 11, 2020 Published: June 25, 2020 Abstract Ideal muscle relaxant; Rocuronium bromide; Atracurium besilate; Cisatracurium besilate. The choice of the optimal muscle relaxant in one-day surgery in children with “small” surgical interventions remains relevant to this day. In modern pediatric surgery, the requirements for the quality of muscle relaxation are highest. However, along with the effectiveness of the drug, its duration and controllability of the action, as well as the safety of use, are important [1-7]. The Aim of the Study modern halogen-containing inhalation anesthetics on the duration To determine the pharmacoeconomic rationale for the rational of action of non-depolarizing muscle relaxants. Moreover, according use of muscle relaxants, depending on the duration of operations in one-day surgery in children. to the literature, the degree of this influence is different [14-20]. Material and Research Methods So, isoflurane is able to prolong the duration of muscle relaxants comparable by age and weight. The duration of anesthesia in The study was conducted in surgical clinics of the Azerbaijan by 15-20%, and sevoflurane - by 50-60% [9-13]. All groups were Medical University. The study included 156 children who were atracurium besilate, cisatracurium besilate, rocuronium bromide operated on routinely from 0 to 16 years old (risk of anesthesia I-II various groups is shown in Table 1.