Integrative Approaches to Management of Depression & Anxiety
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Variability of Major Phenyletanes and Phenylpropanoids in 16-Year-Old Rhodiola Rosea L
molecules Article Variability of Major Phenyletanes and Phenylpropanoids in 16-Year-Old Rhodiola rosea L. Clones in Norway Abdelhameed Elameen 1,* , Vera M. Kosman 2, Mette Thomsen 3, Olga N. Pozharitskaya 4 and Alexander N. Shikov 5 1 NIBIO, Norwegian Institute for Bioeconomy Research, Høghskoleveien 7, N-1431 Ås, Norway 2 St. Petersburg Institute of Pharmacy, Leningrad Region, Vsevolozhsky District, P 245 188663 Kuzmolovo, Russia; [email protected] 3 NIBIO, Norwegian Institute for Bioeconomy Research, Øst Apelsvoll, 2849 Kapp, Norway; [email protected] 4 Murmansk Marine Biological Institute of the Russian Academy of Sciences (MMBI RAS), Vladimirskaya, 17, 183010 Murmansk, Russia; [email protected] 5 St. Petersburg State Chemical Pharmaceutical University, Prof. Popov, 14, 197376 Saint-Petersburg, Russia; [email protected] * Correspondence: [email protected]; Tel.: +479-020-0875 Academic Editors: Francesco Cacciola and Lillian Barros Received: 17 June 2020; Accepted: 28 July 2020; Published: 30 July 2020 Abstract: Rhodiola rosea L. (roseroot) is an adaptogen plant belonging to the Crassulaceae family. The broad spectrum of biological activity of R. rosea is attributed to its major phenyletanes and phenylpropanoids: rosavin, salidroside, rosin, cinnamyl alcohol, and tyrosol. In this study, we compared the content of phenyletanes and phenylpropanoids in rhizomes of R. rosea from the Norwegian germplasm collection collected in 2004 and in 2017. In general, the content of these bioactive compounds in 2017 was significantly higher than that observed in 2004. The freeze-drying method increased the concentration of all phenyletanes and phenylpropanoids in rhizomes compared 1 with conventional drying at 70 ◦C. As far as we know, the content of salidroside (51.0 mg g− ) observed in this study is the highest ever detected in Rhodiola spp. -
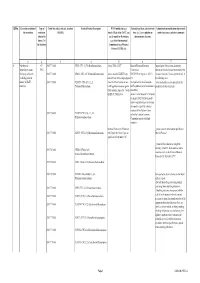
Qrno. 1 2 3 4 5 6 7 1 CP 2903 77 100 0 Cfcl3
QRNo. General description of Type of Tariff line code(s) affected, based on Detailed Product Description WTO Justification (e.g. National legal basis and entry into Administration, modification of previously the restriction restriction HS(2012) Article XX(g) of the GATT, etc.) force (i.e. Law, regulation or notified measures, and other comments (Symbol in and Grounds for Restriction, administrative decision) Annex 2 of e.g., Other International the Decision) Commitments (e.g. Montreal Protocol, CITES, etc) 12 3 4 5 6 7 1 Prohibition to CP 2903 77 100 0 CFCl3 (CFC-11) Trichlorofluoromethane Article XX(h) GATT Board of Eurasian Economic Import/export of these ozone destroying import/export ozone CP-X Commission substances from/to the customs territory of the destroying substances 2903 77 200 0 CF2Cl2 (CFC-12) Dichlorodifluoromethane Article 46 of the EAEU Treaty DECISION on August 16, 2012 N Eurasian Economic Union is permitted only in (excluding goods in dated 29 may 2014 and paragraphs 134 the following cases: transit) (all EAEU 2903 77 300 0 C2F3Cl3 (CFC-113) 1,1,2- 4 and 37 of the Protocol on non- On legal acts in the field of non- _to be used solely as a raw material for the countries) Trichlorotrifluoroethane tariff regulation measures against tariff regulation (as last amended at 2 production of other chemicals; third countries Annex No. 7 to the June 2016) EAEU of 29 May 2014 Annex 1 to the Decision N 134 dated 16 August 2012 Unit list of goods subject to prohibitions or restrictions on import or export by countries- members of the -

