2006 AAZV Proceedings.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE CROFTER, December 20131
1 THE CROFTER, DECEMBER 20131 Scottish Crofting Federation THE CROFTER rooted in our communities The journal of the Scottish Crofting Federation, the only member-led organisation dedicated to the promotion of crofting and the largest association of small-scale food producers in the UK DECEMBER 2013 Number 101 Did the 2010 Questions on Scottish Act equalise availability of Government land sale policy OLLOWING THE Scottish Government's expressing an interest in the land, when, as crofting grants? decision to withdraw part of its Rosal the sales particulars were keen to point out, Fforest estate in Sutherland from communities were cleared from this land and open market sale after public criticism, the it is a deserted wilderness. ROFTING-SPECIFIC grants, SCF asked the government to examine its Putting this land on the market in this way is namely CCAGS and CHGS, policies on the sale of public land, community simply perpetuating a system of land ownership were expected to be extended to ownership and the creation of new crofts. concentrated into few hands, a system the C SCF chair Derek Flyn believes the Rosal Scottish people want to see changed.” owner-occupier crofters by virtue of the Crofting Reform (Scotland) Act 2010. case demonstrates some of the problems He continued “A great deal of effort and The former scheme provides grants caused by the manner in which the Forestry public money has been invested in reforming towards agricultural developments such Commission conducts the process of land crofting. The SG has pledged its commitment as sheds, barns, fencing and other sale. He said: “There is no surprise that to the crofting system and has legislated to permanent improvements; the latter local communities did not come forward Continued on page 3 towards the building of a croft house. -

Picrotoxin-Like Channel Blockers of GABAA Receptors
COMMENTARY Picrotoxin-like channel blockers of GABAA receptors Richard W. Olsen* Department of Molecular and Medical Pharmacology, Geffen School of Medicine, University of California, Los Angeles, CA 90095-1735 icrotoxin (PTX) is the prototypic vous system. Instead of an acetylcholine antagonist of GABAA receptors (ACh) target, the cage convulsants are (GABARs), the primary media- noncompetitive GABAR antagonists act- tors of inhibitory neurotransmis- ing at the PTX site: they inhibit GABAR Psion (rapid and tonic) in the nervous currents and synapses in mammalian neu- system. Picrotoxinin (Fig. 1A), the active rons and inhibit [3H]dihydropicrotoxinin ingredient in this plant convulsant, struc- binding to GABAR sites in brain mem- turally does not resemble GABA, a sim- branes (7, 9). A potent example, t-butyl ple, small amino acid, but it is a polycylic bicyclophosphorothionate, is a major re- compound with no nitrogen atom. The search tool used to assay GABARs by compound somehow prevents ion flow radio-ligand binding (10). through the chloride channel activated by This drug target appears to be the site GABA in the GABAR, a member of the of action of the experimental convulsant cys-loop, ligand-gated ion channel super- pentylenetetrazol (1, 4) and