WEST NILE VIRUS ABOUT ASM Faqs STEERING COMMITTEE: Michael Gale, Ph.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Everything You Always Wanted to Know About Rabies Virus ♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣♣ (But Were Afraid to Ask) Benjamin M
ANNUAL REVIEWS Further Click here to view this article's online features: t%PXOMPBEmHVSFTBT115TMJEFT t/BWJHBUFMJOLFESFGFSFODFT t%PXOMPBEDJUBUJPOT Everything You Always Wanted t&YQMPSFSFMBUFEBSUJDMFT t4FBSDILFZXPSET to Know About Rabies Virus (But Were Afraid to Ask) Benjamin M. Davis,1 Glenn F. Rall,2 and Matthias J. Schnell1,2,3 1Department of Microbiology and Immunology and 3Jefferson Vaccine Center, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania, 19107; email: [email protected] 2Fox Chase Cancer Center, Philadelphia, Pennsylvania 19111 Annu. Rev. Virol. 2015. 2:451–71 Keywords First published online as a Review in Advance on rabies virus, lyssaviruses, neurotropic virus, neuroinvasive virus, viral June 24, 2015 transport The Annual Review of Virology is online at virology.annualreviews.org Abstract This article’s doi: The cultural impact of rabies, the fatal neurological disease caused by in- 10.1146/annurev-virology-100114-055157 fection with rabies virus, registers throughout recorded history. Although Copyright c 2015 by Annual Reviews. ⃝ rabies has been the subject of large-scale public health interventions, chiefly All rights reserved through vaccination efforts, the disease continues to take the lives of about 40,000–70,000 people per year, roughly 40% of whom are children. Most of Access provided by Thomas Jefferson University on 11/13/15. For personal use only. Annual Review of Virology 2015.2:451-471. Downloaded from www.annualreviews.org these deaths occur in resource-poor countries, where lack of infrastructure prevents timely reporting and postexposure prophylaxis and the ubiquity of domestic and wild animal hosts makes eradication unlikely. Moreover, al- though the disease is rarer than other human infections such as influenza, the prognosis following a bite from a rabid animal is poor: There is cur- rently no effective treatment that will save the life of a symptomatic rabies patient. -

Progressive Multifocal Leukoencephalopathy and the Spectrum of JC Virus-Related Disease
REVIEWS Progressive multifocal leukoencephalopathy and the spectrum of JC virus- related disease Irene Cortese 1 ✉ , Daniel S. Reich 2 and Avindra Nath3 Abstract | Progressive multifocal leukoencephalopathy (PML) is a devastating CNS infection caused by JC virus (JCV), a polyomavirus that commonly establishes persistent, asymptomatic infection in the general population. Emerging evidence that PML can be ameliorated with novel immunotherapeutic approaches calls for reassessment of PML pathophysiology and clinical course. PML results from JCV reactivation in the setting of impaired cellular immunity, and no antiviral therapies are available, so survival depends on reversal of the underlying immunosuppression. Antiretroviral therapies greatly reduce the risk of HIV-related PML, but many modern treatments for cancers, organ transplantation and chronic inflammatory disease cause immunosuppression that can be difficult to reverse. These treatments — most notably natalizumab for multiple sclerosis — have led to a surge of iatrogenic PML. The spectrum of presentations of JCV- related disease has evolved over time and may challenge current diagnostic criteria. Immunotherapeutic interventions, such as use of checkpoint inhibitors and adoptive T cell transfer, have shown promise but caution is needed in the management of immune reconstitution inflammatory syndrome, an exuberant immune response that can contribute to morbidity and death. Many people who survive PML are left with neurological sequelae and some with persistent, low-level viral replication in the CNS. As the number of people who survive PML increases, this lack of viral clearance could create challenges in the subsequent management of some underlying diseases. Progressive multifocal leukoencephalopathy (PML) is for multiple sclerosis. Taken together, HIV, lymphopro- a rare, debilitating and often fatal disease of the CNS liferative disease and multiple sclerosis account for the caused by JC virus (JCV). -

