Supplementary Appendix This Appendix Formed Part of the Original Submission and Has Been Peer Reviewed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Information for Persons Who Wish to Seek Asylum in the Russian Federation
INFORMATION FOR PERSONS WHO WISH TO SEEK ASYLUM IN THE RUSSIAN FEDERATION “Everyone has the right to seek and to enjoy in the other countries asylum from persecution”. Article 14 Universal Declaration of Human Rights I. Who is a refugee? According to Article 1 of the Federal Law “On Refugees”, a refugee is: “a person who, owing to well‑founded fear of being persecuted for reasons of race, religion, nationality, membership of particular social group or politi‑ cal opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country”. If you consider yourself a refugee, you should apply for Refugee Status in the Russian Federation and obtain protection from the state. If you consider that you may not meet the refugee definition or you have already been rejected for refugee status, but, nevertheless you can not re‑ turn to your country of origin for humanitarian reasons, you have the right to submit an application for Temporary Asylum status, in accordance to the Article 12 of the Federal Law “On refugees”. Humanitarian reasons may con‑ stitute the following: being subjected to tortures, arbitrary deprivation of life and freedom, and access to emergency medical assistance in case of danger‑ ous disease / illness. II. Who is responsible for determining Refugee status? The responsibility for determining refugee status and providing le‑ gal protection as well as protection against forced return to the country of origin lies with the host state. Refugee status determination in the Russian Federation is conducted by the Federal Migration Service (FMS of Russia) through its territorial branches. -

2019 Annual Report
Table of Contents A Message from the Chairman.............................................................. 1 A Message from the President .............................................................. 3 Our Impact .................................................................................... 4 What’s Unique About Sister Cities International?....................................... 5 Global Leaders Circle............................................................................... 6 2018 Activities....................................................................................... 7 Where We Are (Partnership Maps) ........................................................ 14 Membership with Sister Cities International ........................................... 18 Looking for a Sister City Partner?......................................................... 19 Membership Resources and Discounts ................................................. 20 Youth Leadership Programs ............................................................... 21 YAAS 2018 Winners & Finalists ............................................................ 23 2018 Youth Leadership Summit .......................................................... 24 Sister Cities International’s 2018 Annual Conference in Aurora, Colorado.......................................................................... 26 Annual Awards Program Winners......................................................... 27 Special Education and Virtual Learning in the United States and Palestine (SEVLUP) -
Building Capacity for Plant Conservation – the Role of Botanic Gardens Volume 10 • Number 1 EDITORIAL SARA OLDFIELD 02
Journal of Botanic Gardens Conservation International Volume 10 • Number 1 • January 2013 Building capacity for plant conservation – the role of botanic gardens Volume 10 • Number 1 EDITORIAL SARA OLDFIELD 02 EDITORS 21 03 BUILDING CAPACITY THROUGH TEACHING ESSENTIAL SKILLS Suzanne Sharrock Sara Oldfield THE ROLE OF BOTANIC GARDENS IN LAURA COHEN AND LEIGH MORRIS Director of Global Secretary General Programmes BUILDING CAPACITY FOR PLANT Cover Photo : Reintroduction of “pata de elefante” CONSERVATION MARIANA CHAVEZ Beaucarnea gracilis in Cuicatlán, Oaxaca, México. A collaborative project between the Botanical Garden and AND SUZANNE SHARROCK the local people (Archive of the Jardín Botanico of the Universidad Nacional Autonoma de Mexico) Design : Seascape www.seascapedesign.co.uk BGjournal is published by Botanic Gardens Conservation International (BGCI) . It is published twice a year and is sent to all BGCI members. Membership is open to all interested individuals, institutions and organisations that support the aims of BGCI (see inside back cover for Membership application form). 