Equity Impacts of Dollar Store Vaccine Distribution
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
HD [email protected] Or by Writing to the Directors at the Following Address
THE HOME DEPOT PROXY STATEMENT AND NOTICE OF 2020 ANNUAL MEETING OF SHAREHOLDERS Thursday, May 21, 2020 at 9:00 a.m., Eastern Time COBB GALLERIA CENTRE, ATLANTA, GA Table of Contents INVESTOR FACTSHEET Strategy Our One Home Depot strategy aims to deliver shareholder value and grow our market share by providing best- in-class customer service through a seamless, interconnected shopping experience for our customers. We are continuously improving our online and in-store experience and providing enhanced training for our associates. In addition, to ensure we are the product authority in home improvement, we strive to provide unique and comprehensive product offerings, continued innovation, and exceptional convenience and value. To execute our strategy, we have committed approximately $11 billion over a multi-year period to investments in our stores, associates, interconnected and digital experience, pro customer experience, services business, supply chain, and product and innovation. Shareholder Return Principles Our first priority for our use of cash is investing in our business, as reflected by our One Home Depot strategy. Our use of the remainder of our cash is guided by our shareholder return principles: • Dividend Principle: Look to increase the dividend every year as we grow earnings • Return on Invested Capital Principle: Maintain a high return on invested capital, benchmarking all uses of excess liquidity against value created for shareholders through share repurchases • Share Repurchase Principle: After meeting the needs of the business, look to return excess cash to shareholders in the form of share repurchases Key Financial Performance Metrics Set forth below are key financial performance metrics for the indicated fiscal years. -

UNITED STATES SECURITIES and EXCHANGE COMMISSION Washington, D.C
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-Q QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the quarterly period ended July 31, 2015 Commission File Number: 001-11421 DOLLAR GENERAL CORPORATION (Exact name of Registrant as specified in its charter) TENNESSEE 61-0502302 (State or other jurisdiction of (I.R.S. Employer incorporation or organization) Identification No.) 100 MISSION RIDGE GOODLETTSVILLE, TN 37072 (Address of principal executive offices, zip code) Registrant’s telephone number, including area code: (615) 855-4000 Indicate by check mark whether the Registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the Registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No o Indicate by check mark whether the Registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the Registrant was required to submit and post such files). Yes x No o Indicate by check mark whether the Registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer,” and “smaller reporting company” in Rule 12b-2 of the Exchange Act. -

Annual Report Also Accompanies This Letter
ANNUAL MEETING ABOUT DOLLAR GENERAL Dollar General Corporation’s annual meeting of shareholders is scheduled for 9 a.m. Central Time on Dollar General Corporation has been delivering NET SALES (IN BILLIONS) Wednesday, May 27, 2020, at: value to shoppers for more than 80 years. Dollar $27.8 Goodlettsville City Hall Auditorium $25.6 General helps shoppers Save time. Save money. $23.5 105 South Main Street, Goodlettsville, TN 37072 ® $22.0 Every day! by o ering products that are frequently $20.4 used and replenished, such as food, snacks, health Shareholders of record as of March 19, 2020 are and beauty aids, cleaning supplies, basic apparel, entitled to vote at the meeting. housewares and seasonal items at everyday low prices in convenient neighborhood locations. NYSE: DG 2015 2016 2017 2018 2019 Dollar General operated 16,278 stores in 44 states The common stock of Dollar General Corporation is as of January 31, 2020. In addition to high-quality traded on the New York Stock Exchange under the private brands, Dollar General sells products ENDING STORE COUNT trading symbol “DG.” The number of shareholders of from America’s most-trusted manufacturers such 16,278 record as of March 19, 2020 was 2,617. 15,370 Visit www.dollargeneral.com as Clorox, Energizer, Procter & Gamble, Hanes, 14,534 to learn more about Dollar General Coca-Cola, Mars, Unilever, Nestle, Kimberly-Clark, 13,320 STOCK PERFORMANCE GRAPH 12,483 and shop online. Kellogg’s, General Mills, and PepsiCo. The graph below compares Dollar General Corporation’s cumulative total shareholder return on common stock STORES with the cumulative total returns of the S&P 500 index STORES IN 44 STATES DISTRIBUTION CENTER and the S&P Retailing index. -

