Guide Yellow Fever Outbreak 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Haitian Revolution Strategy
How to Win a War Without Even Shooting: Haitian Revolution Strategy Lynn Gourinski Fahr Overbrook High School Overview Rationale Objectives Strategies Classroom Activities Annotated Biographies/Works Cited/Resources Appendix/Content Standards Overview: The Haitian Revolution largely impacted world history albeit a small country. The war and the success of the enslaved peoples became the forerunner to modern anti- colonialism movements in the Third World and caused the world to pause and think. During the time of the Haitian Revolution (1791-1804), slaves outnumbered white slave owner’s 10:1.(Garrigus, 2006). The western Caribbean was alive with conquests and movement both socially and politically. It was also caught in a whirlwind of disease being brought from place to place-on ships and brought inland through the purchases of goods and slaves. Yellow Fever and Cholera wiped out thousands of persons in the Caribbean islands, many in just a few hours. But why was Haiti not as hard hit by cholera as other nations in the Caribbean. Why did Yellow Fever play such a pivotal role in the successful uprising of slaves? Many diseases might be prevented through good hygiene and development, while others were common to native peoples but wreaked havoc on troops employed to put down revolutions. Such was the case in Haiti, where of the 162,000 troops, up to 40,000 sent by Napoleon, were killed in attempts to reconquer the slaves and restore order in Haiti as Yellow Fever reared it's ugly head to kill many foreign invaders. (Peterson, 1995) Rationale: This curriculum can be taught in history classes for grades 7-12 in conjunction with a health class currently studying a universal hygiene unit. -

Yellow Fever and Aedes Aegypti Eradication
Al cannuct Peort ¡ of the director / / : a. ~11 · · . * a · =. *~~~· * * * a e -e. * PUBTICATIONS OF THE PAN AMEECAN SANITARY BUREAU OFFICIAL DOCUMENTS Nos. 19-21 Annual Report of the Director, 1956 N .19 Informe Anual del Director, 1956 Nº 19 Financial Report of the Director and External Auditor's Report, 1956 N - 20 Informe Financiero del Director e Informe del Auditor Externo, 1956 N9 20 Proposed Program and Budget Estimates, 1958-59 N 20 Proyectos de Programa y Presupuesto, 1958-59 No 20 t PAN AMERICAN SANITARY ORGANIZATION Official Documents May 1957 No. 19 ANNUAL REPORT OF THE DIRECTOR OF THE PAN AMERICAN SANITARY BUREAU REGIONAL OFFICE FOR THE AMERICAS OF THE WORLD HEALTH ORGANIZATION 1956 PAN AMERICAN SANITARY BUREAU Regional Office of the World Health Organization 1501 New Hampshire Avenue, N.W. Washington 6, D.C. iii ,11165 /0 To the Member States of the Pan American Sanitary Organization I have the honor to transmit herewith the Annual Report of the Pan American Sanitary Bureau, Regional Office for the Americas of the World Health Organiza- tion, for the year 1956. This Report covers the work of the Washington Office as well as that of the Zone Offices. It describes projects implemented in collaboration with the governments of Member States and with other international organizations. The Financial Statement for the year, is submitted separately. Respectfully yours, Fred L. Soper Director iv ANNUAL REPORT O F THE DIRE CTOR 19 56 V ANNUAL REPORT of the DIRECTOR 1956 CONTENTS* Page Part I Introductory Review ......................... 1 Part II Activities in 1956 .......................... 21 Communicable Diseases ................... -
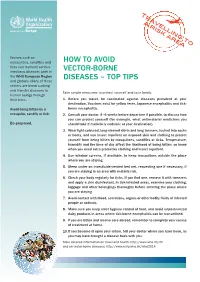
Top Tips How to Avoid Vector Borne Diseases (Eng)
Tr a a v r e i ljl s k in a g r e to a Vectors such as mosquitoes, sandflies and HOW tO AvOid ticks can transmit serious infectious diseases both in vEctOR-BORnE the WHO European Region disEAsEs – tOp tips and globally. Many of these vectors are blood sucking and transfer diseases to Take simple measures to protect yourself and your family. human beings through their bites. 1. Before you travel, be vaccinated against diseases prevalent at your destination. vaccines exist for yellow fever, Japanese encephalitis and tick- Avoid being bitten by a borne encephalitis. mosquito, sandfly or tick. 2. consult your doctor, 4–6 weeks before departure if possible, to discuss how you can protect yourself (for example, what antimalarial medicines you Be prepared. should take if malaria is endemic at your destination). 3. Wear light-coloured, long-sleeved shirts and long trousers, tucked into socks or boots, and use insect repellent on exposed skin and clothing to protect yourself from being bitten by mosquitoes, sandflies or ticks. temperature, humidity and the time of day affect the likelihood of being bitten, so know when you need extra protective clothing and insect repellent. 4. Use window screens, if available, to keep mosquitoes outside the place where you are staying. 5. sleep under an insecticide-treated bed net, requesting one if necessary, if you are staying in an area with malaria risk. 6. check your body regularly for ticks. if you find one, remove it with tweezers and apply a skin disinfectant. in tick-infested areas, examine your clothing, luggage and other belongings thoroughly before entering the place where you are staying. -

