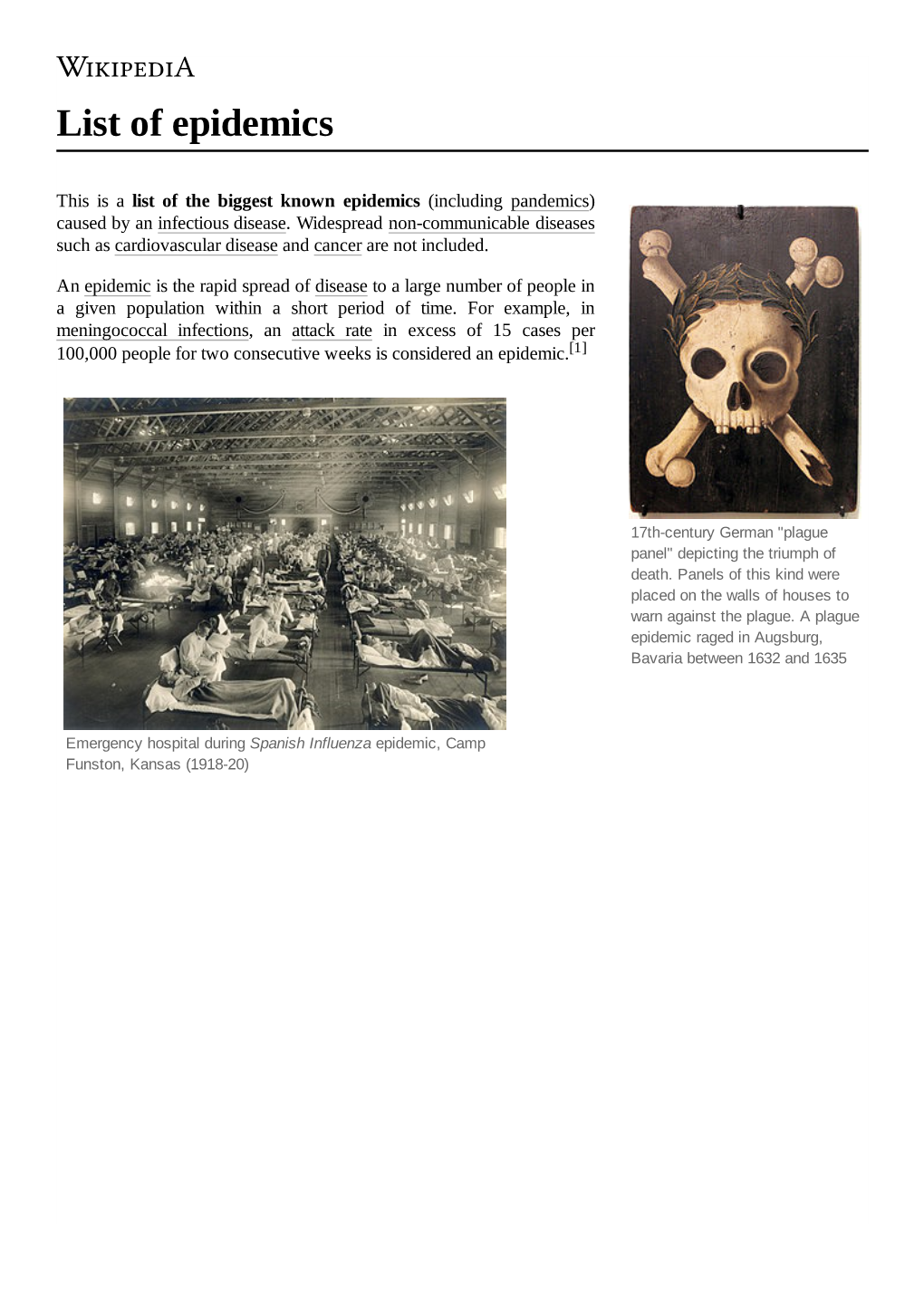
List of Epidemics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Small Drinking Water Systems Project
Strong evidence, stronger public health Small Drinking Water-borne Disease Outbreaks in Water Systems Canadian Small Drinking Water Systems Project Hannah Moffatt, Sylvia Struck Report Highlights Information about Canadian drinking water systems and past water-borne disease outbreaks is incomplete and non-standardized. Standard definitions and coordinated surveillance systems for water-borne disease outbreaks would help inform policy and practice. A relatively high proportion of past water-borne disease outbreaks in Canada are estimated to have occurred in small drinking water systems serving populations of 5,000 people or less. Water-borne disease outbreaks in small drinking water systems are often the result of a combination of water system failures; contributing factors often include a lack of source water protection and inadequate drinking water treatment. Analyses suggest small drinking water systems face challenges associated with infrastructure, technology, and financial constraints. Investments in drinking water systems and operator training have the potential to reduce the burden of water-borne disease in Canada. Executive Summary Generally, Canadians have access to safe and secure drinking water. However, as demonstrated by the events of Walkerton in 2000, the exception can be tragic. Outbreaks of water-borne disease are preventable, yet evidence-informed policy and practice is hampered, in part, by our limited knowledge of drinking water systems that experience outbreaks and the factors that contribute to outbreaks in Canada. There is no national surveillance system for systematic collection of water-borne disease outbreak data. Investigating past water-borne disease outbreaks is a valuable approach to collect information to inform practice and policy. Investigations of water-borne disease outbreaks are challenging because the outbreak events are rare, the pathogenic agents involved may be transmitted via multiple routes (e.g., person to person, food-borne, as well as water-borne), and gastrointestinal illnesses are frequently under-reported. -

Pandemic Flu Planning for Schools
PandemicPandemicPandemic FluFluFlu PlanningPlanningPlanning forforfor SchoolsSchoolsSchools EdenEden Wells,Wells, MD,MD, MPHMPH Michigan Department of Community Health Influenza Strains •Type A – Infects animals and humans –Moderate to severe illness – Potential epidemics/pandemics • Type B – Infects humans only Source: CDC – Milder epidemics – Larger proportion of children affected •Type C –No epidemics –Rare in humans A’s and B’s, H’s and N’s • Classified by its RNA core – Type A or Type B influenza • Further classified by surface protein – Neuraminidase (N) – 9 subtypes known – Hemagluttin (H) – 16 subtypes known • Only Influenza A has pandemic potential Influenza Virus Structure Type of nuclear material Neuraminidase Hemagglutinin A/Moscow/21/99 (H3N2) Virus Geographic Strain Year of Virus type origin number isolation subtype Influenza Overview • Orthomyxoviridae, enveloped RNA virus •Strains –Type A –Type B –Type C Source: CDC • Further classified by surface protein –Neuraminidase (N) – 9 subtypes known – Hemagglutinin (H) – 16 subtypes known Influenza A: Antigenic Drift and Shift • Hemagglutinin (HA) and neuraminadase (NA) structures can change •Drift: minor point mutations – associated with seasonal changes/epidemics – subtype remains the same •Shift:major genetic changes (reassortments) – making a new subtype – can cause pandemic Seasonal Influenza •October to April • People should get flu vaccine • Children and elderly most prone • ~36,000 deaths annually in U.S. Seasonal Effects Seasonal Influenza Surveillance Differentiating -