Dollar General
NNN Dollar General the strongest dollar store chain High growth metro area REPRESENTATIVE PHOTO For more info on this opportunity please contact: very low unemployment RICK SANNER BOB SANNER [email protected] | (415) 274-2709 [email protected] | (415) 274-2717 rent increases CA BRE# 01792433 CA BRE# 00869657 JOHN ANDREINI CHRIS KOSTANECKI just opened [email protected] | (415) 274-2715 [email protected] | (415) 274-2701 118 Riley Ave, Ogden, KS 66517 CA BRE# 01440360 CA BRE# 01002010 In conjuction with KS Licensed Broker: Phil Bundy [email protected] | (316) 686-9292 Capital Pacific collaborates. Click here to meet the rest of our San Francisco team. NNN PROPERTY IN OGDEN, KANSAS Investment Highlights New 15-year primary term lease with four (4) five-year options with a 10% rental increase at the beginning of each option period. There is also a 3% rent increase at year 11. Ogden is a suburb of Manhattan, Kansas (home of Kansas State University), and is a part of the Manhattan MSA. The subject Representative Photos property is also quite close to one of the US Army’s largest bases, Ft. Riley. PRICE ............ $1,339,308 RENTABLE SF .........9,100 SF CAP RATE ............6.65% YEAR BUILT ..........2014 LEASE TYPE ..........NNN INVESTMENT GRADE CREDIT Dollar General’s credit is BBB- and the company’s credit rating has been raised four times since 2009. It has a better credit rating than both of its large competitors (See more information later in this offering) STRONG TENANT During fiscal 2014, Dollar -
Dollar Stores Are Multiplying Rapidly
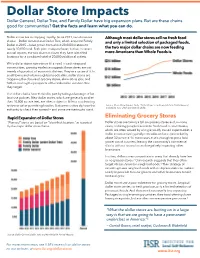
Dollar Store Impacts Dollar General, Dollar Tree, and Family Dollar have big expansion plans. But are these chains good for communities? Get the facts and learn what you can do. Dollar stores are multiplying rapidly. Since 2011, two dominant Although most dollar stores sell no fresh food chains — Dollar General and Dollar Tree, which acquired Family and only a limited selection of packaged foods, Dollar in 2015 — have grown from about 20,000 locations to nearly 30,000 total. Both plan to expand even further. In recent the two major dollar chains are now feeding annual reports, the two chains indicate they have identified more Americans than Whole Foods is. locations for a combined total of 20,000 additional outlets. While dollar stores sometimes fill a need in cash-strapped communities, growing evidence suggests these stores are not merely a byproduct of economic distress. They’re a cause of it. In small towns and urban neighborhoods alike, dollar stores are triggering the closure of grocery stores, eliminating jobs, and further eroding the prospects of the vulnerable communities they target. The dollar chains have thrived in part by taking advantage of lax land use policies. New dollar stores, which are generally smaller than 10,000 square feet, are often subject to little or no planning review or other permitting hurdles. But communities do have the Source: Chain Store Guide | Note: “Dollar Stores” combines data from Dollar General and Dollar Tree, which owns Family Dollar authority to check their spread — and some are starting to use it. Rapid Expansion of Dollar Stores Eliminating Grocery Stores “Planned” stores are based on “identified locations” as reported Dollar stores are taking a toll on grocery stores and, in many by the major dollar store chains. -