Congenital Cytomegalovirus Infection Alters Olfaction Before Hearing Deterioration in Mice
10424 • The Journal of Neuroscience, December 5, 2018 • 38(49):10424–10437 Development/Plasticity/Repair Congenital Cytomegalovirus Infection Alters Olfaction Before Hearing Deterioration In Mice X Franc¸oise Lazarini,1,2 Lida Katsimpardi,1,2* Sarah Levivien,1,2,3*Se´bastien Wagner,1,2 XPierre Gressens,3,4,5 Natacha Teissier,3,4,6† and Pierre-Marie Lledo1,2† 1Institut Pasteur, Perception and Memory Unit, F-75015 Paris, France, 2Centre National de la Recherche Scientifique, Unite´ Mixte de Recherche 3571, F-75015 Paris, France, 3PROTECT, INSERM, Unite´ 1141, F-75019 Paris, France, 4Paris Diderot University, Sorbonne Paris Cite´, F-75018 Paris, France, 5Center for Developing Brain, King’s College, London, WC2R2LS United Kingdom, and 6Pediatric Otorhinolaryngology Department, Robert Debre´ Hospital, Assistance Publique–Hoˆpitaux de Paris, F-75019 Paris, France In developed countries, cytomegalovirus (CMV)-infected newborns are at high risk of developing sensorineural handicaps such as hearing loss, requiring extensive follow-up. However, early prognostic tools for auditory damage in children are not yet available. In the fetus, CMV infection leads to early olfactory bulb (OB) damage, suggesting that olfaction might represent a valuable prognosis for neurological outcome of this viral infection. Here, we demonstrate that in utero CMV inoculation causes fetal infection and growth retardation in mice of both sexes. It disrupts OB normal development, leading to disproportionate OB cell layers and rapid major olfactory deficits. Olfaction is impaired as early as day 6 after birth in both sexes, long before the emergence of auditory deficits. Olfactometry in males reveals a long-lasting alteration in olfactory perception and discrimination, particularly in binary mixtures of monomolecular odorants. -
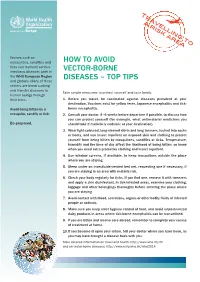
Top Tips How to Avoid Vector Borne Diseases (Eng)
Tr a a v r e i ljl s k in a g r e to a Vectors such as mosquitoes, sandflies and HOW tO AvOid ticks can transmit serious infectious diseases both in vEctOR-BORnE the WHO European Region disEAsEs – tOp tips and globally. Many of these vectors are blood sucking and transfer diseases to Take simple measures to protect yourself and your family. human beings through their bites. 1. Before you travel, be vaccinated against diseases prevalent at your destination. vaccines exist for yellow fever, Japanese encephalitis and tick- Avoid being bitten by a borne encephalitis. mosquito, sandfly or tick. 2. consult your doctor, 4–6 weeks before departure if possible, to discuss how you can protect yourself (for example, what antimalarial medicines you Be prepared. should take if malaria is endemic at your destination). 3. Wear light-coloured, long-sleeved shirts and long trousers, tucked into socks or boots, and use insect repellent on exposed skin and clothing to protect yourself from being bitten by mosquitoes, sandflies or ticks. temperature, humidity and the time of day affect the likelihood of being bitten, so know when you need extra protective clothing and insect repellent. 4. Use window screens, if available, to keep mosquitoes outside the place where you are staying. 5. sleep under an insecticide-treated bed net, requesting one if necessary, if you are staying in an area with malaria risk. 6. check your body regularly for ticks. if you find one, remove it with tweezers and apply a skin disinfectant. in tick-infested areas, examine your clothing, luggage and other belongings thoroughly before entering the place where you are staying. -