People, Plagues, and Prices in the Roman World: the Evidence from Egypt
People, Plagues, and Prices in the Roman World: The Evidence from Egypt KYLE HARPER The papyri of Roman Egypt provide some of the most important quantifiable data from a first-millennium economy. This paper builds a new dataset of wheat prices, land prices, rents, and wages over the entire period of Roman control in Egypt. Movements in both nominal and real prices over these centuries suggest periods of intensive and extensive economic growth as well as contraction. Across a timeframe that covers several severe mortality shocks, demographic changes appear to be an important, but by no means the only, force behind changes in factor prices. his article creates and analyzes a time series of wheat and factor Tprices for Egypt from AD 1 to the Muslim conquest, ~AD 641. From the time the territory was annexed by Octavian in 30 BCE until it was permanently taken around AD 641, Egypt was an important part of the Roman Empire. Famously, it supplied grain for the populations of Rome and later Constantinople, but more broadly it was integrated into the culture, society, and economy of the Roman Mediterranean. While every province of the sprawling Roman Empire was distinctive, recent work stresses that Egypt was not peculiar (Bagnall 1993; Rathbone 2007). Neither its Pharaonic legacy, nor the geography of the Nile valley, make it unrepresentative of the Roman world. In one crucial sense, however, Roman Egypt is truly unique: the rich- ness of its surviving documentation. Because of the valley’s arid climate, tens of thousands of papyri, covering the entire spectrum of public and private documents, survive from the Roman period (Bagnall 2009). -

Globalization and Infectious Diseases: a Review of the Linkages
TDR/STR/SEB/ST/04.2 SPECIAL TOPICS NO.3 Globalization and infectious diseases: A review of the linkages Social, Economic and Behavioural (SEB) Research UNICEF/UNDP/World Bank/WHO Special Programme for Research & Training in Tropical Diseases (TDR) The "Special Topics in Social, Economic and Behavioural (SEB) Research" series are peer-reviewed publications commissioned by the TDR Steering Committee for Social, Economic and Behavioural Research. For further information please contact: Dr Johannes Sommerfeld Manager Steering Committee for Social, Economic and Behavioural Research (SEB) UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR) World Health Organization 20, Avenue Appia CH-1211 Geneva 27 Switzerland E-mail: [email protected] TDR/STR/SEB/ST/04.2 Globalization and infectious diseases: A review of the linkages Lance Saker,1 MSc MRCP Kelley Lee,1 MPA, MA, D.Phil. Barbara Cannito,1 MSc Anna Gilmore,2 MBBS, DTM&H, MSc, MFPHM Diarmid Campbell-Lendrum,1 D.Phil. 1 Centre on Global Change and Health London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK 2 European Centre on Health of Societies in Transition (ECOHOST) London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK TDR/STR/SEB/ST/04.2 Copyright © World Health Organization on behalf of the Special Programme for Research and Training in Tropical Diseases 2004 All rights reserved. The use of content from this health information product for all non-commercial education, training and information purposes is encouraged, including translation, quotation and reproduction, in any medium, but the content must not be changed and full acknowledgement of the source must be clearly stated. -
History and Epidemiology of Global Smallpox Eradication Smallpox
