Comparison of Long-Term Clinical Implications of Beta-Blockade In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

3364-136-03-01 Preparation and Administration of Medications Used in Respiratory Care Page 2
Name of Policy: Preparation and Administration of Medications Used in Respiratory Care Policy Number: 3364-136-03-01 Department: Respiratory Care Approving Officer: Associate VP Patient Care Services / CNO Responsible Agent: Director, Respiratory Care Scope: Effective Date: 6/1/2020 The University of Toledo Medical Center Initial Effective Date: 5/7/1989 Respiratory Care Department New policy proposal X Minor/technical revision of existing policy Major revision of existing policy Reaffirmation of existing policy (A) Policy Statement Medications administered by persons in the Respiratory Care Department will be in accordance with the physician's order as described in Hospital Policy # 3364-100-70-10 “Medication Management”, Pharmacy policies #3364-133-28 “Use of single and multi-dose Vials”, and # 3364-133-70 “Standard Medication Administration Times”. Medications for Respiratory Care administration must be approved by the Medical Director of Respiratory Care. Approved drugs are listed in attached Appendix A for 3364-136-03-01. (B) Purpose of Policy To insure safe preparation and administration of medications used by the practitioners of the Respiratory Care Department. (C) Procedure I. Procedure for Preparing Medications for Patient Use: Unit dose: . Unit dose medications will be used when available in ordered doses. Medications removed from the AcuDose Medication System and not administered must be returned to the AcuDose using the return medication procedure. Persons administering medications for respiratory care purposes will be knowledgeable about the drug being administered, regarding its purpose, indication, contraindication, and side affects. II. Medication Errors: The on-line SafetyNet system must be used for occurrences if: . A medication is missed. -
Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE MEDICINAL PRODUCT Salbutamol CFC-Free Inhaler 100 micrograms per metered dose, pressurised inhalation, suspension 2 QUALITATIVE AND QUANTITATIVE COMPOSITION One metered dose contains 100 micrograms of salbutamol (equivalent to 120 micrograms of salbutamol sulphate). This is equivalent to a delivered dose of 90 micrograms of salbutamol (equivalent to 108 micrograms of salbutamol sulphate). For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Pressurised inhalation suspension Pressurised inhalation suspension supplied in an aluminium canister with a metering valve and a plastic actuator and dust cap. 4 CLINICAL PARTICULARS 4.1 Therapeutic Indications Salbutamol CFC-Free Inhaler is indicated in adults, adolescents and children. For babies and children under 4 years of age, see sections 4.2 and 5.1. Salbutamol CFC-Free Inhaler is indicated for the relief and prevention of bronchial asthma and conditions associated with reversible airways obstruction. Salbutamol CFC-Free Inhaler can be used as relief medication in the management of mild, moderate or severe asthma, provided that its use does not delay the introduction and use of regular inhaled corticosteroid therapy, where necessary. 4.2 Posology and method of administration Salbutamol CFC-Free Inhaler is for oral inhalation use only. Posology Adults (including the elderly) and adolescents (children 12 years and over): For the relief of acute bronchospasm, one inhalation (100 micrograms) increasing to two inhalations (200 micrograms), if necessary. To prevent allergen- or exercise-induced symptoms, two inhalations (200 micrograms) should be taken 10-15 minutes before challenge. Maximum daily dose: two inhalations (200 micrograms) up to four times a day. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

Or Should It Be Mast Cell Mediator Disorders?
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Expert Rev Manuscript Author Clin Immunol Manuscript Author . Author manuscript; available in PMC 2020 February 06. Published in final edited form as: Expert Rev Clin Immunol. 2019 June ; 15(6): 639–656. doi:10.1080/1744666X.2019.1596800. Recent advances in our understanding of mast cell activation – or should it be mast cell mediator disorders? Theoharis C. Theoharidesa,b,c,d, Irene Tsilionia, Huali Rene aMolecular Immunopharmacology and Drug Discovery Laboratory, Department of Immunology, Tufts University School of Medicine, Boston, MA, USA bSackler School of Graduate Biomedical Sciences, Tufts University School of Medicine, Boston, MA, USA cDepartment of Internal Medicine, Tufts University School of Medicine and Tufts Medical Center, Boston, MA, USA dDepartment of Psychiatry, Tufts University School of Medicine and Tufts Medical Center, Boston, MA, USA eDepartment of Otolaryngology, Beijing Electric Power Hospital, Beijing, China Abstract Introduction: An increasing number of patients present with multiple symptoms affecting many organs including the brain due to multiple mediators released by mast cells. These unique tissue immune cells are critical for allergic reactions triggered by immunoglobulin E (IgE), but are also stimulated (not activated) by immune, drug, environmental, food, infectious, and stress triggers, leading to secretion of multiple mediators often without histamine and tryptase. The presentation, diagnosis, and management of the spectrum of mast cell disorders are very confusing. As a result, specialists have recently excluded neuropsychiatric symptoms, and made the diagnostic criteria stricter, at the expense of excluding most patients. Areas covered: A literature search was performed on papers published between January 1990 and November 2018 using MEDLINE. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Chapter 10 Drugs for Treating Colds and Allergies Case Study It Seems
Chapter 10 Drugs for Treating Colds and Allergies Case Study It seems that the university’s wrestling team benefited from the exceptionally long break the coach gave them over the Christmas holidays because they all seem eager to continue the remaining part of the season in earnest. However, Sam, the team’s 74-kg class wrestler, appears uncomfortable and less energetic. He reports that over break he contracted an upper respiratory tract infection. Sam started taking an over-the-counter (OTC) medication to relieve his runny nose when he first felt the onset of the cold. He states that it seems to be helping, but he is feeling more tired since starting the medication. What is a possible explanation for Sam’s symptoms? Answer: The medication Sam is taking likely contains a first-generation antihistamine. These medications are found in several OTC cough, cold, and allergy products, both alone and in combination with other medications. They are helpful in colds because they decrease mucus production and have a drying effect, therefore relieving the symptom of runny nose. However, they also have a major adverse effect of causing drowsiness. This is likely the cause of Sam’s tiredness. The second-generation antihistamines are non-sedating; however, they also lack the drying effect of the first-generation antihistamines and therefore would not be as effective in treating Sam’s symptoms. Some of the first-generation antihistamines, such as chlorpheniramine, have less of a sedating effect, so switching products may help with the adverse effects. Exam Questions 1. All of the following intranasal corticosteroid products are available by prescription only except for: a. -