08 25 Further details available from: THE UNIVERSITY OF WASHINGTON • Botanic Gardens Conservation International, Descanso BOTANIC GARDEN AND RESTORATION BUILDING CAPACITY AND FACILITATING House, 199 Kew Road, Richmond, Surrey TW9 3BW UK. Tel: +44 (0)20 8332 5953, Fax: +44 (0)20 8332 5956 ECOLOGY KERN EWING AND NETWORKS FOR PLANT E-mail: [email protected], www.bgci.org SARAH REICHARD CONSERVATION: KEW’S ON-GOING • BGCI-Russia, c/o Main Botanical Gardens, COMMITMENT -

Russian Tour and Cruise St. Petersburg, Moscow and Tula
Russian Tour and Cruise St. Petersburg, Moscow and Tula Albany-Tula Alliance 20th Anniversary June 16-July 4, 20ll Sponsored by The Albany-Tula Alliance with Grand Circle Travel Arrangements by Charlotte S. Buchanan Russian Tour and Cruise St. Petersburg, Moscow and Tula Albany-Tula Alliance 20th Anniversary Join the Grand Central Tours (GCT) for its cruise and tours from St. Petersburg to Moscow. Experience the personal relationships developed over 20 years with the people of Tula and visit the estate of Tolstoy. Please visit the website of the Albany-Tula Alliance--www.albanytula.org for detailed itineraries, photos, prices, and other information and reservation forms. The GCT portion of the tour includes the following: Round trip coach transport from Albany to JFK and round trip transatlantic air transportation—from New York JFK to St. Petersburg Airport welcome by a GCT representative at your destination Accommodations—14 nights on a Grand Circle river ship in an outside cabin 40 meals— 14 breakfasts, 12 lunches, and 14 dinners (including complimentary wine with dinner) 11 exclusive, guided sightseeing tours—Moscow City & Subway tour, Novodevichy (New Maiden) Cemetery, Moscow Circus, The Kremlin & the Armory Museum, Uglich, Kizhi Island, Petrozavodsk, Peter & Paul Fortress, St. Petersburg city tour, Hermitage Museum, Catherine’s Palace & Park Exclusive Discovery Series events—Meeting with Russian World War II veterans, Russian handcrafts presentation, Russian language lesson, Vodka tasting, Blini party, Home-Hosted Visit, Candid -
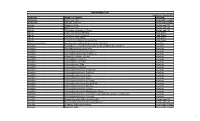
Unai Members List August 2021
UNAI MEMBER LIST Updated 27 August 2021 COUNTRY NAME OF SCHOOL REGION Afghanistan Kateb University Asia and the Pacific Afghanistan Spinghar University Asia and the Pacific Albania Academy of Arts Europe and CIS Albania Epoka University Europe and CIS Albania Polytechnic University of Tirana Europe and CIS Algeria Centre Universitaire d'El Tarf Arab States Algeria Université 8 Mai 1945 Guelma Arab States Algeria Université Ferhat Abbas Arab States Algeria University of Mohamed Boudiaf M’Sila Arab States Antigua and Barbuda American University of Antigua College of Medicine Americas Argentina Facultad de Ciencias Económicas de la Universidad de Buenos Aires Americas Argentina Facultad Regional Buenos Aires Americas Argentina Universidad Abierta Interamericana Americas Argentina Universidad Argentina de la Empresa Americas Argentina Universidad Católica de Salta Americas Argentina Universidad de Congreso Americas Argentina Universidad de La Punta Americas Argentina Universidad del CEMA Americas Argentina Universidad del Salvador Americas Argentina Universidad Nacional de Avellaneda Americas Argentina Universidad Nacional de Cordoba Americas Argentina Universidad Nacional de Cuyo Americas Argentina Universidad Nacional de Jujuy Americas Argentina Universidad Nacional de la Pampa Americas Argentina Universidad Nacional de Mar del Plata Americas Argentina Universidad Nacional de Quilmes Americas Argentina Universidad Nacional de Rosario Americas Argentina Universidad Nacional de Santiago del Estero Americas Argentina Universidad Nacional de -

Bishkek, Kyrgyzstan