History and Epidemiology of Global Smallpox Eradication Smallpox Three Egyptian Mummies 1570-1085 BC Ramses the Vth Died 1157 BC Early Written Description of Smallpox India 400 AD “Severe pain is felt in the large and small joints, with cough, shaking, listlessness and langour; the palate, lips, and tongue are dry with thirst and no appetite. The pustules are red, yellow, and white and they are accompanied by burning pain. The form soon ripens …the body has a blue color and seems studded with rice. The pustules become black and flat, are depressed in the centre, with much pain.” Smallpox and History • In the Elephant war in Mecca 568 AD, smallpox decimated the Ethiopian soldiers • Introduction of smallpox into the new world (Carribean 1507, Mexico 1520, Peru 1524, and Brazil 1555 ) facilitated Spanish conquest • Smallpox destroys Hottentots (1713) • In 1738, smallpox killed half the Cherokee Indian population • Smallpox disrupted colonial army in 1776 Smallpox Control Strategies • Smallpox hospitals (Japan 982 AD). • Variolation 10th Century. • Quarantine 1650s. • Home isolation of smallpox in Virginia 1667. • Inoculation and isolation (Haygarth 1793). • Jenner and widespread practice of vaccination throughout Europe and rest of the world. • Mass vaccination. • Surveillance containment. Variolation Inoculation with Smallpox Pus • Observations: – Pocked marked persons never affected with smallpox – Persons inoculated with smallpox pustular fluid or dried scabs usually had milder disease • Not ideal control strategy – Case fatality rate still 2% – Can transmit disease to others during illness The 1st Smallpox Vaccination Jenner 1796 Cowpox lesions on the hand of Sarah Nelmes (case XVI in Jenner’s Inquiry), from which material was taken for the vaccination of James Phipps below in 1796 History of Smallpox Vaccination 1805 Growth of virus on the flank of a calf in Italy. -

On Confinement and Quarantine Concerns on an SEIAR Epidemic
S S symmetry Article On Confinement and Quarantine Concerns on an SEIAR Epidemic Model with Simulated Parameterizations for the COVID-19 Pandemic Manuel De la Sen 1,* , Asier Ibeas 2 and Ravi P. Agarwal 3 1 Campus of Leioa, Institute of Research and Development of Processes IIDP, University of the Basque Country, 48940 Leioa (Bizkaia), Spain 2 Department of Telecommunications and Systems Engineering, Universitat Autònoma de Barcelona, UAB, 08193 Barcelona, Spain; [email protected] 3 Department of Mathematics, Texas A & M University, 700 Univ Blvd, Kingsville, TX 78363, USA; [email protected] * Correspondence: [email protected] Received: 7 September 2020; Accepted: 30 September 2020; Published: 7 October 2020 Abstract: This paper firstly studies an SIR (susceptible-infectious-recovered) epidemic model without demography and with no disease mortality under both total and under partial quarantine of the susceptible subpopulation or of both the susceptible and the infectious ones in order to satisfy the hospital availability requirements on bed disposal and other necessary treatment means for the seriously infectious subpopulations. The seriously infectious individuals are assumed to be a part of the total infectious being described by a time-varying proportional function. A time-varying upper-bound of those seriously infected individuals has to be satisfied as objective by either a total confinement or partial quarantine intervention of the susceptible subpopulation. Afterwards, a new extended SEIR (susceptible-exposed-infectious-recovered) epidemic model, which is referred to as an SEIAR (susceptible-exposed-symptomatic infectious-asymptomatic infectious-recovered) epidemic model with demography and disease mortality is given and focused on so as to extend the above developed ideas on the SIR model. -