numerous family. Unlike the competitive GABAR polychlorinated hydrocarbon insecticides, antagonist bicuculline, PTX is clearly a including dieldrin, lindane, and fipronil, noncompetitive antagonist (NCA), acting compounds that have been applied in not at the GABA recognition site but per- huge amounts to the environment with haps within the ion channel. Thus PTX major agricultural economic impact (2). ͞ appears to be an excellent example of al- Some of the other potent toxicants insec- losteric modulation, which is extremely ticides were also radiolabeled and used to important in protein function in general characterize receptor action, allowing and especially for GABAR (1). -
Qrno. 1 2 3 4 5 6 7 1 CP 2903 77 100 0 Cfcl3
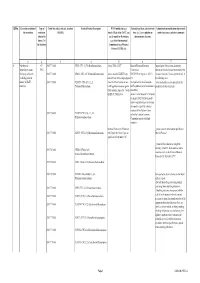
QRNo. General description of Type of Tariff line code(s) affected, based on Detailed Product Description WTO Justification (e.g. National legal basis and entry into Administration, modification of previously the restriction restriction HS(2012) Article XX(g) of the GATT, etc.) force (i.e. Law, regulation or notified measures, and other comments (Symbol in and Grounds for Restriction, administrative decision) Annex 2 of e.g., Other International the Decision) Commitments (e.g. Montreal Protocol, CITES, etc) 12 3 4 5 6 7 1 Prohibition to CP 2903 77 100 0 CFCl3 (CFC-11) Trichlorofluoromethane Article XX(h) GATT Board of Eurasian Economic Import/export of these ozone destroying import/export ozone CP-X Commission substances from/to the customs territory of the destroying substances 2903 77 200 0 CF2Cl2 (CFC-12) Dichlorodifluoromethane Article 46 of the EAEU Treaty DECISION on August 16, 2012 N Eurasian Economic Union is permitted only in (excluding goods in dated 29 may 2014 and paragraphs 134 the following cases: transit) (all EAEU 2903 77 300 0 C2F3Cl3 (CFC-113) 1,1,2- 4 and 37 of the Protocol on non- On legal acts in the field of non- _to be used solely as a raw material for the countries) Trichlorotrifluoroethane tariff regulation measures against tariff regulation (as last amended at 2 production of other chemicals; third countries Annex No. 7 to the June 2016) EAEU of 29 May 2014 Annex 1 to the Decision N 134 dated 16 August 2012 Unit list of goods subject to prohibitions or restrictions on import or export by countries- members of the -

Effects of Parasites on Marine Maniacs
EFFECTS OF PARASITES ON MARINE MANIACS JOSEPH R. GERACI and DAVID J. ST.AUBIN Department of Pathology Ontario Veterinary College University of Guefph Guelph, Ontario Canada INTRODUCTION Parasites of marine mammals have been the focus of numerous reports dealing with taxonomy, distribution and ecology (Defyamure, 1955). Descriptions of associated tissue damage are also available, with attempts to link severity of disease with morbidity and mortality of individuals and populations. This paper is not intended to duplicate that Iiterature. Instead we focus on those organisms which we perceive to be pathogenic, while tempering some of the more exaggerated int~~retations. We deal with life cycles by emphasizing unusual adap~t~ons of selected organisms, and have neces- sarily limited our selection of the literature to highlight that theme. For this discussion we