Ongoing Norwegian Capacity Building Programmes in 13 countries of Central and Eastern Europe and the CIS Some few highlights. Trond Dahlsveen, ENSI - Energy Saving International AS, NEEG - The Norwegian Energy Efficiency Group … co-ordinated with ongoing UN ECE projects 16th Session of the Energy Efficiency 21 Project (EE 21) Geneva, 29 June - 1 July 2005 Norwegian, long-term Programmes on Energy Efficiency and Cleaner Production Capacity Building according UN ECE EE 2000 “Demo-Zones” Concept A set of activities: Training, Education New Financing Technologies Demo Projects Networks Information Commercial Projects Developing local capacities and skills: Technical Universities Industrial companies Energy Efficiency and Cleaner Production Consultants and experts Centre Authorities & Municipalities Northwest Russia: six Energy Efficiency Centres 1. Kirovsk 1996 3. Arkhangelsk 1999 5. Syktyvkar 2003 2. Murmansk 1998 4. Petrozavodsk 1999 6. Narjan Mar 2004 2004: 33 employees, 100 % self-financed Combined Training and Project Development Session 1 Homework Company Visits Session 2 Homework Session 3 Homework Result: Projects developed, ready for implementation First Russian Demo-project: Kirovsk Kindergarten no. 12 Before After Total heated area 3.000 m2 Total investment 170.000 USD Energy savings 60 % Payback 4 years “Kirovsk City Revolving Fund” Energy Saving Programme (For establishment of Revolving Funds) 25 projects developed together with the Centres (Capacity Building) 5 Projects: technical completed Investment 14 Projects: under implementation -

Atlantic Ocean
60˚ 30˚ 20˚ 10˚ 0˚ 10˚ 20˚ 30˚ 40˚ 50˚ 60˚ 70˚ 60˚ Barents Sea Nizhnevartovsk Inta Surgut Ob' Reykjavik Nefteyugansk Pe Tromso cor Pechora Ob' a a Thjors Irtys Iceland Harstad Murmansk Kozhva Monchegorsk Narvik Kiruna Apatity tys Ir I Ukhta s Bodo Malmberget im Tobol'sk Norwegian Sea Troitsko-Pechorsk Rovaniemi Kemi Severodvinsk Archangel Lulea Serov Ishim cegda Krasnotur'insk T Vy ob Sweden Oulu ol Namsos Pitea Solikamsk Irbit Tyumen' Faroe Islands Finland Trondheim Stenkjaer Jakobstad Kotlas Russia Asbest Atlantic Kristiansund Lake Onega Kuopio Velikiy Ustyug Alesund Perm' Ostersund Vaasa Petrozavodsk Kungur Ocean Lake Yekaterinburg Shetland Islands Jyvaskyla Suchona Glama Mikkeli Ladoga Norway T Sundsvall ob Kirovo-Chepetsk Chelyabinsk ol Gjovik Bollnas Lappeenranta Sarapul Bergen Oslo Gavle Turku Helsinki St. Petersburg Qostanay Kama Oufa Haugesund Vasteras Kostroma Magnitogorsk Inverness Stavanger Tverca Tallinn Cheboksary Kazan' Skien Orebro Rybinsk Volga 50˚ Aberdeen Stockholm EstoniaJarve Salavat Glasgow Dundee Yaroslavl' Londonderry Gothenburg Linkoping Tartu Staraja Russa a Nizhniy Novgorod Ayr Edinburgh Ok 50˚ V Pskov olga Thisted Jonkoping Riga Moscow Vladimir Orenburg Ural Orsk Belfast Tynemouth Denmark Volga Dublin Viborg Liepaja Latvia Chapayevsk Aqtobe Tralee Preston North Sea Daugavpils Obninsk Saransk Ireland Arhus Malmo Baltic Sea Lithuania Penza Kaluga Ryazan' Oral Liverpool Manchester Copenhagen Klaipeda Taurage Smolensk Cork TulaDon Tambov Balakovo Birmingham Gdansk Vilnius Minsk Kirov Saratov Nottingham KazakhstanUral United Hamburg Balashov Swansea Neth. Stettin Babruysk Oriol KingdomLondon Grodno Dnieper Bristol Amsterdam Belarus Kamyshin Poznan Warsaw Voronezh Southampton Antwerp The Hague Bug Homyel' Kursk Berlin Prypyat Atyrau Guernsey Cologne Poland Belgorod Don Volzhskiy Jersey BrusselsBel. Wroclaw Brest Sumy Liege Germany Lodz Kiev Kharkiv Akhtubinsk Me Volgograd Caen Main Lublin Poltava Volga Rennes Paris us Lux. -

Alexey Golubev