ECRM Ad Comparisons the LEADING PROVIDER of PROMOTIONAL DATA and BUSINESS INTELLIGENCE St
ECRM Ad Comparisons THE LEADING PROVIDER OF PROMOTIONAL DATA AND BUSINESS INTELLIGENCE St. Patrick’s Day Promotional Review 2013 versus 2014 Confidential and Proprietary to ECRM 1 METHODOLOGY Effective Ad Count Used in Study: Effective Ad Count gives partial credit to any product that shares an ad block with other products in order to provide more context in promotional analysis. For example: If 4 products are present in an ad block each will only receive a .25 count for that particular promotion. If 3 products are present each one receives .33 count. Time Periods: Current Year: 2/16/2014 - 3/22/2014 Prior Year: 2/17/2013 - 3/23/2013 Retailers Used in Representative Market Review: A & P, Albertson's - SoCal (SVU), Albertsons SOC, CVS, Dollar General, Family Dollar, Food Lion, Giant Eagle, Giant Food Landover, H.E.B., Jewel-Osco (NAI), Jewel-Osco (SVU), Kmart, Kroger CIN, Meijer, Rite Aid, Safeway Stores, Stater Bros, Super 1 Foods, Target Stores, Walgreens, Walmart-US, Winn Dixie. Representative Markets Used. Retailers Used in Promoted Price Study: Chicago Market Retailers: CVS, Dominick's Finer Foods, Food 4 Less, Meijer, Strack & Van Til, Target Stores, Ultra Foods. Media Type: Circular Promotions. Sampling Methodology: A typical basket of St. Patrick’s Day items was developed using the following categories: Beef, Cheese, Cheese Chunk/Block, Cordial, Deli Beef/Roast Beef, Deli Cheese, Dry Potatoes, Fingerling Potatoes, Fresh Cut Flowers, Grated Cheese, Imported Beer, Irish Whiskey, Other Vegetables, Petite Potatoes, Potato Chips, Red Potatoes, Russet Potatoes, Specialty Cheeses, White Potatoes, Yellow Potatoes and Bakery In-Store. The basket was used to identify pages containing St. -

RETAIL INVESTOR PRESENTATION Contents
SECOND QUARTER 2019 RETAIL INVESTOR PRESENTATION Contents Investment Thesis 4 Company Overview 5 Performance Track Record 10 Dependable Dividends 11 Portfolio Diversification 15 Asset Management & Real Estate Operations 22 Investment Strategy 25 Capital Structure and Scalability 28 Business Plan 32 Appendix 33 All data as of June 30, 2019 unless otherwise specified 2 Safe Harbor For Forward-Looking Statements Statements in this investor presentation that are not strictly historical are "forward-looking" statements. Forward-looking statements involve known and unknown risks, which may cause the company‘s actual future results to differ materially from expected results. These risks include, among others, general economic conditions, domestic and foreign real estate conditions, tenant financial health, the availability of capital to finance planned growth, continued volatility and uncertainty in the credit markets and broader financial markets, property acquisitions and the timing of these acquisitions, charges for property impairments, and the outcome of any legal proceedings to which the company is a party, as described in the company's filings with the Securities and Exchange Commission. Consequently, forward-looking statements should be regarded solely as reflections of the company's current operating plans and estimates. Actual operating results may differ materially from what is expressed or forecast in this investor presentation. The company undertakes no obligation to publicly release the results of any revisions to these forward-looking statements that may be made to reflect events or circumstances after the date these statements were made. 3 Investment Thesis Business model offers attractive total return with minimal cash flow volatility PROVEN TRACK RECORD OF RETURNS 16.4% Compound Average Annual Total Return Since ‘94 NYSE Listing 0.4 Beta vs. -