address the parasites of cetaceans---baleen whales (mysticetes), and toothed whales, dolphins and porpoises (odon- tocetes): pinnipeds-true seals (phocidsf, fur seals and sea Iions (otariidsf and walruses (adobenids); sirenians~anatees and dugongs, and the djminutive sea otter. ECTOPARASITES We use the term “ectoparasite’” loosely, when referring to organisms ranging from algae to fish which somehow cling to the surface of a marine mammal, and whose mode of attachment, feeding behavior, and relationship with the host or transport animal are sufficiently obscure that the term parasite cannot be excluded. What is clear is that these organisms damage the integument in some way. For example: a whale entering the coid waters of the Antarctic can acquire a yelIow film over its body. Blue whales so discoiored are known as “sulfur bottoms”. -
Fluorides in the Environment
Color profile: Disabled Composite 150 lpi at 45 degrees Fluorides in the Environment A4662 - Weinstein - Vouchers - VP10 #K.prn 1 Z:\Customer\CABI\A4642 - Weinstein\A4662 - Weinstein - Vouchers - VP10 #K.vp Monday, November 10, 2003 3:35:50 PM Color profile: Disabled Composite 150 lpi at 45 degrees A4662 - Weinstein - Vouchers - VP10 #K.prn 2 Z:\Customer\CABI\A4642 - Weinstein\A4662 - Weinstein - Vouchers - VP10 #K.vp Monday, November 10, 2003 3:35:50 PM Color profile: Disabled Composite 150 lpi at 45 degrees Fluorides in the Environment Effects on Plants and Animals Professor L.H. Weinstein Boyce Thompson Institute for Plant Research Tower Road Ithaca NY 14853 USA and Professor A. Davison School of Biology Ridley Building University of Newcastle Newcastle upon Tyne NE1 7RU UK CABI Publishing A4662 - Weinstein - Vouchers - VP10 #K.prn 3 Z:\Customer\CABI\A4642 - Weinstein\A4662 - Weinstein - Vouchers - VP10 #K.vp Monday, November 10, 2003 3:35:51 PM Color profile: Disabled Composite 150 lpi at 45 degrees CABI Publishing is a division of CAB International CABI Publishing CABI Publishing CAB International 875 Massachusetts Avenue Wallingford 7th Floor Oxon OX10 8DE Cambridge, MA 02139 UK USA Tel: +44 (0)1491 832111 Tel: +1 617 395 4056 Fax: +44 (0)1491 833508 Fax: +1 617 354 6875 E-mail: [email protected] E-mail: [email protected] Web site: www.cabi-publishing.org ©L.H. Weinstein and A. Davison 2004. All rights reserved. No part of this publication may be reproduced in any form or by any means, electronically, mechanically, by photocopying, recording or otherwise, without the prior permission of the copyright owners. -

Proceedings of the Helminthological Society of Washington 51(2) 1984
Volume 51 July 1984 PROCEEDINGS ^ of of Washington '- f, V-i -: ;fx A semiannual journal of research devoted to Helminthohgy and all branches of Parasitology Supported in part by the -•>"""- v, H. Ransom Memorial 'Tryst Fund : CONTENTS -j<:'.:,! •</••• VV V,:'I,,--.. Y~v MEASURES, LENA N., AND Roy C. ANDERSON. Hybridization of Obeliscoides cuniculi r\ XGraybill, 1923) Graybill, ,1924 jand Obeliscoides,cuniculi multistriatus Measures and Anderson, 1983 .........:....... .., :....„......!"