Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Top Tips How to Avoid Vector Borne Diseases (Eng)
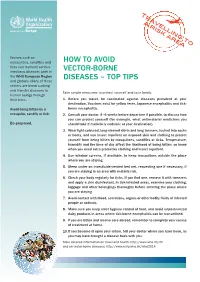
Tr a a v r e i ljl s k in a g r e to a Vectors such as mosquitoes, sandflies and HOW tO AvOid ticks can transmit serious infectious diseases both in vEctOR-BORnE the WHO European Region disEAsEs – tOp tips and globally. Many of these vectors are blood sucking and transfer diseases to Take simple measures to protect yourself and your family. human beings through their bites. 1. Before you travel, be vaccinated against diseases prevalent at your destination. vaccines exist for yellow fever, Japanese encephalitis and tick- Avoid being bitten by a borne encephalitis. mosquito, sandfly or tick. 2. consult your doctor, 4–6 weeks before departure if possible, to discuss how you can protect yourself (for example, what antimalarial medicines you Be prepared. should take if malaria is endemic at your destination). 3. Wear light-coloured, long-sleeved shirts and long trousers, tucked into socks or boots, and use insect repellent on exposed skin and clothing to protect yourself from being bitten by mosquitoes, sandflies or ticks. temperature, humidity and the time of day affect the likelihood of being bitten, so know when you need extra protective clothing and insect repellent. 4. Use window screens, if available, to keep mosquitoes outside the place where you are staying. 5. sleep under an insecticide-treated bed net, requesting one if necessary, if you are staying in an area with malaria risk. 6. check your body regularly for ticks. if you find one, remove it with tweezers and apply a skin disinfectant. in tick-infested areas, examine your clothing, luggage and other belongings thoroughly before entering the place where you are staying. -

Guide Yellow Fever Outbreak 2016
© World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

Evaluation of the Diagnostic Value of the Tourniquet Test in Predicting Severe Dengue Cases in a Population from Belo Horizonte, State of Minas Gerais, Brazil
Revista da Sociedade Brasileira de Medicina Tropical 46(5):542-546, Sep-Oct, 2013 Major Article http://dx.doi.org/10.1590/0037-8682-0161-2013 Evaluation of the diagnostic value of the tourniquet test in predicting severe dengue cases in a population from Belo Horizonte, State of Minas Gerais, Brazil Alice Costa Antunes[1], Geancarlo Laporte Oliveira[1], Leidiane Ileila Nunes[1], Luiz Alberto Guedes Filho[1], Rafael Santos Prado[1], Hugo Rezende Henriques[2] and Aristides José Carvalho Vieira[3] [1]. Curso de Medicina, Faculdade da Saúde e Ecologia Humana, Vespasiano, MG. [2]. Departamento de Parasitologia, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, SP. [3]. Departamento de Medicina Social e Preventiva, Faculdade da Saúde e Ecologia Humana, Vespasiano, MG. ABSTRACT Introduction: Dengue is prevalent in many tropical and sub-tropical regions. The clinical diagnosis of dengue is still complex, and not much data are available. This work aimed at assessing the diagnostic accuracy of the tourniquet test in patients with suspected dengue infection and its positivity in different classifi cations of this disease as reported to the Information System for Notifi able Disease in Belo Horizonte, State of Minas Gerais, Brazil between 2001 and 2006. Methods: Cross-section analysis of the diagnostic accuracy of the tourniquet test for dengue, using IgM-anti-DENV ELISA as a gold standard. Results: We selected 9,836 suspected cases, of which 41.1% were confi rmed to be dengue. Classic dengue was present in 95.8%, dengue with complications in 2.5% and dengue hemorrhagic fever in 1.7%. -

How Can We Use Genetic Engineering to Get Rid of Malaria for Good?
DECEMBERMARCH 20172020 How can we use genetic engineering to get rid of malaria for good? Authors: Susan Crow, Meghan Pawlowski, Manyowa Meki, LaraAuthors: LaDage, Timothy Roth II, Cynthia Downs, BarryKyros SinervoKyrou, Andrew and Vladimir Hammond, Pravosudov Andrea Crisanti & others Associate Editors: LindseySeda Dawson Hall and and Gogi Madeleine Kalka Corcoran Abstract Nobody likes the buzzing sound or itchy bite of mosquitoes. What if we used genetic engineering? Here we modified But mosquito bites (only females bite, by the way!) are not the genetic makeup of Anopheles gambiae mosquitoes (the just irritating: they can carry and spread deadly diseases main carriers of malaria). The mutation prevented females such as malaria, dengue, yellow fever and many more. Every from biting and laying eggs. It spread through our caged year, millions of people die from mosquito-borne diseases and populations quickly and drove them extinct. Our results pave most of them are young children. There are ways to get rid the way for lowering mosquito populations in the wild and of mosquitoes and prevent such diseases, but they are not as getting rid of malaria in the future. effective as we would like. EDITING GENES WITH CRISPR A tool used by scientists to precisely edit genes inside cells. Introduction It consists of two parts… Cas9 Guide RNA (An enzyme that (Directs the Cas9 You may have heard about malaria and the devastation it cuts DNA) + to the target DNA) causes in Africa. But did you know that a child dies of malaria every two minutes? Despite global efforts, malaria remains one of the world’s deadliest diseases. -