Dollar General- 24 1St Street Allegany, NY 14706
OFFERING MEMORANDUM 24 1st Street Allegany, NY 14706 LEASE & LOCATION: » Brand new 10 year lease extension (base term will now run through 4/30/2029) DOLLAR GENERAL » Dollar General Plus format – The store is 11,782 sf which is typically an 24 1st Street indicator of strong sales and a proven market ALLEGANY, NY 14706 » All masonry block construction – no metal sides » Brand new roof which was replaced in 2017 (15 year transferable LISTED BY: warranty) JOSH BISHOP » Tenant pays an additional $550 / month toward parking lot maintenance VP & DIRECTOR which does not have to be reconciled (potential for additional revenue) (snow removal is reimbursed separately at 100% of the cost) DIRECT (214) 692-2289 MOBILE (315) 730-6228 » The subject property is located just off I-86 which sees roughly 15,000 [email protected] vehicles daily LIC # 688810 (TX) » ±22,000 residents within a 5-mile radius ARON CLINE SVP & SENIOR DIRECTOR » Allegany is home to St. Bonaventure University LIC # 01904371 (CA) » Local retail tenants include The Home Depot, Walmart, AMC, McDonald’s, Friendly’s, Tractor Supply, AutoZone, KFC, Applebee’s, CALVIN SHORT Verizon, Tim Hortons, Kohl’s, CVS, Burger King and many more. SVP & SENIOR DIRECTOR LIC # 01927216 (CA) TENANT: CHAD KURZ SVP & NATIONAL DIRECTOR » Investment grade credit rating of BBB, recently upgraded from BBB- LIC # 01911198 (CA) » Dollar General currently operates ±15,500 locations nationwide with plans to add another ±900 store in 2019 BROKER OF RECORD JEFFREY TERWILLIGER » LIC # 30TE0892302 (NY) Dollar General is the premier dollar store and the nation’s largest small- box discount retailer » Dollar General has a market cap of more than $30 billion 2 DOLLAR GENERAL ALLEGANY, NY PARCEL MAP St. -
Serving Others Report
SERVING OTHERS REPORT AS OF JUNE 2020 TABLE OF CONTENTS OUR COMPANY Letter from our CEO 3 Our Company Overview 4 Our History 5-6 OUR MISSION OF SERVING OTHERS Introduction: Our Mission 7 Serving Our Customers 8-9 Serving Our Employees 10-13 Serving Our Communities 14-15 Serving Our Environment 16-17 Serving Our Shareholders 18-20 OUR CODE Business Conduct & Ethics 21 APPENDICES Chemical Policy 22 SERVING OTHERS REPORT 2 FROM OUR CEO Our fiscal 2019 was one of celebrations as we marked our 80th anniversary and opened our 16,000th store location. While much has changed in the retail landscape since our founding in 1939, Dollar General’s mission of Serving Others remains strong and steadfastly integrated into the fabric of our business. Our second annual Serving Others Report serves as an extension of that mission by communicating the many ways in which we serve our customers, employees, communities and shareholders every day. Our core values help guide our more than 155,000 employees in more than 16,500 stores, more than 20 traditional and DG Fresh distribution centers and our Store Support Center serve others every day. Whether we are helping customers stretch their budget, generating positive economic impact with each new store and distribution center, providing career development opportunities through our growing organization, promoting sustainable business practices, creating shareholder value or helping further literacy and education initiatives in the communities we proudly call home, Serving Others is not just a mission—it’s a cornerstone of our culture and a filter through which business decisions are made. -

DOLLAR GENERAL Tel: 775-348-5220 1470 N
Offering Memorandum Contact: Todd Blonsley, MBA, CCIM Senior Vice President Investments DOLLAR GENERAL Tel: 775-348-5220 1470 N. State Hwy 95 • Bastrop, TX 78602 [email protected] Tim Speck, Texas Broker of Record NON- ENDORSEMENT AND DISCLAIMER NOTICE Confidentiality and Disclaimer The information contained in the following Marketing Brochure is proprietary and strictly confidential. It is intended to be reviewed only by the party receiving it from Marcus & Millichap Real Estate Investment Services, Inc. ("Marcus & Millichap") and should not be made available to any other person or entity without the written consent of Marcus & Millichap. This Marketing Brochure has been prepared to provide summary, unverified information to prospective purchasers, and to establish only a preliminary level of interest in the subject property. The information contained herein is not a substitute for a thorough due diligence investigation. Marcus & Millichap has not made any investigation, and makes no warranty or representation, with respect to the income or expenses for the subject property, the future projected financial performance of the property, the size and square footage of the property and improvements, the presence or absence of contaminating substances, PCB's or asbestos, the compliance with State and Federal regulations, the physical condition of the improvements thereon, or the financial condition or business prospects of any tenant, or any tenant's plans or intentions to continue its occupancy of the subject property. The information contained in this Marketing Brochure has been obtained from sources we believe to be reliable; however, Marcus & Millichap has not verified, and will not verify, any of the information contained herein, nor has Marcus & Millichap conducted any investigation regarding these matters and makes no warranty or representation whatsoever regarding the accuracy or completeness of the information provided. -