......... _ x. iXJ-v- 179 YATES, JON A., AND ROBERT C. LOWRIE, JR. Development of Yatesia hydrochoerus "•! (Nematoda: Filarioidea) to the Infective Stage in-Ixqdid Ticks r... 187 HUIZINGA, HARRY W., AND WILLARD O. GRANATH, JR. -Seasonal ^prevalence of. Chandlerellaquiscali (Onehocercidae: Filarioidea) in Braih, of the Common Grackle " '~. (Quiscdlus quisculd versicolor) '.'.. ;:,„..;.......„.;....• :..: „'.:„.'.J_^.4-~-~-~-<-.ii -, **-. 191 ^PLATT, THOMAS R. Evolution of the Elaphostrongylinae (Nematoda: Metastrongy- X. lojdfea: Protostrongylidae) Parasites of Cervids,(Mammalia) ...,., v.. 196 PLATT, THOMAS R., AND W. JM. SAMUEL. Modex of Entry of First-Stage Larvae ofr _^ ^ Parelaphostrongylus odocoilei^Nematoda: vMefastrongyloidea) into Four Species of Terrestrial Gastropods .....:;.. ....^:...... ./:... .; _.... ..,.....;. .-: 205 THRELFALL, WILLIAM, AND JUAN CARVAJAL. Heliconema pjammobatidus sp. n. (Nematoda: Physalbpteridae) from a Skate,> Psammobatis lima (Chondrichthyes: ; ''•• \^ Rajidae), Taken in Chile _... .„ ;,.....„.......„..,.......;. ,...^.J::...^..,....:.....~L.:....., -

Cha Kuna Taiteit Un Chitan Dalam Menit
CHA KUNA TAITEIT US009943590B2UN CHITAN DALAM MENIT (12 ) United States Patent ( 10 ) Patent No. : US 9 ,943 ,590 B2 Harn , Jr . et al. (45 ) Date of Patent: Apr . 17 , 2018 (54 ) USE OF LISTERIA VACCINE VECTORS TO 5 ,679 ,647 A 10 / 1997 Carson et al. 5 ,681 , 570 A 10 / 1997 Yang et al . REVERSE VACCINE UNRESPONSIVENESS 5 , 736 , 524 A 4 / 1998 Content et al. IN PARASITICALLY INFECTED 5 ,739 , 118 A 4 / 1998 Carrano et al . INDIVIDUALS 5 , 804 , 566 A 9 / 1998 Carson et al. 5 , 824 ,538 A 10 / 1998 Branstrom et al. (71 ) Applicants : The Trustees of the University of 5 ,830 ,702 A 11 / 1998 Portnoy et al . Pennsylvania , Philadelphia , PA (US ) ; 5 , 858 , 682 A 1 / 1999 Gruenwald et al. 5 , 922 , 583 A 7 / 1999 Morsey et al. University of Georgia Research 5 , 922 ,687 A 7 / 1999 Mann et al . Foundation , Inc. , Athens, GA (US ) 6 ,004 , 815 A 12/ 1999 Portnoy et al. 6 ,015 , 567 A 1 /2000 Hudziak et al. (72 ) Inventors: Donald A . Harn , Jr. , Athens, GA (US ) ; 6 ,017 ,705 A 1 / 2000 Lurquin et al. Yvonne Paterson , Philadelphia , PA 6 ,051 , 237 A 4 / 2000 Paterson et al . 6 ,099 , 848 A 8 / 2000 Frankel et al . (US ) ; Lisa McEwen , Athens, GA (US ) 6 , 287 , 556 B1 9 / 2001 Portnoy et al. 6 , 306 , 404 B1 10 /2001 LaPosta et al . ( 73 ) Assignees : The Trustees of the University of 6 ,329 ,511 B1 12 /2001 Vasquez et al. Pennsylvania , Philadelphia , PA (US ) ; 6 , 479 , 258 B1 11/ 2002 Short University of Georgia Research 6 , 504 , 020 B1 1 / 2003 Frankel et al . -

RHS Supreme Champions 2017
RHASS MAGAZINE SUMMER 2017 What a ShowStoppER! RHS Supreme Champions 2017: 8-page pullout + Post-Show Overview + New Members’ Area Survey + Technical Innovation Awards + Exhibitors Stories + RHASS Directors and Presidential Team 2017-18 + RHET Latest News + RHC Events to look out for RHASS • Society Magazine • Summer 2017 | 1 6 Contents COVER STORIES 6 Post-Show Overview 21 RHET News 24 RHC Events 13 26 RHASS Directors and Officials 2017 28 RHASS Presidential Team FEATURES 3 Welcome - Alan Laidlaw, Chief Executive 4 News Update 6 Royal Highland Show - Post-Show Analysis 21 8 Case Studies - “What the Royal Highland Show means to me...” 10 Technical Innovation Awards 13 Supreme Champions 2017 Pullout 21 Royal Highland Education Trust News 