Yellow Fever
Infectious Disease Epidemiology Section Office of Public Health, Louisiana Dept of Health & Hospitals 800-256-2748 (24 hr. number), (504) 568-8313 www.infectiousdisease.dhh.louisiana Yellow Fever Revised 06/03/2016 Yellow fever is caused by a Flavivirus (the family which includes dengue, West Nile, Saint Louis en- cephalitis and Japanese encephalitis) Epidemiology Yellow fever is transmitted by Aedes aegypti and other mosquitoes. It is naturally occurring in Africa and South America, but the anthroponotic (vector-borne person-to-person) transmission of the virus may oc- cur wherever a suitable vector is present (Figure). Figure: Yellow Fever Endemic Zones in Africa (left) and South America (right) In the southern United States where A. aegypti is present, epidemics of urban yellow fever occurred. Yel- low fever was transmitted by A. aegypti mosquitoes that are infected after feeding on viremic humans and then spread the infection in subsequent feeding attempts. ------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- Louisiana Office of Public Health – Infectious Disease Epidemiology Section- Epidemiology Manual Page 1 of 5 Urban cycle The urban cycle involves human hosts and A.aegypti vector. For over 200 years it was a major killer in U.S. port cities (1,000 deaths in the last major epidemic in New Orleans in 1905). Elimination efforts un- dertaken in the early 1900s led to the complete elimination of yellow fever as an urban epidemic in the Americas in the 1930’s (the last urban American cases occurred in northeastern Brazil). This was one of the most successful eradication campaigns in public health. Sylvatic cycle The sylvatic cycle involves forest primates, principally monkeys and forest canopy mosquitoes. -

Epidemics Investigated
EPIDEMICS INVESTIGATED During the lifetime of CAREC staff members were called existence of “jungle yellow fever” was proven some 30 upon to investigate a variety of disease outbreaks, such years later in Brazil. Dr T H G Aitken, entomologist at as the periodic occurrence of yellow fever in Trinidad the TRVL, suggested the possibility of the existence of and pan Caribbean epidemics of dengue fever. Dengue a 10-15 year cycle in the upsurge of yellow fever activity indeed is endemic in CAREC Member Countries (CMCs) in Trinidad (Aitken 1991), if not in humans, certainly in even though at one time the Cayman Islands was free monkeys. of Aedes aegypti. Malaria is still present in some CMCs such as Belize, Guyana and Suriname. It is also present The report of dead Howler monkeys (Fig. 6.1.1) in the in Haiti. Food-borne illnesses were common due to the Guayaguayare forests of south-eastern Trinidad in lack of proper hygienic standards and there were periodic November 1978 set alarm bells ringing. A team of staff outbreaks in the countries. Some of the outbreaks members of the Veterinary Public Health Unit, Insect investigated are highlighted below. Fig. 6.1.1. A dead Howler monkey, Alouatta seniculus found on Vector Control Division, Forestry Division and CAREC the forest floor at Fishing Pond, north-eastern Trinidad. visited the area to determine the veracity of the reports. Photo: Elisha Tikasingh Yellow Fever A dead Howler monkey was found, as well as other evidence to suggest more than one monkey had died. Yellow fever was once a scourge in the West Indies and has been documented since the 1600s. -