Chapter 16 Demand and Availability of Rhodiola Rosea L
CHAPTER 16 DEMAND AND AVAILABILITY OF RHODIOLA ROSEA L. RAW MATERIAL BERTALAN GALAMBOSI Agrifood Research Finland, Ecological Production Karilantie 2A, FIN-50600 Mikkeli, Finland E-mail: [email protected] Abstract. Rhodiola rosea L. roseroot, (Golden root or Arctic root) is a herbaceous perennial plant of the family Crassulaceae. The yellow-flowered roseroot species is a circumpolar species of cool temperate and sub-arctic areas of the northern hemisphere, including North America, Greenland, Iceland and the Altai, Tien-Shan, Himalaya mountains in Asia. The European distribution includes Scandinavia and most of the mountains of Central Europe. Roseroot has traditionally been used in Russia and Mongolia for the treatment of long-term illness and weakness caused by infection. Rhodiola radix and rhizome is a multipurpose medicinal herb with adaptogenic properties: it increases the body’s nonspecific resistance and normalizes body functions. A special emphasis in pharmacological research has been put on roseroot in the former Soviet Union. Several clinical studies have documented roseroot’s beneficial effects on memory and learning, immune- response stress and cancer therapy. Rhodiola preparations have widely been used to increase the stress tolerance of the cosmonauts. Salidroside and its precursor tyrosol, and cinnamic glycosides (rosin, rosavin and rosarin) have been identified from the roots and rhizome. Other important constituents are flavonoids, tannins and gallic acid and its esters (Brown et al. 2002). Based on the documented pharmacological effects and its safe use, the commercial interest for roseroot-based products has quickly increased worldwide. Presently one of the biggest problems is to meet the raw-material requirement for the growing industrial demand. -
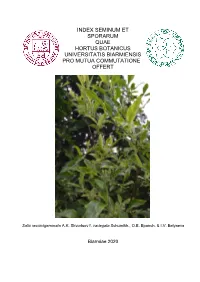
Index Seminum Et Sporarum Quae Hortus Botanicus Universitatis Biarmiensis Pro Mutua Commutatione Offert
INDEX SEMINUM ET SPORARUM QUAE HORTUS BOTANICUS UNIVERSITATIS BIARMIENSIS PRO MUTUA COMMUTATIONE OFFERT Salix recurvigemmata A.K. Skvortsov f. variegata Schumikh., O.E. Epanch. & I.V. Belyaeva Biarmiae 2020 Federal State Autonomous Educational Institution of Higher Education «Perm State National Research University», A.G. Genkel Botanical Garden ______________________________________________________________________________________ СПИСОК СЕМЯН И СПОР, ПРЕДЛАГАЕМЫХ ДЛЯ ОБМЕНА БОТАНИЧЕСКИМ САДОМ ИМЕНИ А.Г. ГЕНКЕЛЯ ПЕРМСКОГО ГОСУДАРСТВЕННОГО НАЦИОНАЛЬНОГО ИССЛЕДОВАТЕЛЬСКОГО УНИВЕРСИТЕТА Syringa vulgaris L. ‘Красавица Москвы’ Пермь 2020 Index Seminum 2020 2 Federal State Autonomous Educational Institution of Higher Education «Perm State National Research University», A.G. Genkel Botanical Garden ______________________________________________________________________________________ Дорогие коллеги! Ботанический сад Пермского государственного национального исследовательского университета был создан в 1922 г. по инициативе и под руководством проф. А.Г. Генкеля. Здесь работали известные ученые – ботаники Д.А. Сабинин, В.И. Баранов, Е.А. Павский, внесшие своими исследованиями большой вклад в развитие биологических наук на Урале. В настоящее время Ботанический сад имени А.Г. Генкеля входит в состав регионального Совета ботанических садов Урала и Поволжья, Совет ботанических садов России, имеет статус научного учреждения и особо охраняемой природной территории. Основными научными направлениями работы являются: интродукция и акклиматизация растений, -