24 Royal Highland Centre Events 30 Members’ Feedback 24 RHASS MAGAZINE SUMMER 2017 CONTACT DETAILS: RHASS Society magazine Written & produced by is published by: The Royal Highland and Represent Agricultural Society of Scotland, Royal Highland 57 Calton Road, Centre, Ingliston, Edinburgh EH28 8NB Edinburgh EH8 8FJ Tel: (0131) 335 6200 [email protected] What a Email: [email protected] ShowStoppER! Web: www.rhass.org.uk RHS Supreme Champions 2017: 8-page pullout + Post-Show Overview + New Members’ Area Survey + Technical Innovation Awards + Exhibitors Stories Charity No. SC4561 + RHASS Directors and Presidential Team 2017-18 + RHET Latest News + RHC Events to look out for RHASS • Society Magazine • Summer 2017 | 1 2 | RHASS • Society Magazine • Summer 2017 Over 8,000 members attended the Show on each of the four days Welcome from RHASS Chief Executive Alan Laidlaw t is with pride that I reflect on my first Show as Chief Executive. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Register of GDP Sites 2019
Register of GDP Sites 2019 Updated 16 August 2019 There are other sites authorised for wholesale dealing of veterinary medicinal products which do not appear on this register. These sites wholesale deal in both human and veterinary medicinal products and can be found on the MHRA section of GOV.UK: https://www.gov.uk/government/publications/human-and-vetinary-medicines- register-of-licensed-wholesale-distribution-sites-december-2014 Register of Authorised Wholesale Dealer Sites Authorisation Holder: WDA33618 ABBEYVET LLP 310 CHESTER ROAD, HARTFORD, NORTHWICH, CHESHIRE, CW8 2AB SITE ID: S0415 ABBEYVET LLP 310 CHESTER ROAD, HARTFORD, NORTHWICH, CHESHIRE, CW8 2AB SITE ID: S0010 ABBEYVET LLP SHERBURN ENTERPRISE PARK, SHERBURN IN ELMET, LEEDS, WEST YORKSHIRE, LS25 6NB Authorisation Holder: WDA8599 AGRIHEALTH (N.I.) LIMITED 9 SILVERWOOD INDUSTRIAL AREA, SILVERWOOD ROAD, LURGAN, CRAIGAVON, COUNTY ARMAGH, BT66 6LN SITE ID: S0015 AGRIHEALTH (N.I.) LIMITED 9 SILVERWOOD INDUSTRIAL AREA, SILVERWOOD ROAD, LURGAN, CRAIGAVON, COUNTY ARMAGH, BT66 6LN Authorisation Holder: WDA5097 ALBAVET LIMITED BUSINESS INCUBATOR OFFICE 21, MYREGORMIE PLACE, MITCHELSTON INDUSTRIAL ESTATE, KIRKCALDY, FIFE, KY1 3NA SITE ID: S0456 ALBAVET LIMITED BUSINESS INCUBATOR OFFICE 21, MYREGORMIE PLACE, MITCHELSTON INDUSTRIAL ESTATE, KIRKCALDY, FIFE, KY1 3NA SITE ID: S0525 CVS GROUP PLC CVS HOUSE, OWEN ROAD, DISS, NORFOLK, IP22 4ER Authorisation Holder: WDA5030 ALBERT E JAMES & SON LIMITED BARROW MILL BARROW STREET, BARROW GURNEY, BRISTOL, BS48 3RU SITE ID: S0303 ALBERT E JAMES & -

The Helminthological Society of Washinqton I
. Volume 46 1979 Number 2 PROCEEDINGS The Helminthological Society %Hi.-s'^ k •''"v-'.'."'/..^Vi-":W-• — • '.'V ' ;>~>: vf-; • ' ' / '••-!' . • '.' -V- o<•' fA • WashinQto" , ' •- V ' ,• -. " ' <- < 'y' : n I •;.T'''-;«-''•••.'/ v''.•'••/••'; •;•-.-•• : ' . -•" 3 •/"-:•-:•-• ..,!>.>>, • >; A semiannual: journal Jof research devoted to Helminthology and a// branches of Paras/fo/ogy ,I ^Supported in part by<the / ^ ^ ;>"' JBrayton H. Ransom^Memorial TrustJiund /^ v ''•',''•'•- '-- ^ I/ •'/"! '' " '''-'• ' • '' * ' •/ -"."'