Walgreens 2 Dearborn Heights, Mi Investment Highlights
DEARBORN HEIGHTS, MI | OFFERING MEMORANDUM TABLE OF CONTENTS EXCLUSIVELY LISTED BY: BILL PEDERSEN 03 INVESTMENT HIGHLIGHTS SENIOR ASSOCIATE DIR (949) 432-4501 MOB (831) 246-0646 04 FINANCIAL OVERVIEW [email protected] LIC # 01975700 (CA) 07 TENANT OVERVIEW KYLE MATTHEWS 08 AREA OVERVIEW CEO & CHAIRMAN BROKER OF RECORD KYLE MATTHEWS 6505399495 (MI) WALGREENS 2 DEARBORN HEIGHTS, MI INVESTMENT HIGHLIGHTS • Below Average Rent – Walgreens is paying less than $10.00/PSF in rent, which is less than half of the national average for Walgreens. • Over 20 years in Operation at this Location – Walgreens has occupied this building since 1997. • Prototype Walgreens Store Format on Signalized Intersection – Drive-thru 13,905 SF store format on 1.45 acres. At the southeast corner of N Telegraph Rd (55,000 VPD) and Joy Rd (16,000 VPD). • Nearby Commercial Tenants – Include CVS, Dollar General, Advance Auto Parts, Taco Bell, The Salvation Army, 7-Eleven, Aldi, Starbucks, Dunkin’ Donuts, Dollar General, Chase Bank, and many more. • Dense Population – More than 392,000 residents in the 5-mile radius with an average household income of $64,000. • Detroit MSA – Less than 17 miles from downtown Detroit. Detroit MSA is home to about 4.3 million people and is the second largest Midwest MSA only behind Chicago. • Nationally Recognized Investment Grade Tenant – Lease is fully guaranteed by Walgreens Co. (S&P’s Rated BBB). The company is ranked #17 on the 2017 Fortune 500. MATTHEWS™ 3 FINANCIAL OVERVIEW EXECUTIVE SUMMARY 8706 North Telegraph Rd PROPERTY ADDRESS Dearborn Heights, MI 48127 GLA ± 13,905 SF WALGREENS - STORE # 4367 LOT SIZE ±1.45 AC (63,162 SF) 8706 North Telegraph Rd YEAR BUILT 1997 Dearborn Heights, MI 48127 APN 33 001 02 0108 300 WALGREENS LEASE SUMMARY $1,731,000 TENANT WALGREEN CO. -

Oregon Redemption Centers Albany Beaverton
Oregon Redemption Centers and Associated Retailers (5,000 or more sq ft in size) ZONE 1 ZONE 2 EXEMPT** DEALER REDEMPTION CENTERS*** FULL SERVICE PARTICIPATING RETAILERS PARTICIPATING RETAILERS (accept 144 containers) (accept 24 containers) REDEMPTION CENTERS (accept 0 containers) (accept 24 containers) 0 - 2.0 miles radius Albany from redemption center No Zone 2 Zone 1 No Zone 2141 Santiam Hwy SE Albany Grocery Outlet Albany East Liquor Store 1103 ALOHA 1950 14th Ave SE 2530 Pacific Blvd SE Albertsons #3557 approved 6/18/2015 Big Lots #4660 Dollar Tree #1508 6055 SW 185th 2000 14th Ave SE, Ste 102 1307 Waverly Dr SE Bi-Mart #606 Lowe's #3057 BEAVERTON 2272 Santiam Hwy 1300 9th Ave SE Fred Meyer #482 Costco #0682 15995 SW Walker Rd 3130 Killdeer Ave SE Fred Meyer #005 CANBY 2500 Santiam Blvd Fred Meyer #651 North Albany Market 1401 SE 1st Ave 621 NE Hickory Rite Aid #5365 Safeway #2604 1235 Waverly Dr SE 1051 SW 1st Ave Safeway #1659 1990 14th Ave SE CLACKAMAS Target #T609 Fred Meyer #063 2255 14th Ave SE 16301 SE 82nd Dr Walgreens #6530 1700 Pacific Blvd SE DALLAS Walmart #5396 Safeway #4404 1330 Goldfish Farm SE 138 W Ellendale Ave Wheeler Dealer 1740 SE Geary St EUGENE Winco Foods Fred Meyer #325 (Santa Clara) 3100 Pacific Blvd SE 60 Division St 0 - 2.0 miles radius 2.01 - 2.8 miles radius Beaverton from redemption center from redemption center Either Zone FLORENCE 9307 SW Beaverton-Hillsdale Hwy Albertsons #505 99 Ranch Cost Plus World Market #6060 Fred Meyer #464 5415 SW Beaverton Hillsdale Hwy 8155 SW Hall Blvd 10108 SW Washington