King's Research Portal
King’s Research Portal DOI: 10.1503/cmaj.160355 Document Version Other version Link to publication record in King's Research Portal Citation for published version (APA): Trifirò, G., De Ridder, M., Sultana, J., Oteri, A., Rijnbeek, P., Pecchioli, S., Mazzaglia, G., Bezemer, I., Garbe, E., Schink, T., Poluzzi, E., Frøslev, T., Molokhia, M., Diemberger, I., & Sturkenboom, M. C. J. M. (2017). Use of azithromycin and risk of ventricular arrhythmia. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 189(15), E560-E568. https://doi.org/10.1503/cmaj.160355 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Annexes to the Annual Report of the European Medicines Agency 2014
Annexes to the annual report of the European Medicines Agency 2014 Table of contents Annex 1 – Members of the Management Board ............................................................................. 2 Annex 2 – Members of the Committee for Medicinal Products for Human Use ................................... 4 Annex 3 – Members of the Pharmacovigilance Risk Assessment Committee ...................................... 6 Annex 4 – Members of the Committee for Medicinal Products for Veterinary Use ............................... 8 Annex 5 – Members of the Committee on Orphan Medicinal Products ............................................ 10 Annex 6 – Members of the Committee on Herbal Medicinal Products .............................................. 12 Annex 07 – Committee for Advanced Therapies .......................................................................... 14 Annex 8 – Members of the Paediatric Committee ........................................................................ 16 Annex 9 – Working parties and working groups .......................................................................... 18 Annex 10 – CHMP opinions in 2014 on medicinal products for human use ...................................... 22 Annex 11 – CVMP opinions in 2014 on medicinal products for veterinary use .................................. 36 Annex 12 – COMP opinions in 2014 on designation of orphan medicinal products ............................ 41 Annex 13 – HMPC European Union herbal monographs in 2014.................................................... -
Ing Medication Targeting Obstructive Lung Disease
PHD THESIS DANISH MEDICAL JOURNAL Spirometry utilisation among Danish adults initiat- ing medication targeting obstructive lung disease Mette Marie Koefoed, MD persisting for at least 2 weeks, and not known to have asthma or This review has been accepted as a thesis together with three previously published other pulmonary diseases. Among these patients over one third papers by University of Southern Denmark 28 February 2013 and defended on 21 has airflow limitation due to asthma or chronic obstructive pul- June 2013 monary disease (COPD); among middle-aged and older patients 7 Tutor(s): Dorte Ejg Jarbøl, Jens Søndergaard and Rene dePont Christensen airflow limitation is predominantly due to COPD, whereas asth- 8 ma is the most common cause among younger age groups. Also, Official opponents: David Price, Peter Lange and Ingrid Louise Titlestad over one third of the patients presenting with symptoms of acute bronchitis (coughing more than two weeks, but no more than Correspondence: Institute of public health, Faculty of Health Sciences, University of Southern Denmark, J.B.Winsløws Vej 9A, DK- 5000 Odense C, Denmark four weeks, and presence of either expectoration of purulent sputum and/or rhonchi assessed by auscultation) in general prac- E-mail: [email protected] tice have airflow limitation due to obstructive lung disease.9 Asthma and COPD are common chronic illnesses10-13 and there is evidence that the prevalence may be higher as a proportion of Dan Med J 2015;62(2):B5004 patients with respiratory symptoms are suffering from these diseases, but are not diagnosed. The papers Management of patients attending general practice with symp- toms like dyspnoea, coughing and wheezing is only sparsely stud- Lack of Spirometry use in Danish Patients initiating medication ied. -