Rhodiola Rosea L
u Ottawa l.'Univcrsilc! cnnnrlicwu- Cnnodn's univcrsiiy FACULTE DES ETUDES SUPERIEURES ls=l FACULTY OF GRADUATE AND ET POSTOCTORALES U Ottawa POSDOCTORAL STUDIES L*University canadiennc Canada's university Vicky J. Filion AUTEUR DETATHISET/ AUTHOR OF THESIS" M_.Sc. (Biology) GRADE/DEGREE Department of Biology TAMTE"TCOLirDpARTEMENT~^ACUITY, S*CHOdi~DEWRTMENT" A Novel Phytochemical and Ecological Study of the Nunavik Medicinal Plant Rhodiola rosea L. TITRE DE LA THESE / TITLE OF THESIS _____„„____Dr._ J. Arnason A. Cuerrier EXAMINATEURS (EXAMINATRICES) DE LA THESE / THESIS EXAMINERS Dr. C. Charest Dr. J. Kerr Dr. N. Cappuccino _Garjr\V^SJatCT_ Le Doyen de la Faculte des etudes superieures et postdoctorales I Dean of the Faculty of Graduate and Postdoctoral Studies A Novel Phytochemical and Ecological Study of the Nunavik Medicinal Plant Rhodiola rosea L. Vicky J. Filion Thesis submitted to the Faculty of Graduate and Postdoctoral Studies University of Ottawa in partial fulfillment of the requirements for the M.Sc. degree in the Ottawa-Carleton Institute of Biology These soumise a la Faculte des etudes superieures et postdoctorales Universite d'Ottawa en vue de l'obtention de la maitrise es sciences Institut de biologie d'Ottawa-Carleton © Vicky J. Filion, Ottawa, Canada, 2008 Library and Bibliotheque et 1*1 Archives Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington Ottawa ON K1A0N4 Ottawa ON K1A0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-50879-4 -

Rhodiola Rosea: a Phytomedicinal Overview By
Rhodiola rosea: A Phytomedicinal Overview by Richard P. Brown, M.D., Patricia L. Gerbarg, M.D., and Zakir Ramazanov, Ph.D., D.S. Rhodiola rosea L., also known as "golden root" or "roseroot" belongs to the plant family Crassulaceae.1 R. rosea grows primarily in dry sandy ground at high altitudes in the arctic areas of Europe and Asia.2 The plant reaches a height of 12 to 30 inches (70cm) and produces yellow blossoms. It is a perennial with a thick rhizome, fragrant when cut. The Greek physician, Dioscorides, first recorded medicinal applications of rodia riza in 77 C.E. in De Materia Medica.3 Linnaeus renamed it Rhodiola rosea, referring to the rose-like attar (fragrance) of the fresh cut rootstock.4 For centuries, R. rosea has been used in the traditional medicine of Russia, Scandinavia, and other countries. Between 1725 and 1960, various medicinal applications of R. rosea appeared in the scientific literature of Sweden, Norway, France, Germany, the Soviet Union, and Iceland.2,4-12 Since 1960, more than 180 pharmacological, phytochemical, and clinical studies have been published. Although R. rosea has been extensively studied as an adaptogen with various health-promoting effects, its properties remain largely unknown in the West. In part this may be due to the fact that the bulk of research has been published in Slavic and Scandinavian languages. This review provides an introduction to some of the traditional uses of R. rosea, its phytochemistry, scientific studies exploring its diverse physiological effects, and its current and future medical applications. Rhodiola rosea in Traditional Medicine Traditional folk medicine used R. -

Rhodiola Rosea in Nunatsiavut
ETHNOBOTANICAL ENTREPRENEURSHIP FOR INDIGENOUS BIOCULTURAL RESILIENCE: RHODIOLA ROSEA IN NUNATSIAVUT © Vanessa Mardones A thesis submitted to the School of Graduate Studies In partial fulfillment of the Requirements for the degree of Doctorate of Philosophy Department of Biology/Faculty of Science Memorial University of Newfoundland Submitted August 2019 St. John’s Newfoundland Table of Contents Abstract ............................................................................................................................................ 1 Chapter 1. General Introduction .................................................................................................. 2 1.1 Introduction ............................................................................................................................................. 2 1.2 Thesis Outline ......................................................................................................................................... 6 1.3 Co-Authorship Statement ..................................................................................................................... 9 1.4 References ............................................................................................................................................... 9 Chapter 2. Assessing the Impact of Environmental Variables on Growth and Phytochemistry of Rhodiola rosea in Coastal Labrador to Inform Small-Scale Enterprise. 15 Abstract ....................................................................................................................................................... -