ALEXEY GOLUBEV 560 Agnes Arnold Hall, 3553 Cullen Boulevard, Houston, TX 77204 phone: 1-713-743-7277 email: [email protected] http://uh.academia.edu/AlexeyGolubev PROFESSIONAL EMPLOYMENT 2017– Assistant Professor in Russian History and Digital Humanities, Department of History, University of Houston. 2016–2017 Banting Postdoctoral Fellow, Department of History, University of Toronto. 2015 Sessional Lecturer, Department of History, University of British Columbia. 2009–2011 Assistant Professor (fixed term), Department of History of Northern Europe, Petrozavodsk University, Russia. 2008 Contract Lecturer, Russian-Finnish Cross-Border University. 2006–2009 Lecturer, Department of History of Northern Europe, Petrozavodsk University. 2003–2004 Instructor, Department of History, Karelian State Pedagogical College, Russia. EDUCATION 2016 Ph.D. in History. Department of History, University of British Columbia. 2006 Candidate of Sciences in History. Faculty of History, Petrozavodsk University. 2002 Diploma in Russian and English. Faculty of Philology, Petrozavodsk University. FELLOWSHIPS, GRANTS, AND AWARDS 2020 Aleksanteri Institute Visiting Fellowship, University of Helsinki. 2019 Visiting Assistant Professor, summer term, History Department, University of British Columbia. 2019 Cougar Initiative to Engage Grant, University of Houston. 2018 Research Fellowship, German Historical Institute in Moscow, Russia. 2017 New Faculty Research Award, University of Houston. 2016 Banting Postdoctoral Fellowship. 2016 Davis Center for Russian and Eurasian Studies Postdoctoral Fellowship, Harvard University (declined). 2016 Social Sciences and Humanities Research Council of Canada Postdoctoral Fellowship (declined). 2015 Visiting Lecturer, University of Eastern Finland, Joensuu. 2015 Margaret A. Ormsby Memorial Scholarship. 2015 Teaching Mobility Grant, Kone Foundation, Finland. 2014 Visiting Scholar, St. Petersburg Institute of History of Natural Science and Technology of the Russian Academy of Sciences, St. -

Karelia, Russia Karelia Is Located in the Northwestern Part of the Russian Federation, in an Intermediate Position Between the Basins of White and Baltic Seas
Destination: Karelia, Russia Karelia is located in the northwestern part of the Russian Federation, in an intermediate position between the basins of White and Baltic seas. The greater part of the territory of the Republic of Karelia (148,000 km ² or 85%) is the public forest reserves. It has more than 60,000 lakes. Lakes and wetlands contain about 2000 km ² freshwater of excellent quality. Lake Ladoga and Lake Onega are the largest lakes in Europe. There are fifty minerals in Karelia, located in more than 400 fields and metal layers. Natural resources of the Republic include, among others, iron ore and diamonds. What to visit : Petrozavodsk - the capital of Karelia. It is located on the western shore of Lake Onega, 698 km north of Moscow. Its population is 269.000 inhabitants. Petrozavodsk was founded in 1703 under the name of Petrovskaia Sloboda. Peter the Great had built a foundry for the manufacture of cannons and anchors to provide a war effort during the Great Northern War. This factory, named Petrovskiy zavod or "Factory of Peter”, gave its name to the city. What to visit : Kizhi - Kizhi Island in Lake Onega presents an open-air museum of Wooden architecture. The whole island is a World Heritage site announced by UNESCO in 1990. The island is 7 km long and 500 m wide. Kizhi is world famous for its churchyard (pogost) with two churches of the eighteenth century and an octagonal bell tower surrounded by an enclosure, all built of wood. There is also the unique Church of the Transfiguration, with a pyramid inside, made of 22 frames, decorated with silver bulbs. -
GORGEOUS KARELIA With
GORGEOUS KARELIA with 1 The tours presented in this brochure aim to country had been for centuries populated by the introduce customers to the unique beauty and Russian speaking Pomors – proud independent folk culture of the area stretching between the southern that were at the frontier of the survival of the settled coast of the White Sea and the Ladoga Lake. civilization against the harshness of the nature and Karelia is an ancient land that received her name paid allegiance only to God and their ancestors. from Karelians – Finno-Ugric people that settled in that area since prehistoric times. Throughout the For its sheer territory size (half of that of Germany) history the area was disputed between the Novgorod Karelia is quite sparsely populated, making it in fact Republic (later incorporated into Russian Empire) the biggest natural reserve in Europe. The and Kingdom of Sweden. In spite of being Orthodox environment of this part of Russia is very green and Christians the Karelians preserved unique feel of lavish in the summer and rather stern in the winter, Finno-Ugric culture, somehow similar to their but even in the cold time of the year it has its own Finnish cousins across the border. East of the unique kind of beauty. Fresh water lakes and rivers numbered in tens of thousands interlace with the dense taiga pine forest and rocky outcrops. Wherever you are in Karelia you never too far from a river or lake. Large deposits of granite and other building stones give the shores of Karelian lakes a uniquely romantic appearance. -