Bibliographic Review on the Historical Memory of Previous
REVISIONES Bibliographic review on the historical memory of previous pandemics in nursing reviews on COVID-19: a secularly documented reality Revisión bibliográfica sobre la memoria histórica de pandemias anteriores en revisiones de enfermería sobre COVID-19: una realidad secularmente documentada Joaquín León Molina1 M. Fuensanta Hellín Gil1 Eva Abad Corpa2 1 Nurse Hospital Clínico Universitario Virgen de la Arrixaca de Murcia; Advanced Nursing Care Group of the Murcian Institute of Biosanitary Research Arrixaca. Murcia. Spain. 2 Associate nurse, Hospital General Universitario Reina Sofía de Murcia; Contracted Professor PhD linked University of Murcia. Advanced Nursing Care Group of the Murcian Institute of Biosanitary Research Arrixaca. Murcia. Spain. https://doi.org/10.6018/eglobal.456511 Received: 17/11/2020 Accepted: 10/01/2021 ABSTRACT: Introduction: Reviews for COVID-19 should reflect historical antecedents from previous pandemics. Objective: We plan to map the content of recent reviews in the nursing area on COVID-19 to see if it refers to health crises due to epidemics and infectious diseases. Methodology: Descriptive narrative review. The Science Web, PubMed and Lilacs were consulted to identify the reviews; The content of the documents was consulted to detect the presence of descriptors and terms related to pandemics prior to the 21st century of humanity, taking into account the inclusion criteria and objectives of the study. Results: Relevant reviews were found only in 11 documents of the 192 identified. Conclusions: There may be reluctance to use documentation published more than a century ago; However, it would be advisable not to lose the historical memory of pandemic crises that humanity has suffered for millennia Key words: Pandemics; Epidemics; History; Ancient History. -

Haitian Revolution Strategy
How to Win a War Without Even Shooting: Haitian Revolution Strategy Lynn Gourinski Fahr Overbrook High School Overview Rationale Objectives Strategies Classroom Activities Annotated Biographies/Works Cited/Resources Appendix/Content Standards Overview: The Haitian Revolution largely impacted world history albeit a small country. The war and the success of the enslaved peoples became the forerunner to modern anti- colonialism movements in the Third World and caused the world to pause and think. During the time of the Haitian Revolution (1791-1804), slaves outnumbered white slave owner’s 10:1.(Garrigus, 2006). The western Caribbean was alive with conquests and movement both socially and politically. It was also caught in a whirlwind of disease being brought from place to place-on ships and brought inland through the purchases of goods and slaves. Yellow Fever and Cholera wiped out thousands of persons in the Caribbean islands, many in just a few hours. But why was Haiti not as hard hit by cholera as other nations in the Caribbean. Why did Yellow Fever play such a pivotal role in the successful uprising of slaves? Many diseases might be prevented through good hygiene and development, while others were common to native peoples but wreaked havoc on troops employed to put down revolutions. Such was the case in Haiti, where of the 162,000 troops, up to 40,000 sent by Napoleon, were killed in attempts to reconquer the slaves and restore order in Haiti as Yellow Fever reared it's ugly head to kill many foreign invaders. (Peterson, 1995) Rationale: This curriculum can be taught in history classes for grades 7-12 in conjunction with a health class currently studying a universal hygiene unit. -

The Politics of the Coronavirus and Its Impact on International Relations