Specificity of Hess Test As a Marker of DHF
Original Article Specificity of Hess Test as a Marker of DHF Somia Iqtadar,1 Sami Ullah Mumtaz,2 Sajid Abaidullah,3 Razia Amanat,4 Mohsin Masud5 Abstract 4 groups, patients with only rash, only bleeding, bleed- ing and rash together and Non-bleeding Non-rash. Out Objectives: Dengue Fever is a public problem in most of 09 patients of rash Hess test was positive in only 06 of the tropical countries of South – East Asia. DHF is patients (67.7%). In bleedingonly group Hess test was a serious form of Dengue Infection, diagnosed on the positive in 06 out of 11 patients (54.5%). Similarly in basis of demonstrating an increased capillary permea- bleeding n rash simultaneously Hess test was positive bility and thrombocytopenia with concurrent haemo- in 06 out of 07 patients (85.7%). In non bleeding non concentration. Hess test or Tourniquet test has been rash group Hess test was positive in 08 out of 23 pati- recommended as the initial screening procedure of pat- ents (34.8%). ients with suspected DHF. The objective of the present study was tosee thespecificity of Hess test as a marker Conclusion: The tourniquet test was positive in only of DHF. 52% of all DHF cases. It is concluded that a positive Hess test is a good marker of DHF but negative tourni- Methods: In a total of 50 patients of DHF admitted to quet test may not be sufficient to exclude a diagnosis the Mayo hospital Lahore from September to October of DHF in a febrile patient. This necessitates the need 2011 during outbreak of Dengue Infection, were pros- for the re-defining the clinical criteria for the diagnosis pectively studied. -

How Can We Use Genetic Engineering to Get Rid of Malaria for Good? Teacher’S Key
How can we use genetic engineering to get rid of malaria for good? TEACher’s key Check your understanding 1 Anopheles gambiae mosquitoes are a vector species for malaria. What is a vector species? Can you find out about some other vector species and the diseases they transmit? A vector is an organism that does not cause disease itself but which spreads infection by transmitting pathogens (virus, bacteria, parasites, etc.) from one host to another. Mosquitoes are vector species of many infectious diseases including malaria, dengue, yellow fever, Zika, and West Nile virus. Some other vector species are ticks (Lyme Answer disease), fleas (bubonic plague), raccoons, bats, foxes, skunks (rabies). Scientists genetically engineered Anopheles gambiae mosquitoes. What were the characteristics of engineered 2 mosquitoes that drove the lab populations to extinction? Male mosquitoes with one or both copies of the mutated gene had no physical differences but they were carriers of the mutated gene and passed it onto their offspring. Female mosquitoes with one copy of the mutated gene were healthy but they had reduced fertility. They passed the mutated gene on to the next generation. Females with two copies of the mutated gene had male body parts (a mouth that is not structured to bite, claspers, and hairy Answer antennae). Most importantly, they were infertile - they couldn’t lay eggs. So once all females carried two copies of the mutated gene, the population collapsed. 3 Scientists used a new approach that made this study so successful at wiping out mosquito populations: CRISPR/Cas9 gene drive. What is the purpose of a gene drive? How does it speed up the spread of a useful genetic mutation? In sexual reproduction, half of the genes come from the male organism and the other half come from the female organism. -

The Phenomenon of External Pressure Rumpel Leede Sign: a Review
Chris Elizabeth Vinod et al /J. Pharm. Sci. & Res. Vol. 12(3), 2020, 433-435 The Phenomenon of External Pressure Rumpel Leede Sign: A Review Chris Elizabeth Vinod1, Shruthi Jaya Saju1, Khayati Moudgil* Department of Pharmacy Practice, JSS College of Pharmacy, Ooty, India. JSS Academy of Higher Education and Research. Abstract Rumpel leede sign (RLS) is a clinical presentation observed at the extremities due to pressure applied externally. The appearance ranges from scattered pin-point rashes to an entire arm covered with petechial hemorrhage depending upon the severity. This condition occurs mainly due to fragility of the capillaries which in turn is caused by underlying conditions like hypertension, diabetes mellitus, infections caused by certain organisms, drug-induced RLS etc. When a patient with such condition experiences an external pressure i.e, application of a tourniquet, sphygmomanometer cuff inflation, the region distal to the applied pressure displays the sign. It’s most commonly seen in elderly patients and sometimes appears on the thighs of babies when the baby carrier straps are too tight. This phenomenon is self-limiting and thus does not require additional treatment. It resolves within a period of hours to days, sometimes weeks depending on how severe is the presentation. The RLS is also used as one of the diagnostic criteria to identify disease conditions like dengue. Keywords: Pressure; Capillaries; Pin-point; Severity INTRODUCTION AND BACKGROUND Danlos syndrome, thrombocytopenia and therefore it is not Rumpel Leede (R-L) sign is a rare occurrence where particular to diabetes (4,5,6). petechial rashes are observed due to an external pressure. -