The Role of Herpes Simplex Virus Type 1 Infection in Demyelination of the Central Nervous System
International Journal of Molecular Sciences Review The Role of Herpes Simplex Virus Type 1 Infection in Demyelination of the Central Nervous System Raquel Bello-Morales 1,2,* , Sabina Andreu 1,2 and José Antonio López-Guerrero 1,2 1 Departamento de Biología Molecular, Universidad Autónoma de Madrid, Cantoblanco, 28049 Madrid, Spain; [email protected] (S.A.); [email protected] (J.A.L.-G.) 2 Centro de Biología Molecular Severo Ochoa, CSIC-UAM, Cantoblanco, 28049 Madrid, Spain * Correspondence: [email protected] Received: 30 June 2020; Accepted: 15 July 2020; Published: 16 July 2020 Abstract: Herpes simplex type 1 (HSV-1) is a neurotropic virus that infects the peripheral and central nervous systems. After primary infection in epithelial cells, HSV-1 spreads retrogradely to the peripheral nervous system (PNS), where it establishes a latent infection in the trigeminal ganglia (TG). The virus can reactivate from the latent state, traveling anterogradely along the axon and replicating in the local surrounding tissue. Occasionally, HSV-1 may spread trans-synaptically from the TG to the brainstem, from where it may disseminate to higher areas of the central nervous system (CNS). It is not completely understood how HSV-1 reaches the CNS, although the most accepted idea is retrograde transport through the trigeminal or olfactory tracts. Once in the CNS, HSV-1 may induce demyelination, either as a direct trigger or as a risk factor, modulating processes such as remyelination, regulation of endogenous retroviruses, or molecular mimicry. In this review, we describe the current knowledge about the involvement of HSV-1 in demyelination, describing the pathways used by this herpesvirus to spread throughout the CNS and discussing the data that suggest its implication in demyelinating processes. -

Intrathecal Antibody Production Against Epstein-Barr, Herpes Simplex, and Other Neurotropic Viruses in Autoimmune Encephalitis
ARTICLE OPEN ACCESS Intrathecal Antibody Production Against Epstein-Barr, Herpes Simplex, and Other Neurotropic Viruses in Autoimmune Encephalitis Philipp Schwenkenbecher, MD, Thomas Skripuletz, MD, Peter Lange, Marc Durr,¨ MD, Felix F. Konen, MD, Correspondence Nora Mohn,¨ MD, Marius Ringelstein, MD, Til Menge, MD, Manuel A. Friese, MD, Nico Melzer, MD, Dr. Schwenkenbecher schwenkenbecher.philipp@ ¨ Michael P. Malter, MD, Martin Hausler, MD, Franziska S. Thaler, MD, Martin Stangel, MD, Jan Lewerenz, MD, mh-hannover.de and Kurt-Wolfram Suhs,¨ MD, on behalf of the German Network for Research on Autoimmune Encephalitis Neurol Neuroimmunol Neuroinflamm 2021;8:e1062. doi:10.1212/NXI.0000000000001062 Abstract Background and Objectives Neurotropic viruses are suspected to play a role in the pathogenesis of autoimmune diseases of the CNS such as the association between the Epstein-Barr virus (EBV) and multiple sclerosis (MS). A group of autoimmune encephalitis (AE) is linked to antibodies against neuronal cell surface proteins. Because CNS infection with the herpes simplex virus can trigger anti–NMDA receptor (NMDAR) encephalitis, a similar mechanism for EBV and other neurotropic viruses could be postulated. To investigate for previous viral infections of the CNS, intrathecally produced virus-specific antibody synthesis was determined in patients with AE. Methods Antibody-specific indices (AIs) against EBV and measles, rubella, varicella zoster, herpes simplex virus, and cytomegalovirus were determined in 27 patients having AE (anti-NMDAR encephalitis, n = 21, and LGI1 encephalitis, n = 6) and in 2 control groups comprising of 30 patients with MS and 21 patients with noninflammatory CNS diseases (NIND), which were sex and age matched. Results An intrathecal synthesis of antibodies against EBV was found in 5/27 (19%) patients with AE and 2/30 (7%) of the patients with MS. -
Comprehensive Guidelines for Prevention and Control of Dengue and Dengue Haemorrhagic Fever
C o m p r e h e n s Dengue fever (DF) is the fastest emerging arboviral infection spread by Aedes aegypti i v mosquitoes with major public health consequences for millions of people around the e G world, and in particular the South-East Asia and Asia-Pacific Regions of the World u i Health Organization (WHO). Of the 2.5 billion people globally at risk of DF and its d e severe forms dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS) l i n South-East Asia accounts for approximately 1.3 billion or 52%. e s f As the disease spreads to new geographical areas, the frequency of the o r outbreaks has increased along with a rapidly changing disease epidemiology. In P r response to resolution of the Forty-sixth World Health Assembly urging Member e v States to strengthen national programmes for control of DF/DHF, several documents e n were developed by regional offices of WHO, including South-East Asia. t i o In 1999 the WHO Regional Office for South-East Asia published the Regional n a Comprehensive Guidelines for Guidelines for the Prevention and Control of DF/DHF. Since then new strategies and n d developments in the control of dengue fever, DHF and DSS have come to light. The C Regional Guidelines were extensively revised, updated and expanded with the focus o n Prevention and Control of on new and additional topics of current relevance to the populations of Member t r o States of the Region. They were then rechristened the Comprehensive Guidelines for l o the Prevention and Control of Dengue and Dengue Haemmorhagic Fever. -