Combination Long-Acting Beta-Agonist Inhaled Corticosteroid: Summary of Clinical Evidence and Drug Utilization Evaluation
Drug Use Research & Management Program DHS Division of Medical Assistance Programs, 500 Summer Street NE, E35; Salem, OR 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Combination Long-Acting Beta-Agonist Inhaled Corticosteroid: Summary of Clinical Evidence and Drug Utilization Evaluation Currently, there are two FDA approved combination long-acting beta agonist (LABA) inhaled corticosteroid (ICS) products on the market: salmeterol / fluticasone propionate (Advair diskus, Advair HFA), and formoterol fumarate dehydrate / budesonide (Symbicort). Both drugs are approved for the treatment of asthma and chronic obstructive pulmonary disease (COPD). Specifically, Advair is indicated for treatment of asthma in patients 4 years and older and treatment of airflow obstruction and reducing exacerbations in patients with COPD. Symbicort is approved for maintenance treatment of asthma in patients 12 years of age and older and treatment of airflow obstruction in patients with COPD. Both agents carry an FDA black box warning related to the excess risk of asthma-related death conferred by the LABA component. The FDA issued a Public Health Advisory and revised the product labeling in November 2005 and March 2006 respectively. In February 2010, the FDA recommended additional labeling changes based on a joint meeting of the Pulmonary Allergy Drugs, Drug Safety and Risk Management, and Pediatric Advisory Committees in December 2008. Summaries of combined LABA-ICS evidence of effectiveness and safety are provided below. Evidence for these summaries was -

2018-07 Chiesi Formoterol HFA 12Μg/Actuation Pressurised In
Confidential CTD - Chiesi Farmaceutici S.p.A. SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT {(Invented) name} 12 micrograms/actuation pressurised inhalation solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each metered dose contains 12 micrograms of formoterol fumarate dihydrate. This corresponds to a delivered dose of 10.1 micrograms. For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Pressurised inhalation solution. 4. CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS For the long-term symptomatic treatment of persistent, moderate to severe asthma in patients requiring regular bronchodilator therapy in combination with long-term antiinflammatory therapy (inhaled and/or oral glucocorticoids). Glucocorticoid therapy should be continued on a regular basis. {(Invented) name} is indicated for the relief of broncho-obstructive symptoms in patients with chronic obstructive pulmonary disease (COPD). 4.2 POSOLOGY AND METHOD OF ADMINISTRATION Posology The dosage depends on the type and severity of disease. The following dosages are recommended for adults, including elderly patients, and adolescents aged 12 years and above: Asthma Adults and adolescents aged 12 years and above: Usually one actuation in the morning and evening (24 micrograms formoterol fumarate dihydrate per day). In severe cases, up to a maximum of two actuations in the morning and evening (48 micrograms of formoterol fumarate dihydrate per day). The maximum daily dose is 4 actuations (48 micrograms formoterol fumarate dihydrate). Children younger than 12 years of age: The safety and efficacy of {(Invented) name} in children younger then 12 years of age has not been established yet, therefore {(Invented) name} should not be used in children. -
Asthma COPD and Asthma-COPD Overlap Syndrome (ACOS)
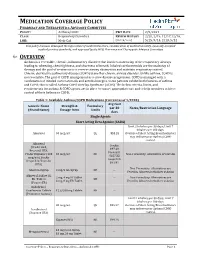
MEDICATION COVERAGE POLICY PHARMACY AND THERAPEUTICS ADVISORY COMMITTEE POLICY: Asthma/COPD P&T DATE 2/9/2021 CLASS: Respiratory Disorders REVIEW HISTORY 2/20, 2/19, 12/17,12/16, LOB: Medi-Cal (MONTH/YEAR) 5/15, 9/14, 2/13, 5/12 This policy has been developed through review of medical literature, consideration of medical necessity, generally accepted medical practice standards, and approved by the HPSJ Pharmacy and Therapeutic Advisory Committee OVERVIEW Asthma is a reversible, chronic, inflammatory disorder that involves narrowing of the respiratory airways leading to wheezing, chest tightness, and shortness of breath. Inhaled corticosteroids are the mainstay of therapy and the goal of treatment is to reverse airway obstruction and maintain respiratory control. Chronic obstructive pulmonary disease (COPD) is another chronic airway disorder. Unlike asthma, COPD is not reversible. The goal of COPD management is to slow disease progression. COPD is managed with a combination of inhaled corticosteroids and anticholinergics. Some patients exhibit both features of asthma and COPD; this is called Asthma-COPD Overlap Syndrome (ACOS). The below criteria, limits, and requirements for asthma & COPD agents are in place to ensure appropriate use and to help members achieve control of their Asthma or COPD. Table 1: Available Asthma/COPD Medications (Current as of 1/2020) Avg Cost Generic Name Strength & Formulary per 30 Notes/Restriction Language (Brand Name) Dosage form Limits days Single Agents Short Acting Beta Agonist (SABA) Limit 2 inhalers per 30 days; Limit 7 inhalers per 180 days. Albuterol 90 mcg/act QL $53.28 Overuse of Short Acting Bronchodilators may indicate poor Asthma/COPD control.