• Subscription $i;iB.OO a Volume; foreign, $1 ?1QO /' rv 'I, > ->\ ., W./JR. Polypocephalus sp. (CeModa; Lecanieephalidae): ADescrip- / ^xtion, of .Tentaculo-PJerocercoids .'from Bay Scallops of the Northeastern Gulf ( ,:. ••-,' X)f Mexico^-— u-':..-., ____ :-i>-.— /— ,-v-— -— ;---- ^i--l-L4^,- _____ —.—.;—— -.u <165 r CAREER, GEORGE^ J.^ANDKENNETI^: C, CORKUM. 'Life jpycle (Studies of Three Di- .:•';' genetic; Trpmatodes, Including /Descriptions of Two New' Species (Digenea: ' r vCryptpgonirnidae) ,^.: _____ --—cr? ..... ______ v-^---^---<lw--t->-7----^--'r-- ___ ~Lf. \8 . ; HAXHA WAY, RONALD P, The Morphology of Crystalline Inclusions in, Primary Qo: ^ - r ',{••' cylesfafiAspidogaJter conchicola von Baer,;1827((Trematoda: A^pidobpthria)— : ' 201 HAYUNGA, EUGENE ,G. (The Structure and Function of the GlaJids1! of .. Three .Carypphyllid T;ape\y,orms_Jr-_-_.--_--.r-_t_:_.l..r ____ ^._ ______ ^..—.^— —....: rJ7l ' KAYT0N , ROBERT J . , PELANE C. I^RITSKY, AND RICHARD C. TbaiAS. Rhabdochona /• ;A ; ycfitostomi sp. n. (Nematoifja: Rhaibdochonidae)"from the-Intestine of Catdstomusi ' 'i -<•'• ' spp.XGatostpmjdae)— ^ilL.^—:-;..-L_y— 1..:^^-_— -L.iv'-- ___ -—- ?~~ -~—:- — -^— '— -,--- X '--224- -: /McLoUGHON, D. K. AND M:JB. CHUTE: \ tenellq.in Chickens:, Resistance to y a Mixture .of Suifadimethoxine and'Ormetpprim (Rofenaid) ,___ _ ... .. ......... ^...j.. , 265 , M, C.-AND RV A;. KHAN. Taxonomy, Biology, and Occurrence of Some " Manhe>Lee^ches in 'Newfoundland Waters-i-^-\---il.^ , R. -

STUDIES on the LIFE HISTORY of RICTULARIA COLORADENSIS HALL, 1916 (NEMATODA: THELAZIIDAE), a PARASITE of Phtomyscus LEUCOPPS NOVEBORACENSIS (FISCHER)
STUDIES ON THE LIFE HISTORY OF RICTULARIA COLORADENSIS HALL, 1916 (NEMATODA: THELAZIIDAE), A PARASITE OF PHtoMYSCUS LEUCOPPS NOVEBORACENSIS (FISCHER) DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio S tate U niversity Bbr VERNON HARVEY OSWALD, B. S ., 11. A. ***** The Ohio State University 1956 Approved by: f Department of Zoology and [ y Entomology ACKNOWLEDGMENTS This study was accomplished through the direct and indirect assistance of many of the faculty members, fellow students, and technical personnel in the Department of Zoology and Entomology of The Ohio State University. The author wishes to thank Dr. Josef N. Knull and Mr. Richard D. Alexander of the Department of Zoology and Entomology for identifying ground beetles and field crickets, respec tively, which were used in th is study. Dr. Edward Thomas of the Ohio State Museum, Columbus, kindly identified wood roaches and camel crickets for the author. Special thanks also go to Mr. Donal (3. Myer for help in collecting material and to Mr. John L. Crites who was concurrently working on the life history of Cruzla americana and who offered many suggestions on techniques which were used by the author. Dr. William H. Coil, a Muellhaupt Scholar in the Depart ment, took an active part in collecting material and is also respon sible for the photomicrographs included in this work. Lastly, the writer wishes to acknowledge the many helpful suggestions and c riti cisms given hy his adviser, Dr. Joseph N. Miller of the Department of Zoology and Entosology. - i i TABLE OF CONTENTS INTRODUCTION ..........................................................................................................