Disease and Social Disruption
Disease and Social Disruption 2 Connect-the-Dots: Making Meaning from Historical Evidence Chris Edwards 5 Yellow Fever in Philadelphia, 1793 (Book Review) Sandra W. Moss 9 World War I Posters: Thinking Critically about History and the Media Tom Carty 16 On the Trail of an Epidemic: Yellow Fever in New Orleans, 1845-1860 Supplement to National Council for the Social Studies Publications Number 31 January/February 2008 www.socialstudies.org Middle Level Learning 31, pp. M2–M4 ©2008 National Council for the Social Studies On the Cover: Nurse wearing a mask as Connect-the-Dots: protection against influ- enza. September 13, 1918. In October of 1918, Congress approved a Making Meaning from $1 million budget for the U. S. Public Health Service to recruit 1,000 medical doctors and Historical Evidence over 700 registered nurses. Nurses were scarce, as their proximity to and interaction with the disease increased the risk of death. Chris Edwards Source: National Archives, “The Deadly Virus: The Influenza Epidemic of 1918,” www.archives.gov/ exhibits/influenza-epidemic/ (Western Newspaper Union). It is often lamented that exciting historical scholarship rarely trickles into the In the case of Pizarro’s conquest of the secondary classroom. I define my job as an eighth grade history teacher as being a Inca’s, I present five dots in this order: bridge between historical scholars and my students. For example, I believe that part of my work is to read a Pulitzer-winning book like Jared Diamond’s Guns, Germs, • Several species of large animals and Steel: The Fates of Human Societies and make its basic insights accessible to were domesticated in Europe, Asia, middle school students, to show how Diamond’s thesis connects to aspects of history and Africa, providing humans with covered in the curriculum.1 I call what I do “the connect-the-dots method,” and the mechanical power and food. -
Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever
C o m p r e h e n s Dengue fever (DF) is the fastest emerging arboviral infection spread by Aedes aegypti i v mosquitoes with major public health consequences for millions of people around the e G world, and in particular the South-East Asia and Asia-Pacific Regions of the World u i Health Organization (WHO). Of the 2.5 billion people globally at risk of DF and its d e severe forms dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS) l i n South-East Asia accounts for approximately 1.3 billion or 52%. e s f As the disease spreads to new geographical areas, the frequency of the o r outbreaks has increased along with a rapidly changing disease epidemiology. In P r response to resolution of the Forty-sixth World Health Assembly urging Member e v States to strengthen national programmes for control of DF/DHF, several documents e n were developed by regional offices of WHO, including South-East Asia. t i o In 1999 the WHO Regional Office for South-East Asia published the Regional n a Comprehensive Guidelines for Guidelines for the Prevention and Control of DF/DHF. Since then new strategies and n d developments in the control of dengue fever, DHF and DSS have come to light. The C Regional Guidelines were extensively revised, updated and expanded with the focus o n Prevention and Control of on new and additional topics of current relevance to the populations of Member t r o States of the Region. They were then rechristened the Comprehensive Guidelines for l o the Prevention and Control of Dengue and Dengue Haemmorhagic Fever. -

Yellow Fever – the Scourge Revealed
Yellow Fever – The Scourge Revealed Stanton E. Cope, Ph.D. Captain United States Navy Note to user: This text accompanies a Powerpoint presentation. When you see a red © in the text, it indicates that you should click the mouse . Slide 1 – Title The following story is that of a prolific and savage killer, yellow fever, and the events by which the veil of this terrible scourge was lifted. Some of the heroes’ names will be familiar to you but most will not. My presentation contains three parts: first, I will present a brief history of yellow fever and its impact on society; second, I will outline the experiments done in Cuba which elucidated the mode of transmission of this disease (C); and finally I will tell you about two young men and their heroic roles in one of the great medical discoveries of our time. Slide 2 – Cartoon of YF in the Americas We believe that yellow fever originated in Africa and made its first visit to the New World in the late 16th or early 17th century. For the next 300 years or so, the disease ravaged hundreds of cities in North America from Texas to Massachusetts as well as the Great Mississippi Valley. Each wave of pestilence was marked by economic shamble, human panic, and widespread death. From 1668 to 1893, there were 135 major epidemics in U.S. port cities. In 1793, yellow fever claimed 1 of every 10 Philadelphians, 1 a total of 4,000 dead. New Orleans, a frequent victim of attack, suffered 29,000 cases and over 8,000 dead in 1853. -

How Can We Use Genetic Engineering to Get Rid of Malaria for Good?
DECEMBERMARCH 20172020 How can we use genetic engineering to get rid of malaria for good? Authors: Susan Crow, Meghan Pawlowski, Manyowa Meki, LaraAuthors: LaDage, Timothy Roth II, Cynthia Downs, BarryKyros SinervoKyrou, Andrew and Vladimir Hammond, Pravosudov Andrea Crisanti & others Associate Editors: LindseySeda Dawson Hall and and Gogi Madeleine Kalka Corcoran Abstract Nobody likes the buzzing sound or itchy bite of mosquitoes. What if we used genetic engineering? Here we modified But mosquito bites (only females bite, by the way!) are not the genetic makeup of Anopheles gambiae mosquitoes (the just irritating: they can carry and spread deadly diseases main carriers of malaria). The mutation prevented females such as malaria, dengue, yellow fever and many more. Every from biting and laying eggs. It spread through our caged year, millions of people die from mosquito-borne diseases and populations quickly and drove them extinct. Our results pave most of them are young children. There are ways to get rid the way for lowering mosquito populations in the wild and of mosquitoes and prevent such diseases, but they are not as getting rid of malaria in the future. effective as we would like. EDITING GENES WITH CRISPR A tool used by scientists to precisely edit genes inside cells. Introduction It consists of two parts… Cas9 Guide RNA (An enzyme that (Directs the Cas9 You may have heard about malaria and the devastation it cuts DNA) + to the target DNA) causes in Africa. But did you know that a child dies of malaria every two minutes? Despite global efforts, malaria remains one of the world’s deadliest diseases. -