00044821 Prodoc 00052843
UNDP Project Document Government of the Republic of Kazakhstan United Nations Development Programme Global Environment Facility PIMS 2898 Atlas Award 00044821 Atlas Project No: 00052843 Conservation and Sustainable Use of Biodiversity in the Kazakhstani Sector of the Altai-Sayan Ecoregion Brief description The goal of the project is to help secure the globally significant biodiversity values of the Kazakhstan. The project’s objective is to enhance the sustainability and conservation effectiveness of Kazakhstan’s national PA system by demonstrating sustainable and replicable approaches to conservation management in the protected areas in the Kazakhstani sector of Altai-Sayan ecoregion.The project will produce five outcomes: the protected area network will be expanded and PA management effectiveness will be enhanced; awareness of and support for biodiversity conservation and PAs will be increased among all stakeholders; the enabling environment for strengthening the national protected area system will be enhanced; community involvement in biodiversity conservation will be increased and opportunities for sustainable alternative livelihoods within PAs and buffer zones will be facilitated; and networking and collaboration among protected areas will be improved, and the best practices and lessons learned will be disseminated and replicated in other locations within the national protected area system. 1 Table of Contents SECTION I: ELABORATION OF THE NARRATIVE .......................................................................... 5 PART -

Medicinal Herbs with Anti-Depressant Effects
J Herbmed Pharmacol. 2020; 9(4): 309-317. http://www.herbmedpharmacol.com doi: 10.34172/jhp.2020.39 Journal of Herbmed Pharmacology Medicinal herbs with anti-depressant effects Mahbubeh Setorki* ID Department of Biology, Izeh Branch, Islamic Azad University, Izeh, Iran A R T I C L E I N F O A B S T R A C T Article Type: Depression is a life-threatening chronic illness which affects people worldwide. Drugs used to Review treat this disease have multiple side effects and may cause drug-drug or drug-food interactions. Additionally, only 30% of patients respond adequately to the existing drugs and the remaining Article History: do not achieve complete recovery. Thus, finding effective treatments that have adequate Received: 10 November 2018 efficacy, fewer side effects and lower cost seem to be necessary. The purpose of this study was Accepted: 24 January 2019 to review animal and double-blind clinical studies on the anti-depressant effects of medicinal herbs. In this study, validated scientific articles indexed in PubMed, SID, Web of Science and Keywords: Scopus databases were reviewed. A database search was performed using the following terms: Depression clinical trials, depression, major depressive disorder, essential oil, extract and medicinal plant. Clinical trials Positive effects of a number of herbs and their active compounds such as St John’s-wort, saffron, Medicinal plants turmeric, ginkgo, chamomile, valerian, Lavender, Echium amoenum and Rhodiola rosea L. in Herbal medicines improvement of symptoms of mild, moderate or major depression have been shown in clinical trials. The above plants show antidepressant effects and have fewer side effects than synthetic drugs. -

Index Seminum Et Sporarum Perm, 2013
INDEX SEMINUM ET SPORARUM QUAE HORTUS BOTANICUS UNIVERSITATIS BIARMIENSIS PRO MUTUA COMMUTATIONE OFFERT СПИСОК СЕМЯН И СПОР , предлагаемых для обмена Ботаническим садом имени проф . А.Г. Генкеля Пермского государственного национального исследовательского университета Пермь , Россия Biarmiae 2013 Federal State Budgetary Educational Institution of Higher Professional Education «Perm State University», Botanic Garden ______________________________________________________________________________________ Дорогие друзья ботанических садов , Дорогие коллеги ! Ботанический сад Пермского государственного национального исследовательского университета был создан в 1922 г. по инициативе и под руководством проф . А.Г. Генкеля . Здесь работали известные ученые – ботаники Д.А. Сабинин , В.И. Баранов , Е.А. Павский , внесшие своими исследованиями большой вклад в развитие биологических наук на Урале . В настоящее время Ботанический сад имени профессора А.Г. Генкеля входит в состав регионального Совета ботанических садов Урала и Поволжья , имеет статус научного учреждения и особо охраняемой природной территории . Основными научными направлениями работы являются : интродукция и акклиматизация растений , выведение и отбор новых форм и сортов , наиболее стойких и продуктивных в местных условиях . Ботанический сад расположен на двух участках общей площадью 2,7 га . Коллекции включают около 4000 видов , форм и сортов древесных , кустарниковых и травянистых растений , произрастающих в открытом и закрытом грунте . Из оранжерейных растений полнее всего представлены -