Specificity of Hess Test As a Marker of DHF Iqtadar S , Mumtaz SU
Specificity of Hess test as a marker of DHF Iqtadar S , Mumtaz SU , Abaidullah S , Amanat R, Masud M North Medical Ward, King Edward Medical university Mayo Hospital Lahore,Pakistan. OBJECTIVES: Dengue Fever is a public problem in most of the tropical countries of South-East Asia. DHF is a serious form of Dengue Infection, diagnosed on the basis of demonstrating an increased capillary permeability and thrombocytopenia with concurrent haemo-concentration. Hess test or Tourniquet test has been recommended as the initial screening procedure of patients with suspected DHF. The objective of the present study was to see the specificity of Hess test as a marker of DHF. METHODS: 50 patients of DHF admitted to the Mayo hospital Lahore from September to October 2011 during outbreak of Dengue Infection, were prospectively studied. Hess test or tourniquet test was conducted in these cases in the standard method. RESULTS: Out of the 50 patients of DHF, only 26 were Hess test positive. These 50 patients were divided into 4 groups, patients with only rash, only bleeding, bleeding & rash together & Non- bleeding Non-rash. Out of 09 patients of rash Hess test was positive in only 06 patients (67.7 %). In bleeding only group Hess test was positive in 06 out of 11 patients (54.5 %). Similarly in bleeding and rash simultaneously Hess test was positive in 06 out of 07 patients (85.7 %). In non bleeding non rash group Hess test was positive in 08 out of 23 patients (34.8%). CONCLUSION: The tourniquet test was positive in only 52% of all DHF cases. -

Rumpel-Leede Phenomenon in a Hypertensive Patient Due to Mechanical Trauma: a Case Report Adam Hartley1*, Phang B
Hartley et al. Journal of Medical Case Reports (2016) 10:150 DOI 10.1186/s13256-016-0950-3 CASEREPORT Open Access Rumpel-Leede phenomenon in a hypertensive patient due to mechanical trauma: a case report Adam Hartley1*, Phang B. Lim1 and Sajad A. Hayat2 Abstract Background: In this report, we present an interesting case of a patient with Rumpel-Leede phenomenon, a rare occurrence that can result in significant delays in medical treatment. This phenomenon is characterized by the presence of a petechial rash that results from acute dermal capillary rupture. In our patient, it occurred secondary to raised pressure in the dermal vessels caused by repeated inflation of a sphygmomanometer cuff. Contributory factors in Rumpel-Leede phenomenon include prevalent conditions such as diabetes mellitus, hypertension, thrombocytopenia, chronic steroid use, antiplatelets, and anticoagulants. Case presentation: A 58-year-old Russian woman with diabetes and hypertension presented to our hospital with a non-ST elevation myocardial infarction, and she subsequently developed a petechial rash on her distal upper limbs. A vasculitic screen was performed, with normal results. Conclusions: Given the timing and distribution of the rash, it was felt that this was an example of Rumpel-Leede phenomenon in a susceptible individual. This is an important diagnosis to be aware of in patients with vascular risk factors presenting for acute medical care who subsequently develop a petechial rash. Keywords: Diabetes mellitus, Mechanical trauma, Petechial rash, Rumpel-Leede phenomenon Background diabetes mellitus, myocardial infarction, atrial fibrillation Rumpel-Leede sign was first reported in 1909 by Theo- on warfarin, heart failure, and stage 4 chronic kidney dor Rumpel and again in 1911 by Carl Stockbridge disease. -
What Is Barmah Forest Virus?
What is Barmah Forest Virus? Barmah Forest Virus is a viral disease that is transmitted to humans through mosquito bites. People with mild cases usually recover in a month or so, but symptoms may persist for longer. What are the symptoms of Barmah Forest Virus? The illness often begins with mild ’flu-like symptoms. Arthritis in large and small joints, joint stiffness and swelling, fever, lethargy, fatigue, headache, night sweats, nausea, muscle tenderness and pain, dizziness and light-headedness—any of these may be present, with or without a prominent rash. Joint pain and fatigue may last up to 6 months. The condition is very similar to Ross River Virus infection, although generally of shorter duration. Who can get Barmah Forest Virus? The infection is unique to Australia where anyone bitten by certain mosquitoes is at risk of acquiring it. Infections tend to be more common in northern Australia and among people aged 35 to 65. Cases occur mainly in the warmer months, a time of peak mosquito activity. What is the incubation period for Barmah Forest Virus? Usually 7–9 days from the bite to the development of symptoms. How long is a person infectious? Immunity develops after initial infection, but there may be a very short period of time when a mosquito can pick up the virus from one person and transfer it to another, or to an animal. How is Barmah Forest Virus transmitted? A mosquito that bites an infected animal or infected person transmits the virus by biting another person or animal. It cannot be passed directly from person to person. -

Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control -- New Edition
DENGUE GUIDELINES FOR DIAGNOSIS, TREATMENT, PREVENTION AND CONTROL New edition DENGUE GUIDELINES FOR DIAGNOSIS, TREATMENT, DENGUE GUIDELINES FOR DIAGNOSIS, TREATMENT, PREVENTION AND CONTROL New edition 2009 Neglected Tropical Diseases (NTD) TDR/World Health Organization HIV/AIDS, Tuberculosis and Malaria (HTM) 20, Avenue Appia World Health Organization 1211 Geneva 27 Avenue Appia 20, 1211 Geneva 27, Switzerland Switzerland Fax: +41 22 791 48 69 Fax: +41 22 791 48 54 www.who.int/neglected_diseases/en www.who.int/tdr [email protected] [email protected] DENGUE GUIDELINES FOR DIAGNOSIS, TREATMENT, PREVENTION AND CONTROL New edition 2009 A joint publication of the World Health Organization (WHO) and the Special Programme for Research and Training in Tropical Diseases (TDR) WHO Library Cataloguing-in-Publication Data Dengue: guidelines for diagnosis, treatment, prevention and control -- New edition. 1.Dengue - diagnosis. 2.Dengue - therapy. 3.Dengue - prevention and control. 4.Endemic Diseases - prevention and control. 5.Fluid therapy. 6.Diagnosis, differential. 7.Disease outbreaks - prevention and control. 8.Mosquito control. 9.Guidelines. I.World Health Organization. ISBN 978 92 4 154787 1 (NLM classification: WC 528) WHO/HTM/NTD/DEN/2009.1 Expiry date: 2014 © World Health Organization 2009 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). -

MOSQUITOES & THEIR C ONTROL Integrated Pest Management for Mosquito Reduction Around Homes and Neighborhoods
SP 498 MOSQUITOES & THEIR CONTROL Integrated Pest Management for Mosquito Reduction Around Homes and Neighborhoods United States National Institute Department of of Food and Agriculture Agriculture Mosquitoes & Their Control Integrated Pest Management for Mosquito Reduction Around Homes and Neighborhoods E. Buckner, C. R. Connelly, E. Bolles, D. Culbert, J. DeValerio, M. Donahoe, K. Gabel, R. Jordi, J. McLaughlin, A. Neal, S. Scalera, E. Toro, and J. Walter © Copyright 2019 by University of Florida, Institute of Food and Agricultural Sciences ISBN: 978-1-949197-06-8 Printed in the United States of America. All rights reserved. Parts of this publication may be reproduced for educational purposes only. Please provide credit to “University of Florida, Institute of Food and Agricultural Sciences,” accompanied by the published date. Contributors E. Buckner, Florida Medical Entomology Laboratory (FMEL) Research and Education Center, Vero Beach, FL 32962 E. Bolles, UF/IFAS Extension Escambia County, Cantonment, FL 32533 C.R. Connelly, Centers for Disease Control and Prevention, Division of Vector-Borne Diseases, Ft. Collins, CO 80521 D. Culbert, UF/IFAS Extension Okeechobee County, Okeechobee, FL 34972 J. DeValerio, UF/IFAS Extension Bradford County, Starke, FL 32091 M. Donahoe, UF/IFAS Extension Santa Rosa County, Milton, FL 32570 K. Gabel, UF/IFAS Extension Monroe County, Key West, FL 33040 R. Jordi, UF/IFAS Extension Nassau County, Callahan, FL 32011 J. McLaughlin, UF/IFAS Extension Miami-Dade, Department of Regulatory and Economic Resources, Miami-Dade County, Miami, FL 33030 A. Neal, UF/IFAS Extension St. Lucie County, Fort Pierce, FL 34981 S. Scalera, UF/IFAS Extension Brevard County, Cocoa, FL 32926 E.