Yellow Fever: the Complete Symposium
Thomas Jefferson University Jefferson Digital Commons Yellow fever, a symposium in commemoration of Carlos Juan Finlay, 1955 Jefferson History and Publications 9-1955 Yellow Fever: The Complete Symposium Follow this and additional works at: https://jdc.jefferson.edu/yellow_fever_symposium Part of the History of Science, Technology, and Medicine Commons Let us know how access to this document benefits ouy Recommended Citation "Yellow Fever: The Complete Symposium" (1955). Yellow fever, a symposium in commemoration of Carlos Juan Finlay, 1955. Paper 12. https://jdc.jefferson.edu/yellow_fever_symposium/12 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Yellow fever, a symposium in commemoration of Carlos Juan Finlay, 1955 by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. YELLOW FEVER A SYMPOSIUM IN COMMEMORATION OF CARLOS JUAN FINLAY BOSHELL III. BUGHER DOWNS KERR IIIAHAFFY NOGUEffiA ORENSTEIN PINTO SEVERO SIIIADEL SOPER THE JEFFERSON IIIEDlCAL COLLEGE of PHILADELPHIA 22-23 SEPTEIIIBER 1955 The addresses in this symposium were designated as William Potter Memorial Lectures Mr. Potter was a member of the Board of Trustees of the jefferson Medical College from 1894-1926 and its president from 1897-1926. -

Yellow Fever
WHO/EPI/GEN/98.11 ORIGINAL: ENGLISH DISTR.: GENERAL Yellow fever Written by: Dr Jari Vainio and Dr Felicity Cutts, London School of Hygiene and Tropical Medicine DIVISION OF EMERGING AND OTHER COMMUNICABLE DISEASES SURVEILLANCE AND CONTROL GLOBAL PROGRAMME FOR VACCINES AND IMMUNIZATION EXPANDED PROGRAMME ON IMMUNIZATION World Health Organization Geneva 1998 The Global Programme for Vaccines and Immunization thanks the donors whose unspecified financial support in 1997 has made the production of this document possible. Ordering code: WHO/EPI/GEN/98.11 Printed : September 1998 This documents is available on the Internet at: http://www.who.ch/gpv-documents/ Copies may be requested from: World Health Organization Global Programme for Vaccines and Immunization CH-1211 Geneva 27, Switzerland • Fax: +22 791 4193/4192 • E-mail: [email protected] • © World Health Organization 1998 This document is not a formal publication of the World Health Organization (WHO), and all rights are reserved by the Organization. The document may, however, be freely reviewed, abstracted, reproduced and translated, in part or in whole, but not for sale nor for use in conjunction with commercial purposes. The views expressed in documents by named authors are solely the responsibility of those authors. 2 Yellow fever Contents Glossary ............................................................................................................................. v List of abbreviations ...................................................................................................... -

How Can We Use Genetic Engineering to Get Rid of Malaria for Good? Teacher’S Key
How can we use genetic engineering to get rid of malaria for good? TEACher’s key Check your understanding 1 Anopheles gambiae mosquitoes are a vector species for malaria. What is a vector species? Can you find out about some other vector species and the diseases they transmit? A vector is an organism that does not cause disease itself but which spreads infection by transmitting pathogens (virus, bacteria, parasites, etc.) from one host to another. Mosquitoes are vector species of many infectious diseases including malaria, dengue, yellow fever, Zika, and West Nile virus. Some other vector species are ticks (Lyme Answer disease), fleas (bubonic plague), raccoons, bats, foxes, skunks (rabies). Scientists genetically engineered Anopheles gambiae mosquitoes. What were the characteristics of engineered 2 mosquitoes that drove the lab populations to extinction? Male mosquitoes with one or both copies of the mutated gene had no physical differences but they were carriers of the mutated gene and passed it onto their offspring. Female mosquitoes with one copy of the mutated gene were healthy but they had reduced fertility. They passed the mutated gene on to the next generation. Females with two copies of the mutated gene had male body parts (a mouth that is not structured to bite, claspers, and hairy Answer antennae). Most importantly, they were infertile - they couldn’t lay eggs. So once all females carried two copies of the mutated gene, the population collapsed. 3 Scientists used a new approach that made this study so successful at wiping out mosquito populations: CRISPR/Cas9 gene drive. What is the purpose of a gene drive? How does it speed up the spread of a useful genetic mutation? In sexual reproduction, half of the genes come from the male organism and the other half come from the female organism.