Rhodiola Rosea: from the Adaptogenic Role to the Anti-Adipogenic Effect?
Metab y & o g lic lo S o y n n i r d c r Endocrinology & Metabolic o o m d n e E Colitti., Endocrinol Metab Synd 2014, 3:3 ISSN: 2161-1017 Syndrome DOI: 10.4172/2161-1017.1000e123 Editorial Open Access Rhodiola rosea: From the Adaptogenic Role to the Anti-Adipogenic Effect? Monica Colitti* Department of Scienze Agrarie e Ambientali, Università di Udine, via delle Scienze, 206 – 33100 Udine, Italy *Corresponding author: Monica Colitti Department of Scienze Agrarie e Ambientali, via delle Scienze, 208 – 33100 Udine, Italy, Tel: +390432558583; Fax: +390432558603; E-mail: [email protected] Received date: Sep 09, 2014, Accepted date: Sep 11, 2014, Published date: Sep 16, 2014 Copyright: © 2014 Colitti M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Editorial visceral fat weight by 30% of rats fed with high fat diet, having a direct effect on sympathetic tone and on hypothalamic norepinephrine Many natural phytonutrients have beneficial effects on health [1,2]. secretion [8]. Although detailed molecular mechanism of the lipid In addition, several botanicals have received positive attention, based lowering and anti-inflammation effects of salidroside are to be on their relative safety and the accumulation of evidence of their identified, in vivo studies on high fat diet-fed LDLr−/− mice antiadipogenic and metabolic effects in animals and humans [3]. demonstrated that this RR compound reduced serum lipid levels and Natural products can decrease of lipid absorption, energy intake, decreased atherosclerotic plaques formation [38]. -

Immunmodulatory and Antiproliferative Properties of Rhodiola Species*
952 Reviews Immunmodulatory and Antiproliferative Properties of Rhodiola Species* Authors Mari-Carmen Recio, Rosa-María Giner, Salvador Máñez Affiliation Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Valencia, Spain Key words Abstract sponsible for many of the effects observed with l" Rhodiola ! Rhodiola extracts. l" salidroside The traditional medicines of Asia and Europe have The aim of this paper is to review the pharmaco- l" adaptatogen long used various Rhodiola species, which are en- logical effects not only of various Rhodiola species, l" antitumor demic to the subarctic areas of the northern mainly R. rosea along with Rhodiola imbricata, l" immunostimulant l" antioxidant hemisphere, as tonic, adaptogen, antidepressant, Rhodiola algida,andRhodiola crenulata, but also and anti-inflammatory drugs. In order to estab- of salidroside, focusing especially on its antioxi- lish the therapeutic uses of these plants in mod- dant, immunomodulatory, antitumoral, and anti- ern medicine, the pharmacological effects of Rho- proliferative activities, as well as to describe their diola sp. have been widely studied. Indeed, the therapeutic significance in disease management. most amply researched species, Rhodiola rosea, Although previous pharmacological studies have has been shown to possess antioxidant, adapto- established a scientific basis for possible thera- genic, antistress, antimicrobial, immunomodula- peutic uses of Rhodiola extracts and salidroside, tory, angiomodulatory, and antitumoral effects. high-quality, randomized, controlled clinical tri- Salidroside (p-hydroxyphenethyl-β-D-glucoside), als are still needed. a major compound in Rhodiola, seems to be re- Introduction as catechin and gallic acid) (l" Fig. 1) have been ! proposed as reference markers [1]. Rhodiola species are herbaceous perennial plants The roots and rhizomes of Rhodiola species have of the Crassulaceae family that have been used ex- been reported to contain distinct groups of chem- tensively in the traditional medicines of both Asia ical compounds.