Vol. 14(3), pp. 116-125, July-September 2020 DOI: 10.5897/AJPSIR2020.1271 Article Number: FA1630564661 ISSN: 1996-0832 Copyright ©2020 African Journal of Political Science and Author(s) retain the copyright of this article http://www.academicjournals.org/AJPSIR International Relations Full Length Research Paper The politics of the coronavirus and its impact on international relations Bheki Richard Mngomezulu Department of Political Science, Faculty of Economic and Management Sciences, University of the Western Cape, South Africa. Received 7 June, 2020; Accepted 1 July, 2020 Pandemic outbreaks are not a new phenomenon globally. There is plethora of evidence to substantiate this view. However, each epidemic has its own defining features, magnitude, and discernible impact. Societies are affected differently. The coronavirus or COVID-19 is not an incongruity. Although it is still active, thus making detailed empirical data inconclusive, it has already impacted societies in many ways - leaving indelible marks. Regarding methodology, this paper is an analytic and exploratory desktop study which draws evidence from different countries to advance certain arguments. It is mainly grounded in political science (specifically international relations) and history academic disciplines. Firstly, the paper begins by looking at how the coronavirus has affected international relations – both positively and negatively. Secondly, using examples from different countries, it argues that the virus has exposed the political leadership by bringing to bear endemic socio-economic inequalities which result in citizens responding differently to government regulations meant to flatten the curve of infection. Thirdly, in the context of Africa, the paper makes a compelling argument that some of the socio-economic situations found within the continent are remnants of colonialism and apartheid. -

The Justinianic Plague's Origins and Consequences
The Justinianic plague’s origins and consequences Georgiana Bianca Constantin1, Ionuţ Căluian2 1Faculty of Medicine and Pharmacy, Dunarea de Jos University Galati, Romania 2Valahia University Targoviste, Romania Corresponding author: Georgiana Bianca Constantin Abstract The bubonic plague is an extremely old disease (apparentely from the late Neolitic era). The so-called “Justinianic plague”of the sixth century was the first well-attested outbreak of bubonic plague in the history of the Mediterranean world. It was thought that the Justinianic Plague, along with barbarian invasions, contributed directly to the so-called “Fall of the Roman Empire.” Keywords: plague, pandemics, history Introduction The bubonic plague is an extremely old disease, and scientists have detected the DNA of the pathogen that causes it—the bacterium Yersinia pestis—in the remains of late Neolithic era [1]. The limited details in historical texts have led scholars to question whether the causative agent of Justinianic Plague was truly Yersinia pestis, a debate that was only resolved recently through ancient DNA analysis [2-4]. Three major plague epidemics have been recorded worldwide so far: the “Justinian” plague in the 6th century, the “Black Death” in the 14th century and the recent 20th century pandemic [5]. The plague first hit cities in the southeastern Mediterranean, and moved swiftly through the Levant to the imperial capital of Constantinople. It seems that the plague arrived in Constantinople in 542 CE and the outbreak continued to sweep throughout the Mediterranean world for another 225 years, finally disappearing in 750 CE [1,6]. It is difficult to approximate the overall mortality rate due to the 542 plague, because of the lack of demographical data. -