Neurotropic Viral Infections in Bangladesh: Burden and Challenges
http://www.banglajol.info/index.php/BJID/index Editorial Bangladesh Journal of Infectious Diseases June 2016, Volume 3, Number 1 ISSN (Online) 2411-670X ISSN (Print) 2411-4820 Neurotropic Viral Infections in Bangladesh: Burden and Challenges Mohammad Enayet Hussain Assistant Professor, Department of Neurology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh; Email: [email protected] Neurotropic virus infections continue to cause encephalopathies. In addition, influenza viruses major disease and economic burdens on society1. It have been linked to the development of Guillan poses a major challenge to human health care Barré syndrome, Kleine Levin syndrome and systems due to the associated morbidity and transfer myelitis5. Maternal influenza has been mortality worldwide. This creates a unique problem associated with schizophrenia and bipolar disorder in providing treatment to the patients involved. This (BD) in the offspring. Acute demyelinating is largely due to unique features of the central encephalomyelitis (ADME) typically occurs in nervous system (CNS), with a plethora of measles patients. Subacute sclerosing interconnected and interdependent cell types, panencephalitis (SSPE) occurs on average 4– complex structures and functions, reduced immune 10 years following acute MV infection. Mumps surveillance and limited regeneration capacity. virus was the leading cause of aseptic meningitis in Infection by neurotropic viruses as well as the local the pre-vaccine era. Pathologically, mumps induced immune responses can -

Cns Response in a Rabid Brain: a Pathological View
Review Article ISSN 2250-0480 VOL 5/ ISSUE 4/OCT 2015 CNS RESPONSE IN A RABID BRAIN: A PATHOLOGICAL VIEW 1PREETY SHARMA, 1 SANJEEV KUMAR,2 V. K. SHARMA* & AJAY KUMAR TEHLAN 1Central Research Institute, Kasauli, District Solan, Himachal Pradesh -173204, India. 2Department of Pharmacology, Govt. College of Pharmacy, Rohru, Distt. Shimla, Himachal Pradesh-171207, India ABSTRACT Animal attacks constitute a huge medical and social problem ending in millions of injuries and thousands of deaths worldwide. Rabies is a dreadful infectious disease that has not been brought under control in many parts of the world even today. Rabies spread by domestic and wild animals particularly by a dog bite, and with the exception of Antarctica, rabies is present on all continents, taking a heavy toll on human lives. Many countries have the status of high-risk areas, but most of the countries around the globe gained the status of rabies free territories. This shows that rabies can be successfully ruled out from the high-risk areas by taking preventing measures and the situation may be better if we continue to untangle the mysterious pathophysiology of this disease. Understanding rabies invasion and its pathophysiology will further enhance the chances of improvement rabies related complications and mortality. Rabies is a prototypic infection of the nervous system in which the virus selectively infects neurons, using retrograde axonal transport to traffic in the nervous system. Neuroinvasiveness, neurotropism and neurovirulence are the major defining characteristics of this virus. The speed of virus uptake, the ability of the virus to spread efficiently from cell-to-cell and the rate of virus replication are the major factors that determine the pathogenicity of rabies virus. -

Guide Yellow Fever Outbreak 2016
© World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