Report on the Charitable Activity of the Elena and Gennady Timchenko Foundation Timchenko Elena & Gennady Timchenko Foundation Foundation Contents
2015 REPORT ON THE CHARITABLE ACTIVITY OF THE ELENA AND GENNADY TIMCHENKO FOUNDATION TIMCHENKO ELENA & GENNADY TIMCHENKO FOUNDATION FOUNDATION CONTENTS Message from Elena and Gennady Timchenko .....................4 Working with the Foundation.............................................109 Message from Xenia Frank .....................................................6 Selecting grant recipients .............................................. 110 Message from Maria Morozova .............................................8 Open grant competitions ............................................... 110 The Foundation’s mission statement and values ................10 Non-competitive support ................................................111 Work programme ..................................................................11 Duration of project support ............................................111 5 years of work – facts and results ...................................... 12 Programme evaluation system ...........................................111 Key results in 2015 .............................................................. 16 Risk management ...............................................................112 Interaction with stakeholders .............................................112 Working with enquiries from the public .........................112 THE OLDER GENERATION PROGRAMME .......................18 Working with regional agents .........................................113 Society for all Ages Focus Area ............................................24 -

Russia 2019 Human Rights Report
RUSSIA 2019 HUMAN RIGHTS REPORT EXECUTIVE SUMMARY The Russian Federation has a highly centralized, authoritarian political system dominated by President Vladimir Putin. The bicameral Federal Assembly consists of a directly elected lower house (State Duma) and an appointed upper house (Federation Council), both of which lack independence from the executive. The 2016 State Duma elections and the 2018 presidential election were marked by accusations of government interference and manipulation of the electoral process, including the exclusion of meaningful opposition candidates. The Ministry of Internal Affairs, the Federal Security Service (FSB), the Investigative Committee, the Office of the Prosecutor General, and the National Guard are responsible for law enforcement. The FSB is responsible for state security, counterintelligence, and counterterrorism as well as for fighting organized crime and corruption. The national police force, under the Ministry of Internal Affairs, is responsible for combating all crime. The National Guard assists the FSB Border Guard Service in securing borders, administers gun control, combats terrorism and organized crime, protects public order, and guards important state facilities. The National Guard also participates in armed defense of the country’s territory in coordination with Ministry of Defense forces. Except in rare cases, security forces generally reported to civilian authorities. National-level civilian authorities, however, had, at best, limited control over security forces in the Republic of Chechnya, which were accountable only to the head of Chechnya, Ramzan Kadyrov. The country’s occupation and purported annexation of Ukraine’s Crimean Peninsula continued to affect the human rights situation there significantly and negatively. The Russian government continued to arm, train, lead, and fight alongside Russia-led forces in eastern Ukraine.