A Comparative Evaluation Between the Impact of Previous Outbreaks and COVID-19 on the Tourism Industry Has Been Made Based on Statistics and Previous Research Studies
The current issue and full text archive of this journal is available on Emerald Insight at: https://www.emerald.com/insight/2516-8142.htm Impact of A comparative evaluation between COVID-19 on the impact of previous outbreaks the tourism and COVID-19 on the industry tourism industry Gulcin Ozbay, Mehmet Sariisik and Veli Ceylan Received 11 November 2020 Revised 9 January 2021 Gastronomy and Culinary Arts, Sakarya University of Applied Sciences, Accepted 10 January 2021 Sakarya, Turkey, and Muzaffer Çakmak Gastronomy and Culinary Arts, Istanbul_ Gelis¸im University, Istanbul, Turkey Abstract Purpose – The main purpose of this study is to make a comparative evaluation of the impacts of previous outbreaks and coronavirus disease 2019 (COVID-19) on the tourism industry. COVID-19 appears to have disrupted all memorizations about epidemics ever seen. Nobody has anticipated that the outbreak in late December will spread rapidly across the world, be fatal and turn the world economy upside down. Severe acute respiratory syndrome, Ebola, Middle East respiratory syndrome and others caused limited losses in a limited geography, thus similar behaviors were expected at first in COVID-19. But it was not so. Today, people continue to lose their lives and experience economic difficulties. One of the most important distressed industries is undoubtedly tourism. Design/methodology/approach – This study is a literature review. In this review, a comparative evaluation between the impact of previous outbreaks and COVID-19 on the tourism industry has been made based on statistics and previous research studies. Findings – The information and figures obtained show that COVID-19 and previous outbreaks have such significant differences that cannot be compared. -

Norovirus Background
DOH 420-180 Norovirus Background Clinical Syndrome of Norovirus Symptoms Norovirus can cause acute gastroenteritis in persons of all ages. Symptoms include acute onset non- bloody diarrhea, vomiting, nausea, and abdominal pain, sometimes accompanied by low-grade fever, body aches, and headache.2,3 Some individuals may only experience vomiting or diarrhea. Dehydration is a concerning secondary outcome.2 Symptoms typically resolve without treatment in 1-3 days in healthy individuals. Illness can last 4-6 days and may manifest more severely in young children elderly persons, and hospitalized patients.2,3 Diarrhea is more common in adults, while vomiting is more common among children.4 Up to 30% of norovirus infections are asymptomatic.2 Incubation The incubation period for norovirus is 12-48 hours.2 Transmission The only known reservoir for norovirus is humans. Transmission occurs by three routes: person-to- person, foodborne, or waterborne.2 Individuals can be infected by coming into contact with infected individuals (through the fecal-oral route or by ingestion of aerosolized vomitus or feces), contaminated foods or water, or contaminated surfaces or fomites.1,2 Viral shedding occurs for 4 weeks on average following infection, with peak viral shedding occurring 2-5 days after infection.2 Norovirus is extremely contagious, with an estimated infectious dose as low as 18 viral particles, indicating that even small amounts of feces can contain billions of infectious doses.2 The period of communicability includes the acute phase of illness up through 48 hours after conclusion of diarrhea. Treatment Treatment of norovirus gastroenteritis primarily includes oral rehydration through water, juice, or ice chips.