คาศัพท์เฉพาะทางด้านการแพทย์ในหมวด Neurotropic Virus
รายงาน ค าศัพท์เฉพาะทางด้านการแพทย์ในหมวด Neurotropic virus Virus ที่มีผลต่อ Cell neuron จัดท าโดย 1. นสพ. กฤตภาส กิจสนาโยธิน รหัสนิสิต 58460042 2. นสพ. จารุกิตติ์ อุบลสะอาด รหัสนิสิต 58460127 3. นสพ. ชนิกานต์ เดชขุนทด รหัสนิสิต 58460189 4. นสพ. พงศ์ศิริ บัวนุ่ม รหัสนิสิต 58460431 5. นสพ. พิมพ์ประไพ ศิลากุล รหัสนิสิต 58460516 6. นสพ. เพ็ญพิชญา มาราช รหัสนิสิต 58460547 7. นสพ. ภัทราวดี เดือนเพ็ญ รหัสนิสิต 58460585 8. นสพ. ภูดิศญา ตั้งวรสิทธิชัย รหัสนิสิต 58460608 9. นสพ. สุชาดา วิเศษกุลพรหม รหัสนิสิต 58460820 10. นสพ. ธนกฤต อนันตจันทรา รหัสนิสิต 58461025 นิสิตแพทย์ชั้นปีที่ 2 กลุ่มที่ 2 เสนอ ผู้ช่วยศาสตราจารย์ นายแพทย์ ดร. ณตพล ศุภณัฐเศรษฐกุล รายงานนี้เป็นส่วนหนึ่งของวิชา 499721 ค าศัพท์เฉพาะทางด้านการแพทย์ คณะแพทยศาสตร์ มหาวิทยาลัยนเรศวร ภาคเรียนที่ 1 ปีการศึกษา 2559 ก ค ำน ำ รายงานฉบับนี้เป็นส่วนหนึ่งของรายวิชาค าศัพท์เฉพาะทางด้านการแพทย์ 499721 โดยมี จุดประสงค์ เพื่อศึกษาค าศัพท์เฉพาะทางการแพทย์ในหมวดขอกลุ่ม Neurotropic virus Virus ที่ มีผลต่อ Cell neuron ซึ่งรายงานนี้มีเนื้อหาเกี่ยวกับไวรัสชนิดต่างๆที่มีผลต่อ cell neuron จ านวน 10 ชนิด โดยศึกษาถึงวิธีการออกเสียง ชนิดของค าศัพท์ ที่มาของค าศัพท์ ความหมายของ ค าศัพท์และศัพท์บัญญัติในภาษาไทย นอกจากนั้นยังมีรายละเอียดเพิ่มเติมเกี่ยวกับไวรัสชนิดนั้นๆ รวมถึงรูปภาพประกอบเพื่อเสริมความเข้าใจอีกด้วย ผู้จัดท าได้เลือกหัวข้อนี้ในการท ารายงาน เนื่องมาจากเป็นเรื่องที่น่าสนใจ รวมถึงเป็นเรื่องที่ ค่อนข้างแปลกใหม่ ผู้จัดท าจะต้องขอขอบคุณ ผู้ช่วยศาสตราจารย์ นายแพทย์ ดร. ณตพล ศุภณัฐเศรษฐกุล ผู้ให้ความรู้ และแนวทางการศึกษารวมถึง อ.พญ.สาธิณี ชูเชิด อาจารย์ผู้ช่วยใน รายวิชานี้ที่คอยให้ค าแนะน าในเรื่องต่าง -

How Can We Use Genetic Engineering to Get Rid of Malaria for Good?
DECEMBERMARCH 20172020 How can we use genetic engineering to get rid of malaria for good? Authors: Susan Crow, Meghan Pawlowski, Manyowa Meki, LaraAuthors: LaDage, Timothy Roth II, Cynthia Downs, BarryKyros SinervoKyrou, Andrew and Vladimir Hammond, Pravosudov Andrea Crisanti & others Associate Editors: LindseySeda Dawson Hall and and Gogi Madeleine Kalka Corcoran Abstract Nobody likes the buzzing sound or itchy bite of mosquitoes. What if we used genetic engineering? Here we modified But mosquito bites (only females bite, by the way!) are not the genetic makeup of Anopheles gambiae mosquitoes (the just irritating: they can carry and spread deadly diseases main carriers of malaria). The mutation prevented females such as malaria, dengue, yellow fever and many more. Every from biting and laying eggs. It spread through our caged year, millions of people die from mosquito-borne diseases and populations quickly and drove them extinct. Our results pave most of them are young children. There are ways to get rid the way for lowering mosquito populations in the wild and of mosquitoes and prevent such diseases, but they are not as getting rid of malaria in the future. effective as we would like. EDITING GENES WITH CRISPR A tool used by scientists to precisely edit genes inside cells. Introduction It consists of two parts… Cas9 Guide RNA (An enzyme that (Directs the Cas9 You may have heard about malaria and the devastation it cuts DNA) + to the target DNA) causes in Africa. But did you know that a child dies of malaria every two minutes? Despite global efforts, malaria remains one of the world’s deadliest diseases.